Acute on chronic hyponatremia polydipsia 11072013
advertisement
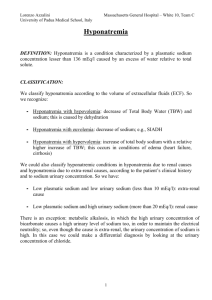
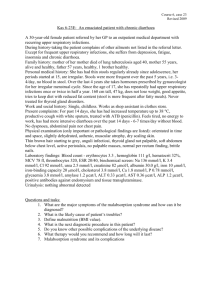
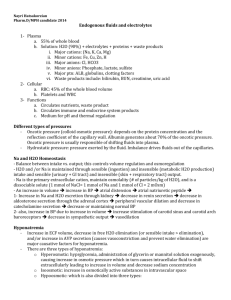
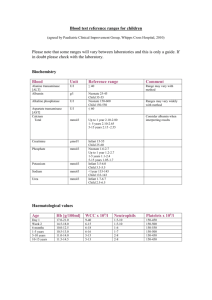
Extreme acute on chronic hyponatremia; polydipsia. MS van Zanten MD1, N Mullaart MD1 1. Emergency departement, Rode Kruis Ziekenhuis Beverwijk, the Netherlands 2. Emergency departement, Westfriesgasthuis Hoorn, the Netherlands Corresponding author: M.S. van Zanten Emergency department Rode Kruis Ziekenhuis Vondellaan 13 1942 LE, Beverwijk, the Netherlands E mail: msvanzanten@hotmail.com, n.mullaart@westfriesgasthuis.nl Total words: 798 Title words: 6 Abstract words: 40 Reference words: 175 Abstract We presented a 67-year old patient with an extreme hyponatremia, presumed acute on chronic, initialy with only few neurologic signs. The chronic hyponatremia was thought to be mainly due to psychogenic polydipsia, reinforced by the use of diuretics and malnutrition. Case presentation A 67-old male patient, came to our emergency department by ambulance after he was found, lying on the floor. Patient said he lost strength in both legs the evening before, fell down and could not get up. There was no other trauma, no head injury or amnesia. Patient denied any recent drug abuse. Beside absent strength in his legs, an active itching skin condition and some dysuria, patient had no other physical complaints. Patients premedical history consisted of a infragenual bypass, aortic bifurcation prosthesis, hypertension and alcoholabuses (till 2001). Besides thiazide, patient was on carbasalat calcium, benzodiazepine, simvastatin and omeprazole. On physical examination we saw a undernourished, dehydrated, shabby and slightly bradyphrenic man, with open pyoderma of the skin. Bloodpressure was 94/74 mmHg, with a pulse rate of 99 bpm. He had a GCS of 14, well orientated in person, place and time, with only minimal correctable visual hallucinations. Temperature 34.5 (ºC), Xthorax showed no abnormalities. Table 1 shows the laboratory results. The ECG only showed sinus tachycardia and urinary retention (1500cc) was found with bladder ultrasound. X-ray of the thorax showed no malignancy. Our patient was admitted to the ICU. Sodium was corrected [1] and thiazide was discontinued. On day two of admission, patient deteriorated neurologically to a GCS of 6. Because suspicion of pontine demyelinolysis, CT and MRI of the brain were done, but showed no intracranial pathology. The next day patient’s neurologic condition recovered. After further history taking, patient admitted recent low nutritional intake and polydipsia, 5-6 Liters H2O a day. After seven days patient was transferred to the ward. A psychiatrist will treat the patient further for possible polydipsia disorder [2]. Patient’s consciousness and renal function fully recovered. Problem list: 1) Extreme hyponatremia, most likely acute on chronic 2) Rhabdomyolysis as a result of hyponatremia and lying on the floor all night 3) Renal insufficiency. Most likely pre-renal (diuretics, dehydration) and post-renal (urinary retention). Infected open pyoderma 4) Bradyphrenia and mild delirium, conceivable due to problem 1, 2 and 3 5) Weakness in both legs, probably due to problem 1 List 1: problem list Discussion Polydipsia is defined as an excessive thirst and fluid intake. The patient drinks large amounts of fluid, which dilutes the extracellular fluid, decreasing its osmotic pressure. The body responds to this by decreasing the level of vasopressin (antidiuretic hormone), with a resultant polyuria. Polydipsia may be due to an organic lesion (both diabetes mellitus and insipidus, Cushing syndrome, SIADH) or have a psychological cause (psychogenic polydipsia, anorexia, anxiety, mouth dryness by medication use). Above mentioned, mostly combined, can lead to hyponatremia. It is important to note that hyponatremia usually never develop from just drinking much. The renal capacity for free water excretion is about 28 liters/day [3]. Psychogenic polydipsia is a multifactorial disease. The underlying pathophysiology of this syndrome is unclear, but malfunction of the hypothalamic thirst center is seen as a likely cause [2]. In a case study of patients with comorbid PPD and diabeters insipidus, chronic intake of excess fluid postulated to change feedback regulation of the hypothalamic-pituitary axis [4]. There are various other theories of polydipsia, including positive symptoms of schizophrenia, compulsive behavior, stress reduction and due to side effects of anticholinergic medication (like mouth dryness) [2]. PPD (psychogenic polydipsia) may lead to hyponatremia. Patients with an extreme hyponatremia may suffer from nausea, vomitting, confusion, loss of strength, disturbance of consciousness, seizures, apnea and asystole [5,6,7]. Looking at other causes in patients with hyponatremia, SIADH is an important co-founding. SIADH is a disorder in which water excretion is partially impaired because of the inability to suppress the secretion of ADH. Diuretics also are a major exacerbating factor in the hyponatremia. They will interfere with sodium resorption at the proximal tube, exacerbate sodium excretion, impair free water excretion and my lead to acute water intoxication [5,6,7]. For the cause of hyponatremia, urine sodium and urine/serum osmolality must be checked to differ between hypovolaemic-, normovolaemic- or hypervolaemic hyponatremia (see List 2). Diagnosis hyponatremia (i) Hypovolaemic hyponatremia (a) Urinary sodium > 20 mmol/L; diuretics, salt-losing nephropathy, Addison’s disease, glycosuria (b) Urinary sodum < 20 mmol/L; vomiting, diarrhea, pancreatitis (ii) Normovolaemic hyponatremia (a) Urine osmolality > serum osmolality; SIADH (due to drugs as carbamazepine, NSAID’s and antidepressants, pneumonia, COPD, CVA, neoplasia) (b) Urine osmolality < serum osmolality; beer potomania, psychogenic polydipsia, ‘tea and toast’diet. (iii) Hypervolaemic hyponatremia (a) Urinary sodium < 20 mmol/L; hypoalbuminaemia, congestive heart failure, cirrhosis, nephritic syndrome (b) Urinary sodium > 20 mmol/L; chronic renal failure, cerebral salt wasting, hypothyroidism List 2: diagnosis hyponatraemia While treating hyponatremia, normalisation of the sodium concentration should be slowly because of the risk of the development of pontine demyelinolysis. Precursors may include seizures, disturbed consciousness, gait changes, and decrease of respiratory function. When not well recognized, it can further lead to acute para- or quadraparesis, dysphagia, dysarthria, diplopia, loss of consciousness and other neurological symptoms associated with brainstem damage. Rapid myelinolysis of the corticobulbar and corticospinal tracts may lead to locked-in syndrome [8,9]. After restoring natrium concentration [1,7] in patients with polydipsia, long-term management includes fluid restriction and removal of exacerbating factors. Since there may be an association between the psychotic process and polydipsia/hyponatremia, there must be an attempt to treat patients psychiatric disorder. A combination of behavioral treatments and medication has been shown to be effective in de long term. Case reports describe positive effects with clozapine, low-dose risperidone and olanzapine. Also beta blockers as propranolol have been found to be effective [10]. Diuretics should be discontinued [3]. CRP Sodium (Sodium september 2011) (Sodium august 2011) (Sodium july 2011) (Sodium june 2011) Potassium Creatinine Alkaline phosphatase Creatine kinase Lactate Alcohol Plasma osmolality Arterial Blood Gas Urine sodium Urine sediment Urine osmolality Albumin Chloride Glucose Urea TSH / FT4 Table 1 178 mg/l 99 mmol/l (126 mmol/l) (113 mmol/l) (125 mmol/l) (126 mmol/l) 3.1 mmol/l 175 µmol/l 156 U/l 11289 U/l 3.7 mmol/l <0.1 0/00 233 mOsm/kg pH 7.44, pCO2 4.3 kPa, pO2 11.3 kPa, HCO3 21.7 mmol/l, sodium < 100 mmol/l 16 mmol/l Negative 35 g/l 71 mmol/l 8.4 mmol/l 13 mmol/l 0.55 mIU/l / 19 pmol/l Blood/urine test analyses References [1] Robert W. Schrier and Shweta Bansal. Diagnosis and management of hyponatremia in acute illness. Curr Opin Crit Care. 2008 December ; 14(6): 627–634. [2] Dundas B. et al. Psychogenic polydipsia review: etiology, differential, and treatment. Curr Psychiatry Rep.2007 June;9(3):236-41. [3] Illowsky B.P. and Kirch D.G. Polydipsia and hyponatremia in psychiatric patients. Am J Psychiatry 1988;145:675-683. [4] Fricchione G, Kelleher S, Ayyala M. Coexisting central diabetes insipidus and psychogenic polydipsia. J Clin Psychiatry. 1987;48:75-76. [5] Wakil A, Ng JM and Atkin S. Investigating hyponatremia. BMJ 2011;342:d1118 [6] Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med 2000; 342:1581. [7] Lidner G, Schwarz C. An update on the current management of hyponatremia. Minerva Med. 2012 Aug;103(4):279-91. [8] Martin RJ. Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry 2004; 75 Suppl 3:iii22. [9] Musana AK, Yale SH. Centrale pontine myelinolysis: case series and review. Wisconsin Medical Journal 2005;104(6):56-60. [10] Verghese C, de Leon J, Josiassen RC. Problems and progress in the diagnosis and treatment of polydipsia and hyponatremia. Schizophr Bull 1996;22:455-464.