Managing Critically Ill Patients: Are Other Clinicians Recognizing the
advertisement
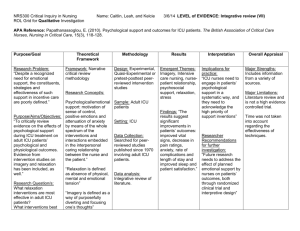
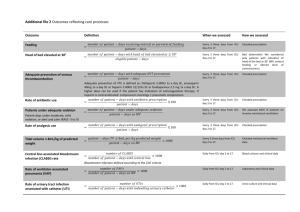
Managing Critically Ill Patients: Are Other Clinicians Recognizing the Difference Between Early Mobility and Early Rehabilitation? Course Learning Objectives After this session participants will be able to: A. Describe the present data examining the unique role that physical therapist services offer patients with critical illness being managed in the ICU. Patricia Ohtake 25 minutes B. Understand the vital clinical reasoning that is used in each interaction with patients with critical illness. Dan Malone 25 minutes C. Describe the contributions of physical therapists and physical therapist assistants in the functioning of interprofessional teams that go beyond direct patient care to enhance patient outcomes and effectively manage the cost of care. Mary Keehn 25 minutes D. Describe some areas of focus for future research on the role of physical therapist services for patients with critical illness. Jennifer Ryan 25 minutes Panel discussion 20 minutes Ohtake Outline: Rehabilitation for people in the ICU is known to be safe and feasible (Bailey et al., 2007; Morris PE et al., 2008; Schwieckert WD et al., 2009; Needham et al., 2010). As described in the literature, physical therapists in the intensive care setting function as the leader of interprofessional teams providing rehabilitation interventions to assist the patient in achieving their prior level of function. Furthermore, physical therapists have been successful in implementing ICU rehabilitation programs in their institutions (Clark DE et al., 2013; Engel HJ et al., 2013; Harris CL et al., 2014). Physical therapists are uniquely qualified to: determine patient readiness for rehabilitation interventions using evidence-based parameters and algorithms select the appropriate rehabilitation interventions prescribe the level of exercise intensity, duration, and frequency monitor and immediately adjust the rehabilitation intervention based on the patient’s responses What is the evidence for patient-centered outcomes resulting from ICU rehabilitation provided by physical therapists? OUTCOME MEASURE Days of Delirium Schweickert WD et al., 2009; Needham et al., 2010; Balas MC et al., 2014 Days of Mechanical Ventilation Schweickert WD et al., 2009; Balas MC et al., 2014; McWilliams D et al., 2014 Individuals being managed in the ICU who received physical therapist-led rehabilitation interventions experienced: ICU – medical, surgical Fewer days of delirium (~ 1- 2 days). ICU – medical, surgical Fewer days of mechanical ventilation (~2 days). ICU Length of Stay Clark DE et al., 2013; Engel HJ et al., 2013; McWilliams D et al., 2014 Hospital Length of Stay Titsworth et al., 2012; Clark DE et al., 2013; Engel HJ et al., 2013; McWilliams D et al., 2014 Ventilator-Associated Pneumonia Titsworth et al., 2012 Deep Vein Thrombosis Clark DE et al., 2013 Pneumonia Clark DE et al., 2013 Physical Restraints Titsworth et al., 2012 Physical Function Needham et al., 2010; Engel HJ et al., 2013; Harris CL et al., 2014; McWilliams D et al., 2014 Mortality Morris PE et al., 2011 ICU – medical, surgical, trauma and burns Fewer days in the ICU (~2 days). ICU - medical, surgical, trauma and burns, neuro Fewer days in the hospital (1 - 5 days). ICU – neuro Lower rates of ventilator-associated pneumonia [2.14 per 1000 ventilator days (pre-PT rehabilitation intervention period) down to 0 cases in a six month period of PT rehabilitation interventions even though there was no difference in number of ventilator days, % of patients ventilated, or compliance with the ventilation protocol} ICU – trauma and burns Decreased risk of deep vein thrombosis (33%) ICU – trauma and burns Decreased risk of pneumonia (21%) ICU – neuro Decreased use of physical restraints ICU – medical, surgical Increased independence in bed to chair transfers Increased % of patients able to perform sit-to-stand Increased % of patients able to ambulate Increased distance walked when ambulating Patients walk further when rehabilitation interventions are provided by physical therapists as compared to nurses. In a one year follow-up of 280 survivors of acute respiratory failure, individuals who did not receive ICU rehabilitation provided by a physical therapist were 77% more likely to experience death or readmission. Malone outline: Program Components of Rehabilitation Understand the vital clinical reasoning that is used in each interaction with patients with critical illness: Plans of Care Provided by Physical Therapists for Patients with Critical Illness (25 minutes) 1. Patient inclusion criteria 2. Physical therapy start & stop criteria o What does the research tell us? 3. Physical therapy examination – emphasis on outcome measures & ICF. For example, o Body structure & function: MRC score o Activity/task limitations: Mobility milestones; FIM/FSS-ICU; PFiTs; o Participation restrictions: SF-36 4. Delirium assessment o Richmond agitation sedation scale (RASS) o Cognitive assessment method for the ICU (CAM-ICU) 5. Example of mobility protocols o ABCDE Bundle Keehn outline: Describe the contributions of physical therapists and physical therapist assistants in the functioning of interprofessional teams that go beyond direct patient care to enhance patient outcomes and effectively manage the cost of care: Team Based Care in the ICU. Objectives for the segment• Identify important characteristics of the ICU context the defines team based care in the ICU • Describe the “Big 5” of teamwork – Eduardo Salas • Where doe PT fit in the ICU team - and how can we improve the fit? 1) The ICU within the US health care system - small # of beds but a big % of costs - important to achieve the Triple Aim 2) Team Based Care& Collaborative Practice contribute to achieving the Triple Aim 3) Care in the ICU is team based - core team, peripheral team members, internal & external consultants 4) Teamwork is managed through checklists, rounds, and protocols 5) What do we know about high functioning teams? - the Big 5 in teamwork (Salas) & coordinating mechanisms 6) Challenges to teamwork - power relationships, "fitting in", individual vs. team productivity 7) How do we ensure that critically ill patients benefit from PT - and that we have PTs who choose to work with them? Ryan Outline: Describe some areas of focus for future research on the role of physical therapist services for patients with critical illness: Where Should Future Research Focus to Further Define the Role of the Physical Therapist in the Management of Patients with Critical Illness? - - How should PLOF factor into determining a patient's need for early rehab versus early mobility? o Present research available versus where we need to investigate o Audience input Are certain physiological determinants of medical stability the most important to guide the intensity and duration of a therapy session? If so, which? o Present research available versus where we need to investigate What about those patients who have non-textbook responses, but it is OK? - - - o Audience input What role should symptoms play in the decision to increase or decrease the intensity and duration of a therapy session? Who makes the decision? o Present research available versus where we need to investigate Cardiac arrhythmias with versus without symptoms-what other signs should be considered? Ventilator settings Medication responses o Audience input What skills of a physical therapist augment a different experience for the patient that positively impacts functional outcomes? o Present research available versus where we need to investigate What design components should be included in a research project? o Audience input. What curricular components need to be enhanced to ready practitioners to be the professional who can bring forward the unique skills of early rehab to enhance early mobility initiatives? How should this be researched? o Where are we now? Present CAPTE requirements Present demand for continuing education Present NPTE o Audience input