BLOOD GROUPS
advertisement

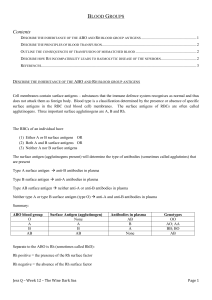
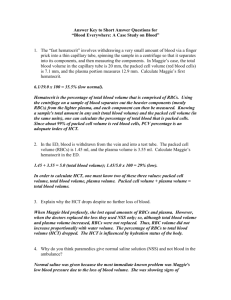
BLOOD GROUPS Blood groups are classified according to antigens on the membrane of RBCs called “Agglutinogen”, which are glycoprotein. The plasma may contain antibodies called agglutinins. Two main systems of antigens and hence grouping are the ABO and Rh systems. ABO system 1- Group (A): 40% of population, RBCs has A Agglutinogens and the plasma contains anti B antibodies. It may be homozygous (AA) or heterozygous (AO). 2- Group (B): 10% of population, RBCs have B antigen and plasma contain anti A it may be homozygous (BB) or heterozygous (BO). ABO system to be continued 3- Group (AB): 5% of population, RBCs has both agglutinogens A + B, the plasma does not contain agglutinins. 4- Group (O): 45% of population, RBCs has no agglutinogens, but the plasma contains both agglutinins Anti A + Anti B. Rh System People are classified according to the presence or absence of Rhesus antigens (most common type D) into Rh+ve with D antigen 85% and Rh-ve without D antigen 15%. Importance of Blood Groups: 1-Medicolegal importance: Disputed parenthood. Regarding blood group inheritance 2 antigens are inherited from both father and mother. These antigens determine the group. The A + B antigens are dominant while the O one is recessive. In group A (phenotype A) the genotype may be AA or AO. In Group B may be (BB or BO). In Group AB and O (AB or O). Blood grouping is a good -ve test in disputed parenthood 2- Blood Transfusion If transfused blood is incompatible usually the donor RBCs are agglutinated by recipient plasma as the donor’s serum is diluted in recipient blood. - Group O: is the universal donor (no agglutinogens). - Group AB: is the universal recipient (no agglutinins). 3-). Importance of Rh factor: (Erythroblastosis Fetalis) The disease occurs when an Rhve mother carries an Rh+ve fetus, small amounts of fetal blood leak into the maternal circulation at the time of delivery, thus the mother will produce Anti D agglutinins. (Erythroblastosis Fetalis) to be cont. During the next pregnancy the mother agglutinins cross the placenta (IgG) to an Rh+ve fetus causing hemolysis of fetal RBCs and may lead to: Anemia of fetus Death of fetus. Jaundice with deposition of bile pigment in the basal ganglia (kernicterus syndrome) as the blood brain barrier is not developed yet (Erythroblastosis Fetalis). (Erythroblastosis Fetalis) to be cont. The first baby (Rh+ve) is affected in case of maternal sensitization by: -Previous Rh +ve blood transfusion. - If the baby was born alive should be treated by exchange blood transfusion with Rh -ve group O blood. (Erythroblastosis Fetalis) to be cont. Fetal-Maternal hemorrhage during pregnancy. This disease can be prevented by avoiding Rh+ve blood transfusion to Rh-ve females, and if pregnancy and labor happened an anti-D antibodies are given to neutralize the D antigens of the Rh +ve fetal cells and prevent sensitization of the mother. BLOOD TRANSFUSION Indications If the whole blood or any of its components is deficient blood transfusion is indicated as in case of; - Acute hemorrhage. - Severe anemia. - Agranulocytosis. - Thrombocytopenia. - Hemophilia. However, if one element only is deficient it is preferable to give this particular element e.g. packed RBCs and human plasma transfusions. Precautions - Blood should be compatible (ABO and Rh) assured by cross matching test. - Blood should be free from contamination. - Blood should be free from blood born diseases. - Blood should be fresh (less than 2 weeks storage). - High hemoglobin content. Precautions to be cont. Blood is stored at 4oC and added to: - Sodium citrate as an anticoagulant. - Dextrose as a nutrient for cells. - Citric acid to reduce the pH. - Storage lead to decrease in platelets, coagulation factors VII, VIII, IX and dextrose, while there is increase in lactic acid content, K and haemoglobin released from haemolysed RBCs. Complications The donor may suffer from anemia in repeated donation and shock in excessive volume donation. The recipient may suffer from: 1- Mechanical effect: - Air or fat embolism. - Dislodgement of a thrombus. 2- Infective complications: E.g. infective hepatitis, AIDS or Malaria. 3- Physiological complications: - Overloading in excessive transfusion leading to heart failure. - Pyrogenic reaction i.e. fevers. 4- Incompatibility complications Agglutinated RBCs may block small vessels causing severe pain, or haemolysis follows i.e., liberation of hemoglobin, K+ and toxins into plasma. a) Hemoglobin liberation will cause: - increased blood viscosity leading to heart failure. - conversion into bile causing jaundice. - precipitate in renal tubules as acid haematin causing renal failure. - hypoxia. b) K+ causes arrhythmia. c) Toxic substances cause powerful vasoconstriction of renal vessels causing acute renal failure.