Case history of patient with malabsorption syndrome
advertisement
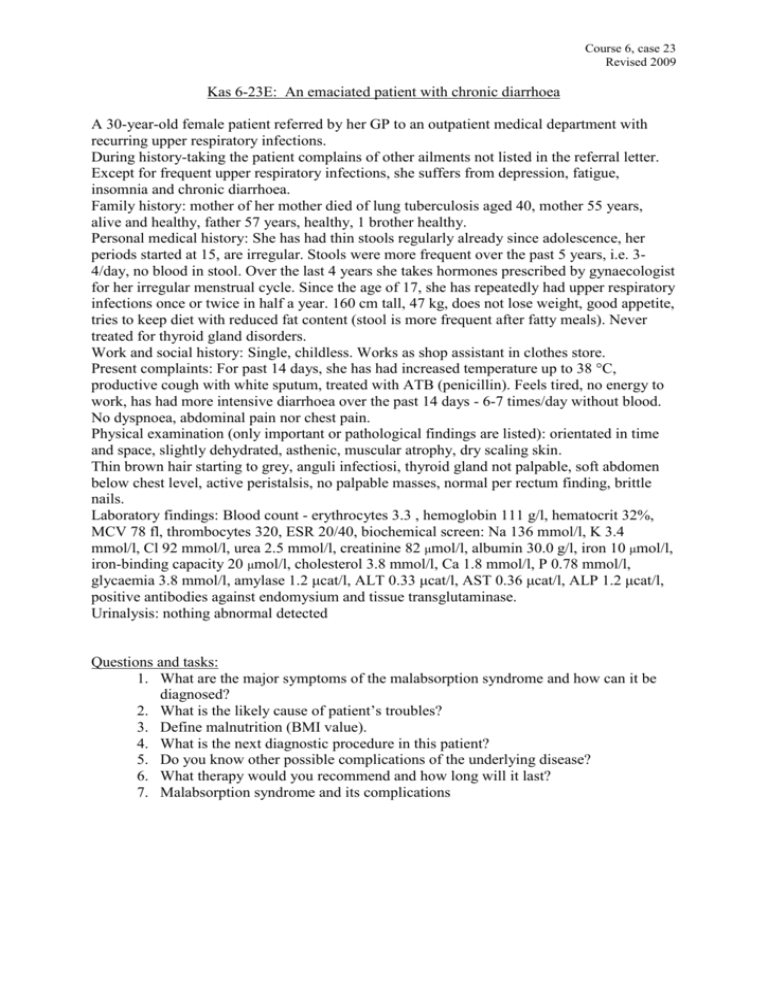
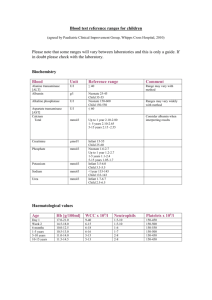
Course 6, case 23 Revised 2009 Kas 6-23E: An emaciated patient with chronic diarrhoea A 30-year-old female patient referred by her GP to an outpatient medical department with recurring upper respiratory infections. During history-taking the patient complains of other ailments not listed in the referral letter. Except for frequent upper respiratory infections, she suffers from depression, fatigue, insomnia and chronic diarrhoea. Family history: mother of her mother died of lung tuberculosis aged 40, mother 55 years, alive and healthy, father 57 years, healthy, 1 brother healthy. Personal medical history: She has had thin stools regularly already since adolescence, her periods started at 15, are irregular. Stools were more frequent over the past 5 years, i.e. 34/day, no blood in stool. Over the last 4 years she takes hormones prescribed by gynaecologist for her irregular menstrual cycle. Since the age of 17, she has repeatedly had upper respiratory infections once or twice in half a year. 160 cm tall, 47 kg, does not lose weight, good appetite, tries to keep diet with reduced fat content (stool is more frequent after fatty meals). Never treated for thyroid gland disorders. Work and social history: Single, childless. Works as shop assistant in clothes store. Present complaints: For past 14 days, she has had increased temperature up to 38 °C, productive cough with white sputum, treated with ATB (penicillin). Feels tired, no energy to work, has had more intensive diarrhoea over the past 14 days - 6-7 times/day without blood. No dyspnoea, abdominal pain nor chest pain. Physical examination (only important or pathological findings are listed): orientated in time and space, slightly dehydrated, asthenic, muscular atrophy, dry scaling skin. Thin brown hair starting to grey, anguli infectiosi, thyroid gland not palpable, soft abdomen below chest level, active peristalsis, no palpable masses, normal per rectum finding, brittle nails. Laboratory findings: Blood count - erythrocytes 3.3 , hemoglobin 111 g/l, hematocrit 32%, MCV 78 fl, thrombocytes 320, ESR 20/40, biochemical screen: Na 136 mmol/l, K 3.4 mmol/l, Cl 92 mmol/l, urea 2.5 mmol/l, creatinine 82 μmol/l, albumin 30.0 g/l, iron 10 μmol/l, iron-binding capacity 20 μmol/l, cholesterol 3.8 mmol/l, Ca 1.8 mmol/l, P 0.78 mmol/l, glycaemia 3.8 mmol/l, amylase 1.2 μcat/l, ALT 0.33 μcat/l, AST 0.36 μcat/l, ALP 1.2 μcat/l, positive antibodies against endomysium and tissue transglutaminase. Urinalysis: nothing abnormal detected Questions and tasks: 1. What are the major symptoms of the malabsorption syndrome and how can it be diagnosed? 2. What is the likely cause of patient’s troubles? 3. Define malnutrition (BMI value). 4. What is the next diagnostic procedure in this patient? 5. Do you know other possible complications of the underlying disease? 6. What therapy would you recommend and how long will it last? 7. Malabsorption syndrome and its complications