Hyponatremia - HUG
advertisement

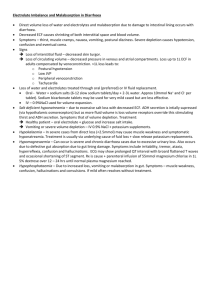
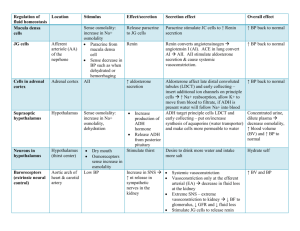
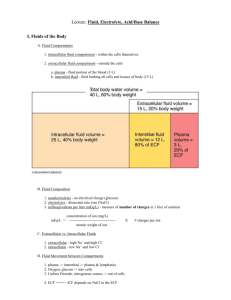
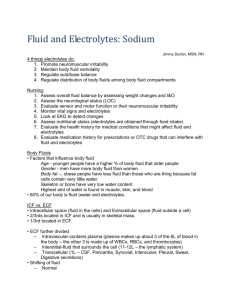
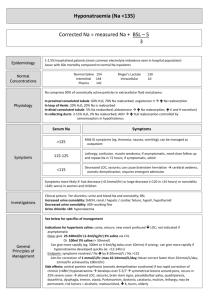
Hyponatremia in neonatology Kirsten L Brunsvig 03.05.10 Sodium • Dominating cation in the ECF • Princible determinant for extracellular osmolality – Necessary for the maintenance of intravascular volume. • Unique among electrolytes because water balance, not sodium balance, usually determines its concentration. Total body water • Distribution of body water – Extracellular fluid • Intravascular • Interstitial – Intracellular fluid • 40 SA – Total body water = 75% of body weight – ECF = 45 % of total body water • 27 SA – Totale body water = 80% of body weight – ECF = 70% of total body water Water loss • Preterm infants have greater weight loss (1015% vs 5%), associated with increased diuresis, comparet to term infants. • Water loss: – Kidneys – Skin • Large insensible water loss, especially in the ELBW infants with very thin skin – Lungs • Decreases with increasing GA, but less important than skin water loss. – Other (stoll, gastric drainage, thoracostomy) [Na] regulation • [Na] thirst and ADH water intake/retention and normalization of [Na] • [Na] decreased ADH water loss and normalization of [Na] • However, volume depletion takes presendence over osmolality and causes increase in ADH even if the patient has hyponatremia. • Also, excretion of Na in the kidneys is not regulated by osmolality, but plasma volume and a variety of regulatory systems. Mechanism of hyponatremia • Dilutional (most common in the neonate) • Excessive Na+ loss • Na+ deficiency Differential diagnoses • Volume overload – Too much volume given – Congestive heart failure – Renal/liver failure – Paralysis with fluid retention – Diluted formulas Differential diagnosis • Increased Na+ loss – VLBW: renal tubular Na+ losses high – Salt-losing nephropathies – GI-losses – Skin losses – 3rd space (e.g. NEC) – Adrenal insufficiency • Mineralocorticoid deficiency => metabolic acidosis and shock Na, K, Differential diagnosis • Inadequate Na+ intake – Normal: 2-4mmol/kg/j • Drug induced – Diuretics – Indomethacine can lead to H2O retention – Opiates, carbamazepine, barbiturates can cause SIADH – Mannitol/hypertonic glucose can cause hyperosmolarity with salt wasting. Differential diagnosis • SIADH = syndrome of inappropriate ADH secretion – CNS disorders (IVH, hydrocephalus, asphyxia, meningitis) – Lung diseases – Critically ill preterm and term neonates Patient with hyponatremia • Important questions – Seizures? (<120mmol/l) –urgency! – How much Na and free water is the patient receiving? – Weight gain or weight loss? – Urine output? – Renal salt-wasting medication? Clinical examination • • • • Complete examination Seizures? Oedema? Decreased skin turgor/ dry mucous membranes as signs of dehydration? • Weight gain/loss • Fluid intake/output over 24hours Further tests • S-Na, S-Osmolality • U-Na, U-osmolality, U-specific gravity • S-electrolytes, S-creatinin, S-total protein to evalue renal function Laboratory findings Urine output U-Na U-osmol U-spec grav. Increased Increased Decreased Decreased Skin/GI loss, 3rd spacing Decreased Decreased Increased Increased SIADH Decreased Decreased Increased (>S-osmol) Increased Excess i.v. fluid Increased Decreased Decreased Heart failure / fluid retention Decreased Rénal loss (diuretics, adrenal insufficiency) Increased Treatment • Seizures: emergency – NaCl 3% – Total body Na-deficit/2 over 12-24 hours Rapid corrections may result in brain damage. [Na] deficit x weight (kg) x 0.6 Total body water = 60-75% of weight Usually use 60% to minimize the likelihood of overly rapid correction [Na] deficit = [Na] desired – [Na] patient Treatment • Volume overload – Fluid restriction • usually by 20ml/kg/d – S-NA every 6-8h – Treat underlying cause • Inadequate intake of Na – 2-4 mmol/kg/d, increased in premature • Increased Na-losses – Treat underlying cause – Increase Na-intake Treatment • Drug induced (e.g. Furosemid) – Increase intake may be required – Indomethacin • Treated with fluid restriction • SIADH – Restrict fluids, – Furosemide can be tried. Long term prognosis • Hyponatremia has been associated with adverse neurological developmental outcomes. – Increased risk of cerebral palsy – Increased risk of hearing loss • Large variations in Na have also been found associated with impaired functional outcomes at 2 years.