Physiology Ch 70 p837-841 [4-25
advertisement
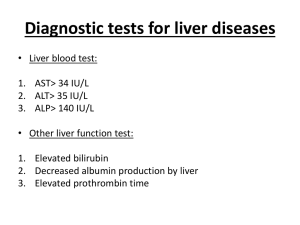
Physiology Ch 70 p837-841 The Liver as an Organ Anatomy of the Liver – liver is largest organ (2% of body weight), functional unit is lobule, and the live has 50000-100000 lobules -lobule surrounds a central vein that empties into hepatic veins and IVC -lobule composed of cellular plates radiating from central vein (each plate 2 cells thick, and lies between bile canaliculi that empty into bile ducts) -Portal venules are found in the septa that receive blood from venous outflow of GI tract through portal vein -venules flow into branching hepatic sinusoids laying between hepatic plates and vein -Hepatic arterioles also present in interlobular septa to supply arterial blood to septal tissues -sinusoids lined by two other cell types: endothelial cells and KUPFFER CELLS, which are resident macrophages capable of phagocytizing bacteria -endothelial lining of sinusoids has extremely large pores -under this lining between endothelial cells and hepatic cells, are narrow tissue spaces called spaces of disse or perisinusoidal spaces to connect lymphatic vessels in interlobular septa (excess fluid removed in spaces of Disse through lymphatics) Hepatic Vascular and Lymph Systems – Blood flows through liver from portal vein and hepatic artery – liver has high blood flow and low vascular resistance (27% of resting cardiac output in liver), very small pressure difference between IVC and hepatic vein = low resistance through sinusoids -Cirrhosis of the liver increases resistance to blood flow – when liver parenchymal cells are destroyed, they are replaced with fibrous tissue that eventually contracts around vessels to impede flow of blood (cirrhosis) -Results from chronic alcoholism or excess fat accumulation (nonalcoholic steatohepatitis (NASH) -Less severe form is nonalcoholic fatty liver disease (NAFLD) is most common liver disease Cirrhosis can follow ingestion of poisons such as CCl4, viruses, obstruction, etc.. Portal system can be blocked by large clot, causing portal hypertension Liver functions as blood reservoir – liver is expandable and large amounts of blood is stored -when high pressure in right atrium causes backpressure in liver, the liver expands and an extra 0.5-1L of blood can be stored in hepatic veins and sinuses, can happen during cardiac failure Liver has very high lymph flow – pores in hepatic sinusoids are permeable and allow passage of fluid and proteins into spaces of Disse, allowing large quantities of lymph to form -half of all lymph in body arises in liver -High hepatic vascular pressures can cause fluid transudation into abdominal cavity from liver and portal capillaries – ASCITES – when pressure in hepatic veins rises 3-7mmHg above normal, fluid begins to leak into lymph and through outer surface of liver into abdominal cavity -fluid is almost pure plasma, and sweating from the liver into abdominal cavity is called ASCITES -blockage of portal flow through liver causes high capillary pressures resulting in fluid transudation through gut wall to cause ascites Regulation of Liver Mass – liver can restore itself after hepatic loss or from hepatectomy -causes remaining lobes to enlarge and restore liver function -control of regeneration is regulated through hepatocyte growth factor (HGF) produced by mesenchymal cells in liver, as well as EGF, TNF, and IL-6 -after liver reaches normal size, TGF-B inhibits liver cell proliferation Hepatic Macrophage System Serves a Blood-Cleansing Function – blood through intestines picks up bacteria, and Kupffer cells can efficiently cleanse blood as it passes through sinusoids Metabolic Functions of Liver – liver has high rate of metabolism, sharing substrates and energy from one metabolic system to another Carbohydrate Metabolism – liver maintains glucose concentration 1. storage of glycogen (allows liver to remove excess glucose from blood, called the glucose buffer function) 2. conversion of galactose and fructose to glucose 3. gluconeogenesis (maintains blood glucose by synthesizing more of it from AA or fat 4. formation of chemical compounds from intermediate products of carb metabolism Fat Metabolism – liver undergoes: 1. Oxidation of fatty acids to supply energy for other body functions 2. Synthesis of cholesterol, phospholipids, and lipoproteins 3. Synthesis of fat from proteins and carbs -energy from fats necessitates conversion of fat into glycerol + fatty acids, and fatty acids are split by B-oxidation 2C acetyl radicals that form acetyl CoA, which can enter TCA cycle and be oxidized -B-oxidation takes place everywhere, but moreso in liver -liver doesn’t use all acetyl CoA, but converts it to acetoacetic acid and transports it to tissues -80% of cholesterol synthesized in liver is converted to bile salts secreted into bile, and remainder is transported in lipoproteins and carried to other tissues -phospholipids are synthesized by liver and transported on lipoproteins -all fat synthesis in liver occurs from carbohydrate and protein Protein Metabolism – without protein metabolism in liver, body would die 1. deamination of amino acids (required before usage for energy or conversion) 2. formation of urea for ammonia removal (ammonium toxic, can result in hepatic coma) 3. formation of plasma proteins (all plasma proteins except for gamma globulin) a. depleting plasma proteins causes liver hyperplasia 4. interconversion of AA and synthesis of other compounds from AA (all non-essential amino acids can be synthesized by the liver) a. a keto-acid is synthesized which is converted to an amino acid Liver is a storage for vitamins – liver stores vitamin A, D, and B12 Liver stores Iron as Ferritin – except for hemoglobin, iron is stored in the liver in the form of ferritin -hepatic cells contain apoferritin which combines with iron reversibly to form ferritin and stored in hepatocytes until needed elsewhere, acts as a blood-iron buffer Liver forms blood substrates for coagulation – liver forms fibrinogen, prothrombin, accelerator globulin, factor VII and other important factors -vitamin K needed for factors II, VII, IX, and X Liver removes or excretes drugs, hormones, and other substances – major route of calcium excretion is through bile, and liver alters drugs like sulfonamides, penicillin, ampicillin, erythromycin, etc… Measurement of Bilirubin in Bile is Diagnostic Tool – bile formation by liver and function of bile is important to liver; many substances are excreted in bile and eliminated in feces -bilirubin is a greenish yellow pigment which is end product of hemoglobin degradation, and provides diagnostic tool for hemolytic diseases -RBCs live for 120 days and then become fragile, after which they rupture and release hemoglobin which is phagocytized by tissue macrophages throughout the body -hemoglobin split into GLOBIN and HEME, from which iron is released and transported in blood on transferrin and a straight chain of 4 pyrrole nuclei, which is the substrate for bilirubin -first substance that is formed is biliverdin –which is reduced to free bilirubin, also called unconjugated bilirubin, gradually released from macrophages into plasma -unconjugated bilirubin absorbed through hepatocytes and conjugates with glucuronic acid bilirubin glucuronide, and a little bit forms bilirubin sulfate and excreted into intestine -Formation and Fate of Urobilinogen – in intestine, half of conjugated bilirubin is converted by bacteria to urobilinogen which is highly soluble; it is reabsorbed in intestine into blood and back to liver back to gut; 5% is excreted in urin -exposure to air in urine oxidizes urobilinogen urobilin -in feces, urobilinogen stercobilin Jaundice – Extra bilirubin in extracellular fluid, is a yellowish tint to body tissues, caused by either unconjugated or conjugated bilirubin in tissues -abnormal plasma levels can be as high as 40mg/dl -skin becomes jaundiced when bilirubin rises to 3x normal above 1.5mg/dl -common causes of jaundice are (1) increased destruction of RBC with rapid bilirubin release, (2) obstruction of bile ducts or damage to liver cells so usual bilirubin can’t be excreted into GI Hemolytic Jaundice – excretory function of liver is not impaired, but RBC are hemolyzed so rapidly that hepatic cells cannot excrete bilirubin as quickly as it is formed -rate of urobilinogen in intestine in increased and excreted in urine Obstructive Jaundice – obstruction of bile ducts by gallstones or cancer, or by damage to hepatic cells during hepatitis, rate of bilirubin formation is normal, but it cannot pass from blood into intestines, and conjugated bilirubin is returned into blood or lymph -differences in unconjugated vs conjugated bilirubin in blood can determine hemolytic vs obstructive jaundice (hemolytic = unconjugated, obstructive = conjugate) -test called van den bergh reaction differentiates between the two -in total obstructive jaundice, no bilirubin is converted to urobilinogen in intestine, so urobilinogen in urine is negative, stools become clay colored -kidneys can excrete small quantities of conjugated bilirubin and not albumin-bound unconjugated bilirubin, therefore, in severe obstructive jaundice, significant conjugated bilirubin appears in urine