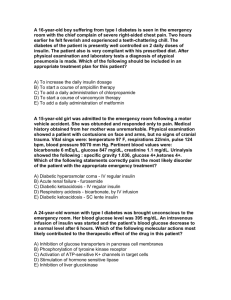
Continuous Subcutaneous Insulin Infusion Pumps in the
advertisement

Continuous Subcutaneous Insulin Infusion Pumps: Exploration of Its Presence in the Perioperative Setting Heather M. Montgomery, CRNA MSNA . Susan McMullan, CRNA MSN Major Peter Strube CRNA MSNA—Faculty Mentor Acknowledgements CSII Therapy in the Perioperative Period 2 I would like to acknowledge individuals that were essential in my professional and educational development. Without them, this thesis would not have been possible. First, I would like to recognize my mentor for this project, Major Peter Strube, CRNA, MSNA APNP ARNP. I thank you sir for your support and guidance in the development of my project. There were many instances when I wanted to bang my head up against a wall, but then you were there to keep me focused and on track. Second, Ms. Susan McMullan, CRNA, MSN is my mentor both professionally and personally. You have given me the courage to stand up to my fears and reach my professional goals. I will never be able to repay my gratitude, but please know that I thank you from the bottom of my soul for all that you have done. Finally I would like to acknowledge my family, especially my mother Maureen L. Brayman and my brother Cody M. Brayman. These two individuals were diagnosed with type I Diabetes early in childhood and continue to fight their disease several years later. I dedicate this thesis to them, so that they may continue the fight so that I can selfishly have a family for as long as possible. I love you both very much and please don’t ever give up. Table of Contents CSII Therapy in the Perioperative Period 1. List of Abbreviations 2. List of Definitions 3. Abstract 4. Introduction 5. The Pathophysiology of Type 1 Insulin Dependent Diabetes Mellitus 6. Insulin Pump Therapy Background 7. Optimizing Diabetes Treatment via Continuous Subcutaneous Insulin Infusion Therapy 8. Continuous Subcutaneous Insulin Infusion Therapy and Anesthesia Practice 9. Attempts at Research and CSII During the Perioperative Period 10. Published Opinions and Recommendations for CSII Therapy During the Perioperative Period 11. From the Source: Insulin Pump Manufacturer Guidelines 12. Conclusions and Recommendations 13. References Chapter 1: List of Abbreviations 3 CSII Therapy in the Perioperative Period BG blood glucose BUN blood urea nitrogen CHF congestive heart failure CMV cytomegalovirus CSII continuous subcutaneous insulin infusion DCCT Diabetes Control and Complications Trial DKA diabetic ketoacidosis ECG electrocardiogram HbA1c hemoglobin A1c HHNKS hyperosmolar hyperglycemic nonketotic syndrome ISBGM intensive ISF insulin sensitivity factor IV intravenous L liter(s) MDI multiple daily insulin injection ACTH adrenal corticotrophic hormone mEq/L milliequivalent(s) per liter mg milligram(s) mg/dL milligram(s) per deciliter MI myocardial infarction MRI magnetic resonance imaging NADPH nicotinamide adenine dinucleotide phosphate NPO nothing by mouth 4 CSII Therapy in the Perioperative Period PKC protein kinase C AGE advanced glycoslyation end product PVD peripheral vascular disease RAGE advanced glycoslyation end product receptor ROS reactive oxygen species SBGM self-blood glucose monitoring SDIS Stockholm Diabetes Interventional Study T1DM Type 1 diabetes mellitus T2DM Type 2 diabetes mellitus U unit(s) U/hr unit(s) per hour Chapter 2: List of Definitions 5 CSII Therapy in the Perioperative Period 6 Basal rate: a continuous supply of a drug or other compound Closed-loop device: Device that provides input with automatic output Conventional insulin therapy: Receiving no more than 2 insulin injections daily Glycoslyated: Glucose affixed to a surface (proteins, lipids, etc.) Hyperglycemia: Blood glucose level > 110 mg/dL Hyperketonia: Elevated ketones Hypoglycemia: Blood glucose level < 70 mg/dL Insulin sensitivity factor: Amount in decrease of blood glucose per 1 unit of insulin administered Intensive insulin therapy: Receiving > 3 injections of insulin per day Intraoperative period: Time from patient into the operating room to the recovery unit Open-loop device: Device provides output with manual input Perioperative period: Time frame from initial admission to entering the operating room Postoperative period: Time from admission to recovery unit to discharge Postprandial: Period of time after a meal Prandial: Period of time during a meal PubMed: an electronic search engine for health-related research articles Chapter 3: Abstract CSII Therapy in the Perioperative Period 7 Recent improved technology and supporting research for continuous subcutaneous insulin infusion (CSII) therapy has allowed great expansion of its use in the treatment of type 1 diabetes (T1DM). It is estimated that 35% of the United State's type 1 diabetics use CSII therapy and this number is expected to grow. In addition, more recent research looks to expand its use in the treatment of type 2 diabetes (T2DM). So what is an anesthesia provider to do when their patient presents with such a device? The following paper helps to explain what CSII therapy is and how its use in the perioperative period can be managed. Research on the benefits of normoglycemia and CSII therapy will be discussed. Although little research has focused on outcomes related to CSII use in the perioperative period, a few recent case studies involving CSII perioperative use have been published. Initial research has looked into CSII presence in the perioperative period and analyzed anesthesia provider’s documentation related to the device. Many hospitals have policies developed for such circumstances but not all. The following paper demonstrates that CSII therapy can be maintained in the perioperative period and is a potential tool in the perioperative management of T1DM. There are contraindications for its use, but the end result for CSII therapy management should be based on the anesthesia provider’s clinical judgment. Chapter 4: Introduction CSII Therapy in the Perioperative Period 8 The thought that the diagnosis of Type 1 insulin dependent diabetes mellitus (T1DM) was untreatable less than 100 years ago is rather baffling considering the advanced treatments available today. Treatments that are of considerable use transform T1DM from a death sentence to a manageable disease that can coincide with a high quality of life. Affecting over 1 million Americans and growing, T1DM accounts for approximately 10% of all diabetics in the United States.1(p2) These 1 million people require optimal continuous therapy not only to survive, but also to avoid the devastating complications seen in poorly treated diabetics. Proper diet and exercise are important in T1DM therapy, but the ultimate result is that patients require insulin replacement. Conventional treatment includes delivery of insulin either by subcutaneous injections or delivery of insulin via a continuous subcutaneous insulin infusion (CSII) pump. More experimental treatments are pancreas transplants, islet cell transplants and stem cell transplants.1(p10) These more unconventional treatments may provide a cure for T1DM in the future, but since they remain in juvenile stages, the risk of such transplant procedures often outweigh the benefit of conventional T1DM therapy. Because T1DM therapy is most often limited to subcutaneous delivery of insulin, strides have been made to minimize interruptions in life that T1DM often requires. Interferences in an T1DM patient include but are not limited to frequent blood glucose (BG) monitoring and the administration of insulin. The relatively new medications glargine and insulin detemir allow 24hour coverage of controlling BG levels with one injection daily. Besides improvements in pharmaceutical treatments, the improvement of technology in CSII pumps has widely expanded its use in the United States. It is estimated that 35% of T1DM patients in the US receive insulin via a CSII pump.2(p6) The number of patients receiving CSII therapy is expected to grow not CSII Therapy in the Perioperative Period 9 only because of increasing numbers of T1DM cases, but additionally, CSII ay be helpful in the treatment of insulin dependent diabetes mellitus type 2 (T2DM).3(2297) Due to its increased presence, there is a high likelihood that a patient with T1DM with CSII therapy will present in the clinical setting. Approximately 50% of T1DM patients will require surgery in their lifetime and of these patients, there is increased probability that there will be a percentage that receives CSII therapy.19 When a T1DM patient presents for surgery and it is noted that they receive CSII therapy, what is the anesthesia provider to do? Do they leave the CSII pump on or do they simply tell the patient to turn off their device prior to entering the operating room? The following paper aims to close this gap and identify what clinically is best for the patient under such circumstances and identify the significance of CSII therapy. In order to close this knowledge gap, several references were obtained by several methods. Pathophysiology texts were consulted and noted to give meaning to treating the underlying disease process. A handbook was obtained outlining CSII therapy and it’s recommendations for its use. A Pub Med search was completed over several hours using keywords such as “continuous subcutaneous insulin infusion therapy + general anesthesia”, “insulin pump therapy + perioperative period”, “CSII + surgery” among several other search engine keywords. Also, the three US CSII pump manufacturers were contacted regarding manufacture’s guidelines for use (Medtronic, Roche and Animas). The following paper is meant to be a guideline for clinical judgment in terms of a T1DM patient presenting for surgery who also happens to wear a CSII pump. The etiology of type 1 diabetes, T1DM’s potential effects on the human body, history of the CSII pump and benefits of use will be explored. Recent literature will also be presented in terms of CSII pumps and the perioperative period. In addition, two case studies that involve general anesthesia and CSII CSII Therapy in the Perioperative Period 10 pump therapy will be discussed. The goals of this thesis are of two: Anesthesia providers may become aware more comfortable with CSII therapy and are not intimidated by it’s presence on their patient presenting for surgery. CSII Therapy in the Perioperative Period 11 Chapter 5: Pathophysiology of IDDM 1 Etiology Recent literature suggests that the etiology of T1DM is not completely understood, however there is a general consensus in the scientific community that there are two factors that play a role in the cause of T1DM: A genetic predisposition and environmental influences.5 It is widely accepted that T1DM is an autoimmune response that ultimately results in the loss of insulin secondary to destruction of beta cells in the islets of Langerhans.5(p745) This autoimmune destruction is T-cell mediated and the pathophysiology is described in a two-stage process. The immune response that leads to beta cell death in the Islets of Langerhans is complex, with multiple pathways identified. Stage 1 begins with an initial insult, with autoantigens found on the surface of beta islet cells begin to circulate throughout the intravascular and lymphatic system.5(p745) These autoantigens are consumed by antigen-presenting cells, which then lead to activation of CD4+ T helper cell lymphocytes. These lymphocytes secrete interleukin 2 that leads to activation of beta cell autoantigen-specific T cytotoxic lymphocytes. T cytotoxic lymphocytes infiltrate and destroy beta cells by their use of secreting granzymes and perforins.5(p746) In addition, interferon is released from T helper lymphocytes and thus causes additional destruction of beta cells. This release of interferon continues the destructive cycle, as this process activates macrophages that secrete destructive cytokines and tumor necrosis factor adding insult to the already assailed beta cell. In summary, the destruction of beta cells result from the infiltration of lymphocytes and macrophages that lead to chronic islet inflammation (also known as “insulitits”) and eventual beta cell death.5(p746) CSII Therapy in the Perioperative Period 12 Stage 2 can be described as the increased production of beta cell autoantibodies, glutamic acid, acid decarboxylase and other cytoplasmic proteins as well.5(p747) In addition of secretion of interluekin 2, T helper cells secrete interleukin 4, which is responsible for the increased presence of B-lymphocytes. B-lymphocytes are responsible for the creation of autoantibodies. Interestingly, these antibodies can be detected in blood years before symptoms of diabetes occur. Insulin is not immune from this response, as autoantibodies against insulin have been discovered as well.5(p748) Other mechanisms that contribute to the development of IDDM 1 include the reduced presence of autoimmune mediators, such as T regulatory cells. These mediators help control the immune response. This theory is supported by evidence of a mutation in T regulatory cells found in a rare form of diabetes known as neonatal diabetes.5(p748) Over the course of time, this autoimmune response leads to a large loss of beta cells and hence insulin. C-peptide is a protein required for insulin synthesis and its presence will decrease during the destruction of beta cells. It is thought that C-peptide plays a protective role and the diminished presence of this protein contributes to additional beta cell loss.5(p748) Although it is thought that the over-reactive immune response is genetically related, there must be an initial trigger for the autoimmune response to occur. This trigger is believed to be environmental, as in an external source that is exposed to the body. The source can either be pharmaceutically sourced, nutritionally related, or pathogen sourced. Pharmaceutically, IDDM 1 has been linked to the drugs alloxan, streptozotocin, pentamidine, and Vacor. Cows milk and high levels of nitrosaminde (a food preservative) in the diet have been linked to IDDM 1 as well.5(p748) The mumps virus and coxsackivirus have been linked to IDDM 1. It is noted that CSII Therapy in the Perioperative Period 13 40% of those with congenital Rubella will eventually develop IDDM 1 . Persistent infections of cytomegalovirus (CMV) have a small link to the development of IDDM.5(p748) Disease Process of IDDM 1 Approximately 80-90% of beta cell loss must occur before hyperglycemia is manifested. Alpha cells (which are responsible for glucagon production) and beta cells are affected. There is a hormonal imbalance as glucagon is in excess of insulin. Hepatic glucose and fat metabolism is regulated by the ratio of glucagon to insulin in the portal vein. High levels of glucagon and low levels of insulin cause hyperglycemia and hyperketonemia.5(p748-749) The role of insulin includes stimulation of fat synthesis and inhibition of fat metabolism. When insulin is absent, fat metabolism is increased and as a result, there is an increase in nonesterfied fats in the liver. This leads to increased glyconeogenesis and therefore hyperglycemia and increased levels of ketone bodies via mitochondria in hepatic tissue.5(p748) Because the peripheral tissue cannot utilize these excess ketones as fast as they are produced, a drop in physiological pH occurs. The body attempts to compensate this metabolic acidosis by creating a buffer system.5(p749) This is known as diabetic ketoacidosis (DKA) and is considered an acute complication of IDDM 1. With little to no insulin, chronic hyperglycemia can lead to serious complications affecting almost every organ system. Chronic hyperglycemia can be evaluated by obtaining a serum hemoglobin A1C level (HbA1c). HbA1c is a measurement of glycoslyated hemoglobin.5(p749) As in the external environment, glucose is adhesive in nature, so it is expected that glucose molecules have a tendency to “stick” to other components physiologically, also known as glycoslyation. Glucose can attach itself to red blood cells in the blood, which is known as glycoslyated hemoglobin. In states of excess glucose, there will be an increase in the CSII Therapy in the Perioperative Period 14 three glycoslyated hemoglobins: HbA1a, HbA1b, and HbA1c. HbA1c is used as a more longterm assessment of therapy excess. Since the average lifespan of a red blood cell is 120 days, HbA1c gives a picture of average glycemic control over the past 3 months. Goal is to keep HbA1c levels as close to normal as possible, with normal values described as between 4-6%, which suggest an average BG level of 65-135 mg/dl. Elevated HbA1c levels are considered between 8 and 10% (average BG level of 205-275 mg/dl). Seriously elevated levels are deemed those 11-14% and correspond to an average BG level of 310-415 mg/dl. Studies have concluded that diabetics with HbA1c levels less than 7% (a BG average of 170 mg/dl) are 50-75% less likely to develop diabetes-related complications. Long-Term Consequences of Poor Glycemic Control in T1DM Chronic elevated BG levels can lead to damage at both the microvascular and macrovascular levels. Examples of microvascular complications include retinopathy, nephropathy and neuropathy. Examples of macrovascular damage are coronary artery disease, cerebral vascular accident and peripheral vascular disease. How this physiological damage occurs is complex and can result from multiple alterations in homeostatis. These mechanisms include alterations in the polyol pathway, the hexosamine pathyway, protein kinase C levels, nonenzymatic glycoslytion and oxidative stress. The polyol pathway is an alternative metabolic pathway that is utilized by tissues that do not require insulin for glucose uptake. These tissues include the lens of the eye, red blood cells, blood vessels and nerves. When high levels of glucose are circulating in the blood, glucose is shifted toward this pathway. Glucose is then metabolized to sorbitol via the enzyme aldose reductase. Slowly, sorbitol is then changed to fructose per sorbitol reductase. This increase in sorbitol and fructose attract water molecules to the site, thus resulting in an increased osmotic CSII Therapy in the Perioperative Period 15 pressure. This increase in osmotic pressure leads to cellular injury. In the nerves, sorbitol affects ion pumps, causes injury to Schwaan cells and interferes with nerve conduction. Red blood cells are stiffened and then become more difficult to circulate throughout the body at the microvascular level. Aldose reductase inhibitors such as epalrestat and ranirestat may help delay the onset of complications that are linked to the polyol pathway.5(p758) Protein Kinase C (PKC) is an enzyme that is activated by increased glucose levels inappropriately. Outcomes of this activation have lead to increased thickening of vascular structures, increased production of extracellular cytokines, increased permeability and increased contractility. These observations may contribute to both the micro and macrovascular complications of diabetes.5(p758-759) Nonenzymiatic glycoslyation is the non-covalent binding of gluose to proteins, lipids, and nucleic acids without the assistance of enzymes. In a chronic hyperglycemic state, glucose binds to collagen, vasculature, interstitial tissues and red blood cells thus becoming more permanent. The product of this process is known as advanced glycoslyation end product (AGE) and it’s receptor (RAGE). Both AGE and RAGE have several characteristics that cause tissue injury. These products can lead to the trapping and cross-linking of proteins such as albumin, low density lipoprotein, immunoglobulin and complement. This results in an increased thickening and permeability in blood vessels and nerves. They can also bind to cellular receptors that then release growth factors and cytokines. Increases in growth factors and cytokines result in cell proliferation in glomueruli, smooth muscle of blood vessels and exhibits a fibrous effect on collagen production. Additionally, AGE and RAGE can inactivate nitric oxide and hence a loss of vasodilatation and decreased endothelium function. AGE and RAGE have been linked to the induction of inflammation and destructive oxidative stress. The final detrimental component CSII Therapy in the Perioperative Period 16 of AGE and RAGE end products have been found to enhance coagulation with promotion of platelet adhesion and decreased fibrinolysis.5(p759) Another source of damage from hyperglycemia is the increased presence of reactive oxygen species (ROS) and oxidative stress. This increased oxidative stress leads to damage in both small and larger blood vessels. ROS is an end-product of alterations in the polyol pathway, AGE’s, decreased nitric oxide synthesis, xanthine oxidase and nicotinamide adenine dinucleotide phosphate (NADPH).5(p579) Chronic hyperglycemia cause a redirection of glucose into the hexosamine pathway. This pathway leads to the glycoslyation of many enzymes and proteins with changes in signal transduction pathways and additional oxidative stress. A source of insulin resistance and cardiovascular damage is thought to be from the attachement of N-actetylglucosamine on the residues of nuclear and cytoplasmic proteins, a direct result of activation of this pathway.5(p759) Acute Consequences of T1DM In addition to DKA mentioned previously, there are other acute complications associated with T1DM. These include hypoglycemia, Dawn Phenomenon and the Somogyi Effect. Hyperosmolar Hyperglycemic Nonketotic Syndrome (HHNKS) is an acute complication of T2DM and therefore will not be explored in this paper. Acute complications of T1DM can be immediately threatening to life and if not identified and treated accordingly, can result in severe comorbidities and mortality. Hypoglycemia is defined as a blood glucose level less than or equal to 70 mg/dL.7 In the neonate, hypoglycemia is defined at a lower level: Less than 35 mg/dL. Approximately 90% of patients with IDDM 1 experience hypoglycemia and is a result of a mismatch between insulin and carbohydrate intake, with favor towards insulin intake.5(p754) Hypoglycemia initiates a CSII Therapy in the Perioperative Period 17 sympathetic response secondary to loss of glucose to brain tissue. Although symptoms vary between patients, general consensus states that tachycardia, palpitations, tremors, pallor, acute anxiety and diaphoresis are symptoms of hypoglycemia. It is thought that the hypothalamus plays a role in initiating this response. Continued loss of glucose to the brain causes an alteration in brain kinase activity and neuron firing rates which lead to additional symptoms: Irritability, hunger, headache, seizure activity, fatigue, lack of judgment, confusion, disruption in vision, and coma. It is important to note that beta-blockers and general anesthesia can mask early symptoms of hypoglycemia since these drugs alter the sympathetic response.6(p) Treatment includes immediate restoration of blood glucose. In the awake patient, 15-20 grams of glucose be administered and to the unconscious patient 0.5-1 mg of glucagon is administered intramuscularly.7 Hypoglycemia is best avoided when the patient is properly educated about the disease process of T1DM. Frequent blood glucose monitoring and customizing BG levels for the patient being treated helps to additionally lower the risk of hypoglycemia.5,7 The Somogyi effect is an acute complication of T1DM that is associated with hypoglycemia and then rebound hyperglycemia.5(p758) This is commonly found in the pediatric population of IDDM 1 patients. This fluctuation of blood glucose levels can be dramatic and warrants a change in therapy. The Somogyi effect is best described as when hypoglycemia attempts to correct itself by initiating gluconeogenesis and glycogenolysis, thus triggering growth hormone, epinephrine, cortisol, and glucagon release. These hormones also cause an inhibition of peripheral glucose uptake, but breakdown fatty acids and proteins to produce glucose. Insulin resistance has been linked to the aforementioned hormones, which this resistance can last up to 48 hours. Factors that are linked to hyperglycemia within the Somogyi effect include excessive carbohydrate intake. It is seen after the peak of insulin injection in CSII Therapy in the Perioperative Period 18 which hypoglycemia can result and hence cause a release of the hormones that lead to rebound hyperglycemia. Ketones in the urine are often seen in Somogyi effect due to the breakdown of fatty acids and proteins. Treatment includes continuous glucose monitoring and decreasing dosages of insulin.5(p758) The dawn phenomenon is a rise in blood glucose levels without hypoglycemia. Its cause is thought to be from nocturnal release of growth hormone, which leads to the counter-regulation of glucose. An increase in the clearance of insulin may also be linked. Changing the dose of insulin and the time of its administration can help minimize dawn phenomenon. It is important to note that treating dawn phenomenon can lead to the Somogyi effect and treatment of the Somogyi effect can lead to dawn phenomenon.5(p758) Long Term Consequences of T1DM The long-term complications of T1DM greatly decrease the quality of life for these patients and can lead to premature death. As explained previously, there are numerous mechanisms how the pathophysiology of diabetes leads to these complications. Diabetic complications are divided into two categories: Microvascular and macrovascular. Endothelial thickening, thrombosis, and capillary hyperplasia lead to the microvascular complications of retinopathy, neuropathy, and nephropathy.5(p759) Chronic hyperglycemia (elevated HgbA1c) is associated with developments of these complications. Numerous studies are linked with lower HgbA1c levels and lower occurrences of these complications and vice versa.8 Macrovascular complications include coronary artery disease, cerebral vascular accident, and peripheral vascular disease. Increased inflammation and the deposit of lipoproteins on an already proliferated blood vessel contribute to these macrovascular comorbidities.5(p763) CSII Therapy in the Perioperative Period 19 Premature atherosclerosis is linked to consequences of AGE and RAGE end products and the increased presence of oxidation. As mentioned previously, several mechanisms at the cellular level are involved in the development of diabetic macrovascular complications. An interesting observation is the combination of microvascular and macrovascular complications contribute to mortality and morbidity in this population. For example, the microvascular complication of neuropathy affects the autonomic system so that the sympathetic nervous system does not respond appropriately to changes in cardiac demand. This in grouping with coronary artery disease can lead to potential for poor outcomes such as myocardial infarction and stroke. Intensive Insulin Therapy and the Decreased Prevalence of Diabetic Complications Several studies involving strict insulin therapy and conventional insulin therapy have observed patient outcomes in terms of HgbA1c levels and the development of both macrovascular and microvascular complications.8,9 “Strict” or “intensive” insulin therapy is generally defined as receiving more than three insulin injections per day or receiving CSII therapy. Intensive self-blood glucose monitoring (ISBGM) was also a part of the intensive insulin therapy, which is defined as blood glucose checks greater than four times per day. “Conventional” treatment of diabetes is viewed as patients receiving no more than two injections of insulin with no or infrequent self-blood glucose monitoring. Most of the studies reviewed involved both T1DM and T2DM especially when meta-analyses were performed. It is noted that within the meta-analysis explored that IDDM 1 and IDDM 2 are analyzed separately in terms of outcome. In 2006, a meta-analysis, performed by Stettler et al., involved studies linking a reduction in the development of macrovascular complications and intensive insulin therapy.9 The review included 8 studies of IDDM 1 patients (N=1800, with a total of 5,578 person-years of intensive CSII Therapy in the Perioperative Period 20 insulin therapy and 5,717 person-years of conventional insulin therapy) and observed the incidence of a “macrovascular event” as a measured outcome. The term “macrovascular event” was defined as any incident that included a fatal or non-fatal myocardial infarction (MI), the need for either cardiac bypass vessel graphing or angioplasty, the development of congested heart failure (CHF), incidence of stroke, or the development of peripheral vascular disease (PVD) as evidence by the diagnosis of claudication in the extremities or amputation of a lower extremity. After analysis of the 8 studies, it was found that in the intensified group there were a total of 33 macrovascular events within the person-years of follow-up compared to 99 macrovascular events within the conventional insulin therapy group. It was found that the incidence of macrovascular complications was less in trials where there was a greater reduction in HgbA1C (p= 0.050). The incidence rate ratio was 0.36 for all studies analyzed, in favor of intensive insulin therapy. Limitations of this meta-analysis include noting that all of these studies in did not set out to observe macrovascular complications directly. For example, the Diabetes Control and Complications Trial (DCCT) study used the development of retinopathy (a microvascular complication) as a measured end-point for observation of intensive versus conventional insulin therapy. The incidence of macrovascular complications was not a targeted measurement, but however was an indirect observation. Many of these observations were subclinical in nature without patient complaint, meaning that a routine ECG that indicated a past MI was included as a macrovascular event (i.e. a “silent MI”). In addition, there were six studies included in this meta-analysis that were measurements of relatively small sample populations (average N= 59) as compared to two other studies that were very large in sample size (average N= 719.5). It is possible that the two larger studies could have caused skewing of the overall data observed. CSII Therapy in the Perioperative Period 21 A meta-analysis of the incidence development of microvascular complications in terms of conventional versus intensive insulin therapy could not be retrieved. However, it is noted that there are studies have been conducted that favor an intensive insulin therapy regimen for a reduction in the incidence of microvascular comorbidities. The largest of these studies (which was included in the aforementioned meta-analysis) was the DCCT, which was performed in 1993.8(p2232) The sample size included 711 patients who were assigned intensive glucose control and 730 who were assigned conservative glucose control. The sample population was followed for an average of 6.5 years. In the DCCT trial, “intensive glucose control” involved treating T1DM with either multiple daily insulin injection (MDI) or CSII therapy. Both intensive management therapies included ISBGM. Conventional glucose control was managed by no more than two injections of insulin daily with infrequent self-blood glucose monitoring (SBGM). This study shows it’s significance by observing a 76% decrease in the development of retinopathy in those with intensive glucose control (p= <0.001) and a 69% reduction in the development of neuropathy with intensive glucose control (p=0.006).8(p2233) It is important to note that this study was partially blinded and that if serious complications developed, both the patient and the clinical researcher were allowed access to outcome data. Otherwise, data was inaccessible to both parties. The Stockholm Diabetes Intervention Study (SDIS) was also conducted in 1993 and observed both HgbA1c levels and the development of serious retinopathy as measurable outcomes.8(p2233) In comparison to the DCCT study, the SDIS study looked at a smaller population size (N= 102) with 48 patients receiving intensive glucose control therapies and 54 utilizing conventional treatments. The SDIS “intensive” therapy differed from the DCCT trial by omitting CSII as a treatment option. Instead, at least three daily subcutaneous injections of CSII Therapy in the Perioperative Period 22 insulin were administered within this group, along with continuous education about the importance of maintaining blood glucose control. The conventional group received insulin in no more than two subcutaneous injections per day and routine diabetes management. The first 5 years of the study included both the intensive and conventional therapy groups, however at the end of the 5 years, the conventional group was switched to the intensive therapy group. The study was conducted over 7.5 years. The development of severe retinopathy in the intensive control group was 27% as compared to 52% incidence in the conventional therapy group. This was calculated to be significant with a p value of 0.04. The development of nephropathy in the intensive control group was statically lower in the intensive glucose therapy group (p= 0.04). However, there was no significance in the development of peripheral neuropathy when comparing the two groups (p= 0.1). Limitations to this study include a small sample size and the incidence of up to 60% of conventional therapy individuals being switched to intensive treatment during the last 2.5 years of the study.8(p2233-2234) Despite the limitations of the previous studies, it is fair to state that optimal glucose control has benefits to reducing the long-term complications of T1DM. Intensive glucose control therapy more closely resembles how the pancreas functions under normal circumstances. As the pancreas continuously secretes insulin to control blood glucose levels, so does frequent administration of insulin for the diabetic patient aids in achieving normoglycemia and thus the prevention of complications associated with T1DM. CSII Therapy in the Perioperative Period 23 Chapter 6: Insulin Pump Therapy Background Initial Conception and Early Designs The idea of an external device used to continuously deliver insulin was first conceptualized in the early 1960’s. In 1963 Arnold Kadish introduced a closed-loop device, meaning that while delivering insulin, blood glucose levels were constantly monitored.2(p2) This closed-loop machine would administer additional insulin when blood glucose levels were detected outside an acceptable range using a pump with an autoanalyzer and pump function was controlled via an on-off servomechanism.10 The device resembled more of a jetpack and it’s large and bulky structure left little to practical use. Advances in computer technology lead to development of the first machine run by a computer. In 1974, the Biostator was introduced which used computer algorithms to calculate insulin and dextrose delivery based blood glucose levels. The pump itself was computer controlled, and blood glucose levels could be plotted and printed in minute intervals on a graph. Like Kadish’s device, the Biostator was a closed-loop system, allowing continuous monitoring of blood glucose levels and an allowing an appropriate response from the machine. Again, the Biostator was large and bulky, requiring it’s placement on a desktop for use. Because of this limitation, it was mainly used for clinical trials, thus providing primary research for more practical approaches to CSII therapy.10(p128) The late 1970’s saw improvements in computer technology and the introduction of the microprocessor. The Mill-Hill insulin infusion pump took advantage of this technology: It was portable and weighed at a relatively light 159 grams, it allowed two means of insulin delivery with a basal infusion rate and an increased prandial rate, and it was powered with a battery.2(p3) The user pushed a button initiated the prandial rate before a meal was consumed and allowed an CSII Therapy in the Perioperative Period 24 eight times higher than basal rate infusion. This pump was an open-loop system meaning that the administration of insulin was not immediately adjusted to blood glucose levels. The MillHill infusion pump was a first in that delivery of insulin was via the subcutaneous route. An intravenous (IV) route connected previous devices, which lead to complications such as phlebitis, infection, and thrombosis. Studies such as the 1978 Pickup and Keen study demonstrated that portable CSII could be a practical approach in the management of T1DM.11 Additional support from additional research lead to the first commercially available CSII pump. One of the first marketed pumps, the Autosyringe, became available in 1978. The same team that developed the Mill-Hill infuser developed a pump that utilized a microprocessor-controlled pump known as the Nordisk infuser.10(p129) Because of the continuous improvements to technology, pharmaceutical companies began to develop more CSII pumps during the early 1980’s. Early Limitations of Its Use and Improvements in Technology These early insulin pumps did have their limitations that eventually lead to reservation of its use and a sense of caution in healthcare providers. For example, in the 1980’s, the pumps were relatively large, awkward (average weight was around 400 grams) and their batteries had to be recharged often.16 Several instances of tube occlusion and needle dislodgement lead to several cases of DKA and hyperglycemia. Infection at the site of infusion was common, not to mention that needles used to deliver the insulin were metal and very uncomfortable. There were no safety alarms so careful observation of the insulin reservoir had to be maintained so that there wasn’t a sudden loss of insulin. The basal rates were limited in customization and some pumps required a screwdriver to alter the basal rate. Because of these limitations, CSII was often reserved to difficult-to-manage diabetes, and even then outcomes were less than optimal.10(p130) CSII Therapy in the Perioperative Period 25 The 1990s gave way to vast improvements in CSII therapy. Improvements in technology lead to resolution of previous issues such as tube occlusion, the accidental delivery of too much insulin, leaking of insulin, and a decrease of the pump size.10 Also, alarms became available to notify the patient of low battery status and low insulin levels in the pump. These many improvements in insulin pump technology lead to greater use among T1DM patients and allowed adequate sample populations to be studied. Today CSII therapy involves pumps that are comparable in size and weight to a pager. Subcutaneous insulin delivery infusion sets that are plastic thus making the wearing of the device more comfortable. Proper education and development of improved insertion techniques have lead to a decrease in the incidence of infection at the infusion site.3(p2296) Batteries can be used for extensive periods of time before recharging or replacing is required. Prandial boluses can be calculated from integrated programs within the pump. Depending on the brand, basal rates can be adjusted within 0.025 U/hr.10(p131) A unique feature of the Medtronic MiniMed Paradigm CSII pump is the availability of a separate continuous glucose monitor that transmits data to the pump so that trends can be established and warn of any potential fluctuations in BG.12 These several improvements in CSII therapy have eliminated many past fears associated with it’s use and has greatly expanded CSII therapy. Advantages to CSII Use The obvious benefit to CSII therapy in T1DM patients is better glycemic control as compared to conventional diabetes management. There is evidence that gives CSII an advantage over blood glucose control as compared to MDI therapy.13,15 A meta-analysis exploring this topic will be reviewed in the next chapter. This benefit of controlled BG levels results in a CSII Therapy in the Perioperative Period 26 decrease of HgbA1c level and can be concluded that the risk of developing T1DM complications is lowered as well. Studies have shown that hypoglycemic events have a decreased incidence among patients who utilize CSII therapy. In fact, recurring hypoglycemia is an indication for CSII use. This minimization of hypoglycemia may be contributed to the patient’s commitment to check BG levels frequently. Also, with CSII therapy, there is no depot of insulin that is created at the site of infusion, unlike with regular subcutaneous injection sites. Exercise, exposure to heat, and manual manipulation can cause increased availability of insulin to the blood stream from the development of these depots. As mentioned previously, some CSII pumps come with a continuous BG monitor that alarms when hypoglycemic events are about to occur. Perhaps the greatest advantage to CSII therapy is the flexibility it allows the T1DM patient. Patients are able to adjust their insulin rates on an hourly basis and therefore it is allowable to skip a meal without the consequence of hypoglycemia.3(p2295) Additionally, they can sleep in late if they choose since the CSII pump continues to deliver insulin in an unconscious state. They do not have to inject themselves on a regular basis and are able to engage in strenuous exercise. It is thought that increased patient freedoms have lead to a spike in CSII therapy use.2 Disadvantages to CSII Use CSII therapy does have its fair share of drawbacks. CSII therapy does not create a depot of insulin at the infusion site can therefore result in DKA if insulin infusion is suddenly interrupted. This in combination that a short-acting insulin (lispro is the common insulin used in CSII pumps) can lead to DKA more quickly than with other treatment methods. On the opposite spectrum, in the past there have been reports of CSII pump malfunction in which too much CSII Therapy in the Perioperative Period 27 insulin is delivered resulting in severe hypoglycemia.3(p2295) However, improved microprocessor technologies have generally eliminated this problem and this problem has not been documented in the past 10 years.10(p130) Frequent blood glucose monitoring can help eliminate both potential DKA and severe hypoglycemia. Also, there is a risk of infection at the site of infusion. This is listed as a primary reason behind discontinuing CSII therapy. Often, a cellulitis develops because of infection. The development of an abscess is rare in CSII site infection. The estimated occurrence rate of infection is between 7.3 and 11.3 per 100 patient years.10(p130) Proper education and aseptic techniques can help minimize this complication. Weight gain is common among patients who switch from conventional T1DM therapy to CSII therapy. In the DCCT trial, patients utilizing CSII treatment gained an average of 4.5 kilograms as compared to those within the conventional treatment group. It is important to note the same study revealed no difference in the weight gained between CSII therapy and MDI therapy. The weight gain is mostly due to reducing glycosuria in these patients, but exercise and close monitoring of caloric intake can help minimize this disadvantage.10(p131) How a CSII pump works A CSII pump (or insulin pump) is a small electronic device that currently is about the size of a pager and weighs less than 100 grams. There are two main parts: The infusion pump and the infusion catheter set. The insulin used is ultrashort-acting and the most commonly found in CSII pumps is lispro.3(p2296) Insulin is found in a syringe or reservoir within the pump. Rechargeable or replaceable batteries are found within the pump device. Using several calculations and making adjustments based on patient response, basal rate and prandial insulin rates can be calculated.12(p2) CSII pumps have the ability to store several CSII Therapy in the Perioperative Period 28 different basal rates depending on the pump manufacturer.3(p2294) In addition, some pumps allow the capability to calculate postprandial insulin doses by entering how many carbohydrates were consumed during the meal. As mentioned previously, those CSII pumps that have continuous glucose monitoring capabilities allow trend in insulin delivery and blood glucose levels to be observed. All CSII pumps on the market today are open-loop systems and are not to be confused with a closed-loop system. Open-loop systems require manual input from the user to adjust insulin dosage rates whereas a closed-loop system acts more like an artificial pancreas as described previously. Although some current CSII pumps allow continuous glucose monitoring of interstitial fluid and the blood glucose level is calculated and transmitted to the device, insulin rates are not adjusted per the pump. Patients must decide on their basal rate for the day and manually press a pad on the CSII pump to activate bolus doses. Current technology does not allow for automatic adjustments in insulin rates, as there are limitations in the continuous glucose-monitoring device for acceptable use in a closed-loop system.2,3,10 Primary insertion sites for CSII infusion catheters include subcutaneous tissue found around the abdomen and the upper buttocks. Upper arm and upper anterior thigh subcutaneous tissue are additional insertion sites.12 The infusion catheter set can remain for 72 hours before removal is required. The catheter infusion set must be rotated to a different aforementioned site in order to prevent the development of lipohytroperphy and scar tissue. During pregnancy, insertion of the device is best avoided in skin tissue of the abdomen where the skin is tense. The best practice for preventing skin infection at the insertion site is to maintain aseptic technique: Wash hands prior to inserting the catheter infusion set, keep the infusion set sterile, and cleanse CSII Therapy in the Perioperative Period the site with an aseptic skin wipe. If a skin infection develops, it is often caused by the staphylococcal bacterium and is treated with oral antibiotics. 3(p2295) 29 30 CSII Therapy in the Perioperative Period Chapter 7: Optimizing Diabetes Treatment via Continuous Subcutaneous Insulin Infusion Therapy Evidence in Support for CSII versus MDI treatment of T1DM Perhaps the best support for CSII therapy came from a meta-analysis by Jeitler et al in 2008.15 This retrospective analysis reviewed data from a total of 17 studies. The goal of the meta-analysis was to compare the effects of CSII therapy to MDI therapy, which was measured by glycemic control. Other measured outcomes such as insulin requirements and hypoglycemic events were reviewed, but not included in the meta-analysis. A total of 22 studies were reviewed to include all measured outcomes, however only 17 studies were considered for the metaanalysis. For purposes of this paper, the meta-analysis regarding adult T1DM patients and glycoslated hemoglobin will be reviewed. Twelve of the total 17 studies were included in evaluation of glycoslated hemoglobin levels. Six of the 12 adult T1DM studies were included in meta-analysis of HgbA1c comparison between MDI therapy and CSII therapy. It was found that the weighted mean difference between MDI therapy and CSII therapy was -0.04% in favor of CSII therapy and held an I2= 72% indicating heterogeneity. The remaining 6 studies measured HgbA1 with a weighted mean difference of -0.06% in favor of CSII therapy and an I2= 84% which also indicated heterogeneity. Additionally, there was no statistical difference when the two groups were analyzed.15(p943-946) Based on these results, it can be strongly suggested that CSII therapy is beneficial for decreasing glycoslated hemoglobin levels without the increased risk of developing hypoglycemia. According to the authors of the study, no meta-analysis of hypoglycemic events was performed due to small numbers of patients reporting mild hypoglycemia and rare reports of CSII Therapy in the Perioperative Period 31 severe hypoglycemia during the trials. There was also a lack of values in the studies that were required for variance calculations. Limitations of the analysis included the high degree of heterogeneity. It is noted that several sensitivity tests were performed to help explain the high levels of heterogeneity but were unable to do so.14(p946) Several of the studies included were older in nature (dating from 1982), did not use the same CSII pump, were not the same in terms of study design, and had smaller sample populations. Interestingly, older studies did not show a statistical difference in the lowering of glycoslated hemoglobin between CSII therapy and MDI therapy, however all studies newer than the year 2000 did show a statistical difference. Perhaps this is an indication of improved technology yielding improved results. Current use of CSII Therapy in Diabetes Mellitus The most studied and utilization group for CSII therapy is by far the T1DM population. After multiple reports of supporting research in favor of CSII therapy, its use has greatly expanded, especially in the United States. It is estimated that 35% of IDDM 1 patients in the United States are current CSII users.2(p6) The United States is considered a “high-use” country as compared to the United Kingdom where current CSII use is only limited “a few hundred users”.14 Discrepancies in rates of use can be contributed to unpredictable reimbursement of pumps and/or supplies and lack of knowledge in regards to benefits of CSII therapy. At this point, use in T2DM patients is limited, although its expanded use in this patient population is currently being explored. When a patient and his or her endocrinologist explore potential implementation of CSII therapy for the treatment of T1DM, there are several indications for CSII therapy: Recurrent hypoglycemia, pregnancy, frequent hospitalizations, recurrent episodes of DKA, incidence of CSII Therapy in the Perioperative Period 32 dawn phenomenon, gastroparesis, low insulin requirements, or patient preference.2,14 The patient should meet the following characteristics as well: be highly motivated, be responsible, be psychologically stable, be agreeing to measure food intake, and be agreeing to medical followup. Although there are few studies evaluating CSII therapy for T2DM treatment, research in this topic is expanding due to a potentially large market. As T2DM continues its course, insulin resistance increases and beta cell dysfunction increases. Eventually many patients require insulin to maintain normoglycemia. Many of the potential benefits that could be obtained from CSII therapy in T2DM patients are extrapolated from benefits seen in CSII therapy in T1DM patients.2(p79) The use of CSII in T2DM is controversial and is associated with additional weight gain but nonetheless, additional research is required to determine the appropriateness of CSII therapy in T2DM patients.15(p948) CSII Therapy in the Perioperative Period 33 Chapter 8: Continuous Subcutaneous Insulin Infusion Therapy and Anesthesia Practice Effects of Surgery and Anesthesia on Glucose Regulation Perhaps the most obvious effect of surgery on the patient is stress response. Stress response can be defined as an increased metabolic rate, increased secretion of hormones, an impaired immune response, among other physiologic responses. The sympathetic stress response results in increased circulating epinephrine, norepinephrine, cortisol, and growth hormones.16,17 In regards to the diabetic patient, the key stress response to surgery is the secretion of cortisol. Cortisol is a powerful hormone that is secreted by the zona fasiculata in the adrenal glands. It is responsible for the induction of glycogenolysis to increase BG levels and dampen the immune response. Neuraxial anesthesia can help minimize the sympathetic response to surgery and therefore minimize these glucose-liberating hormones.16(p) In addition to the sympathetic response created by surgical trauma, halogenated anesthetics have adverse effects on metabolic homeostasis. In vitro studies have demonstrated a dose-dependent decrease in insulin response to hyperglycemia in the following anesthetic agents: Isoflurane, halothane, and enflurane. Although benzodiazepines decrease the presence of adrenal corticotrophic hormone (ACTH) and thus the secretion of cortisol, they have been linked to a paradoxical response that results in an increased secretion of growth hormone.17(p85) Despite the negative impacts of surgery and anesthesia on glucose regulation, there are a few examples of anesthetic technique that can help stabilize the previously mentioned alterations in glucose homeostasis. Etomidate has been demonstrated the ability to minimize cortisol secretion by impairing the production of adrenal steroids.16,17(85) Use of high-dose opioids block the sympathetic response to surgical stress and therefore prevents the release of metabolic- CSII Therapy in the Perioperative Period 34 altering hormones. In continuation of opioids-based technique, regional anesthesia is also beneficial in glucose regulation because of its ability to block the sympathetic response.17(p86) Normoglycemia and Improved Surgical Outcomes Poorly controlled blood glucose levels have been linked to several postoperative complications. Acute hyperglycemia has been shown to delay wound healing secondary to depression of immune function. It has also been related to increased levels of inflammatorycausing cytokines. Hyperglycemia can trigger diuresis and thus lead to dehydration and electrolyte imbalances.18 DKA is always a potentially lethal outcome, especially in T1DM patients after surgery. Several retrospective studies linking postoperative complications and BG control have focused on patients undergoing cardiac surgery. These studies have produced mixed results in terms of perioperative glucose control and improved surgical outcomes, although more current studies suggest that there is indeed a link between glycemic control and unfavorable outcomes.18(p484) A 2005 study by Gandhi et al suggested that within cardiac surgery patients, there is a 30% risk increase in adverse outcomes for every BG increase of 20 mg/dL in serum glucose greater than 100 mg/dL.19 For non-cardiac surgical patients, there are few studies that research intraoperative BG control and a potential link to poor outcomes. What constitutes an acceptable upper-end perioperative serum glucose level is diverse among anesthesia providers. Generally, acceptable practice is to control BG levels and prevent both hyperglycemia and hypoglycemia. A more definitive “high end” BG level was defined in 2009 by a joint statement from the American Association of Clinical Endocrinologists and the American Diabetes Association. Current recommendation is to generally keep blood glucose levels less than 180 mg/dL, depending on the patient’s status.20 For example, in the critically ill CSII Therapy in the Perioperative Period 35 patient, a BG level of 140-180 mg/dL is more desirable. The group also cautions against ambitious treatment of hyperglycemia, as hypoglycemia is more likely to result. A suggestion to prevent hypoglycemia is the implementation of frequent BG checks. Establishing the Clinical Question: What is the Role of CSII in the Perioperative Period? It is clear that CSII therapy is beneficial in the treatment of T1DM. It provides the continuous basal infusion rate that T1DM patients require for survival. It also provides postprandial bolus doses so that large fluctuations in BG levels can be avoided. CSII therapy has suggested through numerous studies that it is superior in maintaining normoglycemia and preventing long-term complications of T1DM as compared to conventional insulin therapy or MDI therapy. Likewise, maintaining normoglycemia, as evidence by numerous clinical studies, can minimize the risk of perioperative complications. Is it possible to utilize a patient’s CSII pump during a surgical procedure as an adjunct in management of T1DM? Attempts to close this knowledge gap will be explored in the following chapters. CSII Therapy in the Perioperative Period 36 Chapter 9: Attempts at Research and CSII during the Perioperative Period Unfortunately, randomized studies observing the outcomes of conventional IDDM 1 management and use of CSII during the perioperative period have not been explored. Most recommendations for its presence during this inpatient timeframe are based on expert opinion and not evidence-based medicine. However, the need to close this knowledge gap has been identified as case studies and preliminary studies have recently been published. The following investigates the presence of CSII in the perioperative setting. Case Study #1: Presence of CSII During General Anesthesia In 2004 the AANA Journal published a case study on a 43 year-old patient, physical status III, who had T1DM and managed his diabetes via CSII. He presented for repair of L5-S1 disc herniation, which resulted in right leg and back pain. He had no other medical problems besides the aforementioned issues. He was of normal weight and stature. His labs were normal except that his BG level was 64 mg/dL, therefore he was given a 4 gram glucose tablet to ingest.21 His CSII pump was set to deliver his established basal rate at 0.3 u/hr and the insulin used in his pump was the standard ultrashort-acting insulin lispro. According to the authors, the patient was very knowledgeable regarding his disease and use of his CSII pump. Dependent on time of the day, the patient’s CSII pump would infuse various basal rates, ranging from 0.2 U/hr to 1.0 U/hr. What was not discussed in the case study was the patient’s insulin sensitivity factor (ISF), what time of the day the patient underwent surgery, or what determined the 0.3 U/hr basal insulin infusion rate.21(p354) The patient had a remifentanyl infusion begun prior to his rapid sequence induction. After successful induction, the patient was repositioned prone and care was taken not to interfere CSII Therapy in the Perioperative Period 37 with the CSII pump’s position and operational status. The maintenance of general anesthesia was obtained by utilizing the remifentanyl infusion at between 0.125 and 0.50 mcg/kg and sevoflurane at 0.8%. The entire operation lasted 66 minutes. Intraoperatively, BG was found to be 118 mg/dL and no adjustments were made to the patient’s CSII pump. A high dose administration of dexamethasone 20 mg IV was performed at the surgeon’s request along with ketorolac 30 mg intramuscularly. At completion of the procedure, the patient was extubated without incident and transferred to the postanesthesia care unit. His blood glucose was checked and was 158 mg/dL. After initial phase recovery, the patient consumed a meal and administered a 1.8 U insulin bolus via his CSII pump. The final BG obtained was 185 mg/dL and discharged home one hour later.21(p355) It was not mentioned in the case study that the patient received any extra insulin from hospital staff. This case study revealed that CSII could be utilized during the perioperative period. The authors believe that CSII is a helpful tool in managing a patient’s T1DM and simplifies glucose control by eliminating the need of intravenous insulin and dextrose infusions. The authors recommend that patients are normoglycemic prior to induction so that the occurrence of intraoperative hypoglycemia is minimized. They also recommend that the anesthesia provider ask the patient how to turn off the CSII pump, how to adjust basal insulin rates, how to determine proper pump function and how to attach an infusion catheter set should it become dislodged. Support of this recommendation originates in their belief that the CSII pump user is highly educated of their device and disease. The authors also recommend checking BG levels at a minimum of one hour and checking CSII pump screen occasionally to assess pump function CSII Therapy in the Perioperative Period 38 during the intraoperative period. The authors also recommend that intravenous solutions should not contain dextrose. Reservations raised from this case study include location of the CSII pump infusion site and what guidelines would be utilized if adjustments in the basal rate were required during the intraoperative period. The authors did not discuss where the infusion site was located and whether or not the infusion site needed to be moved to a site that allowed both optimal surgical access and anesthesia provider access to the CSII pump. These are potential issues that could interfere with CSII therapy during a surgical procedure. Also, concern arises from adjusting basal rates without asking the patient about their ISF. ISF is the amount a patient’s blood glucose level decreases with one unit of ultra short-acting insulin lispro administered. As mentioned previously, the patient’s ISF was not disclosed in this case study although a general consensus was discussed and that for one unit of subcutaneous lispro will lower BG30 to 50 mg/dL. As patients with CSII pumps are very knowledgeable, patients are able to disclose their personal ISF to the anesthesia provider, which can be useful in determining customizable intraoperative basal rates. Case Study #2: Complications After Discontinuation of CSII Therapy In 2005 the Journal of Clinical Anesthesia published a case study about extreme hyperkalemia after discontinuation of CSII therapy. The patient was a 35 year-old male, physical status IV, who was undergoing surgery for renal transplant. He had the diagnoses of T1DM, retinopathy, hypertension, gastroparesis and renal failure. His medication list included aspirin, fexofenadine, ranitidine, valsartan, verapamil, ramipril, furosemide, and terazosin. He received insulin via a CSII pump and his basal rate was set at 0.8 U/hr. His BG in perioperative CSII Therapy in the Perioperative Period 39 labs was 74 mg/dL and his potassium was 5.1 mEq/L. Decreased renal function was evident as BUN was 75 mg/dL and creatinine was 4.6 mg/dL.22 Since the CSII pump infusion site was located within the surgical field, the CSII pump was discontinued and removed from the patient. Plan was to frequently monitor BG levels and cover insulin requirements as needed. Induction of general anesthesia was performed without complications. Maintenance of general anesthesia was obtained via isoflurane. Following induction, blood glucose was 134 mg/dL and serum potassium was 5.3 mEq/L. Three hours after start of surgery, BG was found to be 112 mg/dL however serum potassium was found to be a critical 7.6 mEq/dL. Despite the hyperkalemia, no changes in electrocardiogram were noted per the authors. The patient was administered 3 U of regular insulin and hyperventilated (minute ventilation of 11 L). In 15 minutes serum potassium had decreased to 6.9 mEq/L. The patient was then given a 2 unit regular insulin bolus and started on a regular insulin infusion of 0.8 U/hr (note the basal rate of the CSSII pump). Serum glucose was 201 mg/dL however the serum potassium continued to trend downward with a value of 6.1 mEq/L. Shortly after initiation of the insulin infusion, renal blood flow was established to the newly transplanted kidney; the kidney immediately began to produce urine. The serum potassium level was 5.2 mEq/L after 1 hour of the intravenous insulin infusion drip. Normoglycemia was present as evidence by a blood glucose level of 114 mg/dL. According to the authors, the remainder of the surgery was uneventful. After transfer to the postanesthesia care unit, BG was 169 mg/dL and serum potassium was 4.9 mEq/L.22(p631) This article demonstrates not only the role of insulin and extracellular potassium regulation, but also the need for frequent monitoring of these patients. Although BG and serum potassium levels did not dramatically rise immediately, had levels been checked every hour CSII Therapy in the Perioperative Period 40 instead of the initial 3 hours, the rise in potassium could have been trended and treated before it reached critically high levels. Based on description of this patient, he had poorly controlled diabetes that had resulted in several co-morbidities. This is evidence in itself for frequent serum monitoring. Although this is only one example of complication from discontinuation of CSII therapy, it can be extrapolated that these patients should have some sort of basal insulin infusion either via their CSII pump or via an intravenous insulin infusion drip set at their basal infusion rate. Upon conclusion of the case study, the authors present the same recommendation. Observing CSII Therapy in Patients During the Perioperative Period The purpose of a study titled “Insulin Pump Therapy in Patients Undergoing Surgery” was to observe the perioperative management of patients who received CSII therapy. The findings were presented during the American Association of Clinical Endocrinologists’ Annual Meeting in 2011. The study was retrospective and used documentation review for gathering data.23 The study reviewed 50 general anesthesia surgical cases over the course of 5 years in which the 35 patients with T1DM utilized CSII therapy. The nature of the surgery varied: 16 orthopedic, 9 general surgical cases, 7 urologic, 7 involving renal transplant, and 11 were classified as “other”. The review of documentation revealed discrepancies in not only CSII pump use, but documentation of BG levels as well. During the intraoperative period, documentation revealed that in 7 cases the patient was disconnected from the CSII pump, in another 7 cases the CSII pump was only suspended. The status of the CSII pump in the remaining 36 cases during the intraoperative period is unknown, as documentation of its presence is absent. Further review showed that intraoperative glucose was recorded in 30 of the 50 cases. CSII Therapy in the Perioperative Period 41 This study revealed inconsistency in documentation of intraoperative management of T1DM, which happens to be a responsibility of the anesthesia provider. Because of the poor documentation, it is difficult to draw conclusion about how anesthesia providers feel about the presence of CSII therapy during the perioperative period or how it is managed. The sample population was small and the outcomes of this study are a possibly a reflection of an institutions attitude toward management of T1DM and CSII therapy. Further studies should not include a retrospective approach, but instead a prospective approach so that outcomes may be observed. CSII Therapy in the Perioperative Period 42 Chapter 10: Published Opinions and Recommendations for CSII Therapy During the Perioperative Period Specific guidelines have yet to be published for CSII therapy during the perioperative period. The American Diabetes Association and the American Association of Clinical Endocrinologists have yet to establish recommendations or guidelines regarding this topic. Guidelines that were retrieved from the literature were sourced from hospital-based policy and procedures. These guidelines were variable from institution to institution, as were professional opinions. In a published review from The Diabetes Educator, guidelines with outcome measures were proposed for CSII therapy in the hospital setting. Contraindications to inpatient CSII therapy included: “Patient with altered states of consciousness; critically ill patient requiring intensive care; patient at risk for suicide; patient refuses or is otherwise unable to participate in own care; family member, friend or significant other refuses or is otherwise unable to participate in care; radiology procedure; other circumstances identified by the physician”24 Patients would also be required to carry their own CSII pump supplies since, according to the authors, “because hospitals typically do not keep insulin pump supplies in their formulary (except for insulin)”.24(p852) Unfortunately, the proposed guidelines did not include CSII therapy use during the perioperative period and the authors noted this limitation. They did state that if a patient required general anesthesia for a surgical procedure that CSII therapy should be discontinued since the patient would be unable to regulate their CSII pump. An argument against this recommendation is that patients are unconscious every night as they sleep yet still continue to receive insulin via their CSII pump. CSII Therapy in the Perioperative Period 43 An example of an institutional perioperative glycemic control program can be found at Yale-New Haven Hospital in Connecticut. Fortunately, the staff involved acknowledged patients on CSII therapy and stated that those receiving therapy should have their basal rate decreased by 20% at midnight before surgery. However, guidelines at this institution state that intraoperatively, CSII therapy should be discontinued and insulin should be administered IV. They recommend that hourly BG checks should be performed throughout the perioperative period.25(p6) It is recommended that CSII therapy be discontinued when the patient is to undergo major surgery.2(p47) Instead the patient should be transitioned to a regular insulin intravenous infusion at the basal infusion rate with blood sugars being monitored at least every hour. There are conflicting opinions as whether or not to place the patient on a dextrose infusion as to when an IV insulin drip is initiated.25,26 Currently there are no evidence-based studies to support these claims, but are instead a matter of professional opinion. If the procedure is short and non-complex, the anesthesia provider feels comfortable with the CSII pump, the CSII pump will not interfere with the surgical field, or radiology will not be performed intraoperatively, there are recommendations for using CSII therapy during the perioperative period. Some recommendations for the anesthesia provider include: maintaining the insulin infusion rate, withholding preprandial doses of insulin, measuring blood glucose levels at least every hour, knowing the ISF, and making sure preoperative diet is resumed.27(669) If hyperglycemia occurs during the surgical administration, regular insulin can be administered subcutaneously. Making sure the CSII pump is secure and available to the anesthesia provider at all times is necessary as well. Again, these recommendations are not evidence-based, but founded on expert opinion. CSII Therapy in the Perioperative Period Chapter 11: From the Source: Insulin Pump Manufacturer Guidelines 44 CSII Therapy in the Perioperative Period 45 The 3 most popular insulin pumps available in the United States include Medtronic, Insulet Corporation and Animas Corporation. Of the 3, Medtronic offers inpatient guidelines for management of patients on their insulin pump (the Medtronic MiniMed Paradigm). They also happen to represent approximately 85% of the United States market share.10(p133) According to Medtronic, the company agrees that the best method to maintaining normoglycemia during inpatient status is through use of the patient’s CSII pump. The manufacturer also emphasizes that staff should place trust in the patient regarding management and knowledge of his or her CSII pump. Basal rate is to continue despite NPO status. It is strongly suggested to continue CSII therapy, as discontinuation will result in DKA. If CSII therapy must be withheld, treatment should involve administration of fast-acting insulin. Medtronic notes that their pumps are not MRI compatible and will require removal. The CSII pump should not be exposed to radiation (i.e. x-ray, computerized tomography scans, fluoroscopy). Note: It is important that this information was received in informal, company-provided literature. Chapter 12: Conclusions and Recommendations CSII Therapy in the Perioperative Period 46 Disease Process of IDDM 1 Results in Potentially Devastating Complications Currently, there is no ability to prevent the autoimmune destruction of beta cells that eventually leads to T1DM. Initial insult may have occurred before symptoms of T1DM appear and therefore treatment does not begin until beta cell destruction is near complete. The disease affects millions worldwide and percentage of occurrence is noted to be increasing.1 The pathophysiology of T1DM is complicated, with several derangements of metabolic pathways. Because of chronic hyperglycemia alterations in metabolic pathways there is creation of irreversible damage at the microcellular level that eventually results in more global injury. These injuries are numerous and include: Blindness secondary to retinopathy, renal failure secondary to nephropathy, painful neuropathies, and heart disease and myocardial injury secondary to vascular damage. All of these complications result in an obvious poor quality of life. Fortunately, optimizing glycemic control can significantly reduce the risk of these complications from developing. Several studies and subsequent meta-analysis reviews have greatly supported this claim. However, optimizing glycemic control can prove to be a challenge as it can be difficult for a patient to attempt to mimic the normal physiologic response to insulin secretion. Conventional insulin therapy (no more than 2 insulin injections per day) does not best obtain normoglycemia (as evidence by research) and MDI therapy offers improvement in achieving normoglycemia. According to several studies and meta-analysis review, the ideal form of achieving normoglycemia is through CSII therapy. From its early conception, CSII therapy is designed to replicate pancreatic function. It provides a basal rate, in which so does a normal functioning pancreas. Improved technology in CSII pumps have allowed preprogrammed boluses to be administered for post meal insulin CSII Therapy in the Perioperative Period 47 requirements. CSII pumps can be worn along with continuous glucose monitoring, which allows trends in glucose level and insulin administration to be analyzed. Not only has research supported improved normoglycemia in CSII therapy, but has also demonstrated a risk reduction in: The onset of diabetic complications, a decreased risk in hypoglycemia, and decreasing insulin requirements. Also, a link between improved psychosocial status and CSII therapy has been identified in research. CSII Therapy and the Perioperative Period Because of improved technology and supporting evidence for its use, CSII therapy is increasing in popularity as a method of treating T1DM. As more T1DM patients look to this form of therapy, there will be an increased presence of patients who present for surgery who receive CSII treatment. These patients will present for surgery, as an estimated 50% of all IDDM 1 patients will require surgical intervention at some point during their lifetime. There is a general consensus among anesthesia providers that optimized glucose control within the perioperative period allows improved outcomes, whether these outcomes include avoidance of DKA, avoidance of hypoglycemia, or improved wound healing. Practice Recommendations It should be known to all anesthesia providers that all T1DM patients do require some form of basal insulin. That could be in the form of a long-acting agent such as glargine or a continuous infusion of ultrashort-acting insulin lispro via a CSII pump. It is important to note that serious complications can develop in a relatively short period of time if a patient is abruptly discontinued from their continuous ultra short-acting insulin. Because of this, it is highly recommended that either CSII therapy continue, or a regular insulin IV infusion is started at the patient’s NPO basal rate immediately after discontinuation of the CSII pump. At this time, it is CSII Therapy in the Perioperative Period 48 debatable whether or not to include a potassium-dextrose containing IV solution when an insulin infusion drip is initiated.4,19 Argument for the dextrose solution is that hypoglycemia and hypokalemia will be prevented and at the worst, mild hyperglycemia will result. Argument against the supplemental solution is that if regular insulin were replacing the NPO basal rate of the CSII pump, then no additional nutrition would be required. Additional recommendations include checking BG levels at a minimum of every hour to avoid hypoglycemia and hyperglycemia. This recommendation applies to providers who may decide to continue CSII therapy during the procedure or if CSII is discontinued. As mentioned in the previous case study discussing serious hyperkalemia after discontinuation of CSII therapy, drastic changes in baseline labs can be at the least trended and addressed prior to critical levels if they are being monitored frequently. Deciding on whether or not to utilize CSII therapy during the perioperative period depends on several factors. Initially, the anesthesia provider should investigate to locate any potential hospital-based guidelines regarding inpatient or perioperative CSII therapy use. However, deciding whether or not to continue CSII therapy during the perioperative period is based on the anesthesia provider’s comfort level with the device. If the anesthesia provider feels he or she does not have confidence in managing the patient’s CSII pump, then it should be discontinued, and the patient is provided insulin coverage. Other factors that limit CSII therapy in the perioperative period include: Surgical site interference, long and complex procedures, and the use of radiology or MRI during the procedure. It should be noted that CSII pump catheter insertion site could alternatively be inserted into the back of arms or the upper buttock and thigh. Consideration should also be placed on whether or not the anesthesia provider has access to the pump during the procedure. If it is decided that CSII therapy will be used intraoperatively, care CSII Therapy in the Perioperative Period 49 should be taken as to secure the device so that the catheter set or the CSII pump becomes dislodged. A back up for insulin administration should be considered as a precaution should the CSII pump become inoperable. Need for More Research Although the previous recommendations for CSII therapy in the perioperative period were extrapolated from expert opinions, research in this area is minimal. Studies observing glycemic outcomes comparing CSII therapy and conventional perioperative management of T1DM would be helpful in identifying potential benefits or complications. If more studies were completed, specific guidelines could be establish that were evidence-based in practice. Attempts at research and reported case studies of CSII use in the perioperative period are clues that a knowledge gap has been identified. Fortunately, from research that is already known, critical thinking can be applied to CSII therapy in the perioperative period. This application of knowledge can help the anesthesia provider decide what is best for his or her patient who receives CSII therapy. As CSII therapy for the treatment of T1DM continues to grow, more research will be gathered to assist the decision making process. Chapter 13: References CSII Therapy in the Perioperative Period 50 1. U.S. Department of Heath & Human Sevices. Diabetes Overview. Bethesda, MD; Nov 2008. www.diabetes.niddk.nih.gov. Accessed Feb 1, 2012. 2. Pickup J. Insulin Pump Therapy and Continous Glucose Monitoring. Oxford University Press; 2009. 3. Lenhard MJ, Reeves GD. Continuous subcutaneous insulin infusion: A comprehensive review of insulin pump therapy. Arch Intern Med. 2001; 161:2293-2300. 4. Meneghini LF. Perioperative management of diabetes: translating evidence into practice. Cleveland Clinic Journal of Medicine. 2009; 76 (supp 4): S53-S59. 5. Jones RE, Brashers VL, Huether SE. Alterations of Hormonal Regulation. In: McCance KL, Huether SE, Brashers VL et al, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th Ed. Maryland Heights, MO: Mosby Elservier; 2010: 745-765. 6. Standard of Medical Care in Diabetes-2011: American Diabetes Association. Diabetes Care. 2011; 34: S11-S61. 7. National Diabetes Clearinghouse: Hypoglycemia. Bethesda, MD; Oct 2008. http://diabetes.niddk.nih.gov/dm/pubs/hypoglycemia/. Accessed Feb 1, 2012. 8. Mattila T, de Boer A. Influence of intensive versus conventional glucose control on microvascular and macrovascular complications in type 1 and 2 diabetes mellitus. Drugs. 2010; 70: 2229-2245. 9. Stetter C, Allemann S, Juni P, et al. Glycemic control and macrovascular disease in types 1 and 2 diabetes mellitus: Meta-analysis of randomized trials. American Heart Journal. 2006; 27-38. 10. Alsaleh FM, Smith FJ, Keady S, et al. Insulin pumps: From inception to the present and to the future. Journal of Clinical Pharmacology. 2010; 35: 127-138. 11. Pickup JC, Keen H, Parsons JA, Alberti KGMM: Continuous subcutaneous insulin infusion: an approach to achieving normoglycaemia. BMJ i:204–207, 1978. 12. Bode, B. Pumping protocol: A guide to insulin pump therapy initiation. Northridge, CA: Medtronic; 2008. 13. Weissberg-Benchell J, Antisdel-Lomaglio J, Seshardri R. Insulin pump therapy: A metaanalysis. Diabetes Care. 2003; 26: 1079-1087. CSII Therapy in the Perioperative Period 51 14. Pickup J, Keen H. Continous subcutaneous insulin infusion at 25 years: Evidence base for the expanding use of insulin pump therapy in type 1 diabetes. Diabetes care. 2002; 25: 593-598. 15. Jeitler K, Horvath K, Berghold T, et al. Continuous subcutaneous insulin infusion versus multiple daily insulin injections in patients with diabetes mellitus: systematic review and meta-analysis. Diabetologia. 2008; 51: 941-951. 16. Wall R. Endocrine Disease. In: Hines R, Marschall K. eds. Stoelting’s Anesthesia and Co-Existing Disease. 5th Ed. Philadelphia PA: Saunders Elsevier; 2008: 365-378. 17. McAnulty GR, Robertshaw HJ, Hall GM. Anesthetic management of patients with diabetes mellitus. British Journal of Anaesthesia. 2000; 85:80-90. 18. Akhtar S, Barash P, Inzucchi S. Scientific principles and clinical implications of perioperative glucose regulation and control. Anesthesia and Analgesia. 2010; 110: 478497. 19. Betts P, Brink S, Martin S, et al. Management of children and adolescents with diabetes requiring surgery. Pediatric Diabetes. 2009; 10:169-174. 20. Moghissi E, Korytkowski M, DiNardo M, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. 2009; 32:1119-1131. 21. White WA, Montalvo H, Monday JM. Continuous subcutaneous insulin infusion during general anesthesia: A case report. AANA Journal. 2004;72:353-357. 22. Groundine SB, Phan B. Significant hyperkalemia after discontinuation of an insulin pump. Journal of Clinical Anesthesia. 2005; 17:630-632. 23. Nassar AA, Boyle ME, Seifert KM, et al. Insulin pump therapy in patients with diabetes undergoing surgery. Endocrine Practice. 2012; 18:49-55. 24. Cook CB, Boyle ME, Cisar NS, et al. Use of continuous subcutaneous insulin infusion (Insulin pump) therapy in the hospital setting: Proposed guidelines and outcomes. The Diabetes Education. 2005; 31: 849-857. 25. Alexanian SM, McDonnel ME, Akhtar S. Creating a perioperative glycemic control program. Anesthesiology Research and Practice. 2011; 2011:1-9. 26. Marks J. Perioperative management of diabetes. American Family Physician. 2003; 67: 93-99. 27. Ahmed Z, Lockhart CH, Weiner M, et al. Advances in diabetic management: Implications for anesthesia. Anesthesia Analgesia. 2005; 100: 666-669. CSII Therapy in the Perioperative Period 52