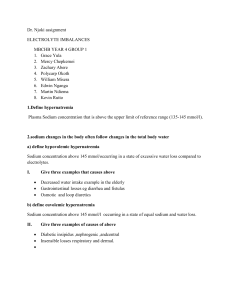
HYPONATREMIA
advertisement

HYPONATREMIA & HYPERNATREMIA DR. HAMED SHAKHATREH NEPHROLOGIST CONSULTANT DR. HASSAN MANSOUR NEPHROLOGIST HYPONATREMIA Normal S. Sodium 135-148 mmol/L <135 = 22% of hospital patients <130 = 4% of hospital patient Hyponatremia important because: 1. Acute hyponatremia cause morbidity & mortality 2. Mild hyponatremia can progress to severe during treatment 3. Rapid correction can produce severe neurological deficits and death. Hyponatremia and hypoosmolality are usually synonymous because the calculated osmolality. P osm = 2 Na + glucose mmol/L + BUN mmol/L The normal range 275- 295 Hyponatremia = hypoosmolality except in 3 conditions: 1. High proteins 2. High glucose 3. High Lipids Here the hyponatremia called pseudohyponatremia because the true sodium is normal if it measure by ion specific electrode not by photometry. For example: S. glucose 500mg/dl & S. Na 125mmol/L The true Na= 125 + (4x2.4) 135 mmol/L PATHOGENESIS: Depletion (primary decrease in total body solute + secondary water retention) 1. Renal solute loss Diuretic use Solute diuresis (Glucose, Mannitol) Solute wasting nephopathy Mineralocorticoid deficiency 2. Non renal solute loss Gastro intestinal (diarrhea, vomiting, pancreatitis, bowel obstruction) Cutaneous (sweating, burns) Blood Loss Dilution (primary increase in total body water + secondary solute depletion). 1. Impaired renal free water excretion a. Increased proximal reabsorption Hypothyroidism b. Impaired distal dilution SIAD Glucocorticoid deficiency c. Combined increased proximal reabsorption and impaired distal dilution CHF Cirrhosis Nephrotic syndrome d. Decreased Urinary solute excretion Beer Potomania 2. Excess water intake Primary polydipsia Dilute infant formula Differential Diagnosis: 1. Decreased volume (hypovolemia) 20% orthostatic changes Decreased urine sodium <30 non renal cause: G/E Increase urine Na >30 renal cause Diuretic the most common cause & Thiazide the common. Low S.K indicate hypovolemia Chronic interstitial nephropathy PKD, Bartter’s Syndrome, Addison’s Disease. EUVOLEMIA 33% Bp & Ps without orthostatic changes BUN & Uric Acid normal or low urine sodium <30 unlikely due to primary dilutional except in hypothyroidism. While Urine Na >30 = SIAD Criteria to Diagnose SIAD: Essential: 1. Decreased osmolality P. <275 2. Inappropriate urine osmolality urine >100mo/kg. H2O with S. hypoosmolality 3. Clinical Euvolemia 4. Increased urine Na on normal salt & water intake 5. Absence of causes of hypoosmolality such hypothyroidism, Addison’s disease and diuretics. SUPPLEMENTAL: 6. Abnormal water load 20ml/kg over 4 hours. Failure to dilute U osm <100 7. AVP inappropriately elevated relative to plasma hypo osmolality. 8. S. Na improved with water restriction but not with volume expansion. COMMON CAUSES OF SIAD - Tumors Pulmonary, GIT, Prostate Uterine Leukemia - Central NS disorders Tumors, Abscess encephalitis, Meningitis - Drug Induced Stimulated Nicotine, Phenothiazine Tricyclics and others - Pulmonary Disease TB, Aspergillosis, COPD Increased ECF (Edema & Ascites 35%) Clinical edema or ascites Na <30 mmol Sometimes Na >30 mmol/L because of glucosuria, diuretic theraphy. Hyponatremia usually in advanced disease as CHF, Nephrotic syndrome and Cirrhosis. CLINICAL MANIFESTATION Clinical picture depends on severity, speed of hyponatremia which means more than 48 hours or less. The picture reflect brain edema which presented from confusion to seizures to coma and the comorbilities. Special high incidence of morbidity & mortality in menstruating females & young children specially post operative. THERAPY Theraphy depends on severity of clinical situations, the level of S. Na, the period of which hyponatremia happened less than 48 hours or longer. Any correction not allowed more than 12 mmol/L in any 24 hours. Safe level >120 restrict water. Rapid correction induced pontine & extra poutine myelinolysis. How to correct hyponatremia (infusate- actual)% (BW/2+1) or hypertonic saline 3%- 70ml/hr in 70kg patient increase S. Na by 1. SIAD – Demeclocyline 600mgx2 to induce NDI. Phenytoin, Opiates, Ethanol- decreased AVP. HYPERNATREMIA Decreased in total body water, however total body Sodium maybe normal, increased or decreased. Hypernatremia happened in 2% of patients. Hypernatremia presented in two ways: Pre- Hospital or Intra-hospital. REGULATION OF WATER HOMOESTASIS: This happened by the interaction of AVP in the Hypothalamus through posterior pituitary gland & the thirst centre in the anterior wall of third ventricle with the distal collecting duct in the kidney. Osmostat in the hypothaleum proportionally affected by osmolality decreased osmolality decreased AVP. Thirst center regulated with 5 mml/kg above osmostat. PATHOPHYSIOLOGY: Hypernatremia happened with thirst sense lost or unable to get water. Defects in Thirst: 1. Primary- Hypodypsia Hypothalamic lesion Trauma Craniopharyngioma or Supracellular Tumor Metastatic Tumor Granulomas Vascular Lesion Essential Hypernatremia Geriatric Hypodypsia 2. Secondary- Cerebravascular Disease Dementia Delirium Mental Status Changes CLINICAL MANIFESTATION: Picture of hypernatremia mostly neurological and appear as confusion, seizures up to coma due to brain shrinkage & dehydration and also depends on the speed of appearance and state of hyperosmolality. CLINICAL CLASSIFICATION: Classifications according to changes in extra cellular volume. Pure Water Deficit DI – hypothalamic Nephrogenic Hypotenic Fluid Loss Renal GastroIntestinal Cutaneous Hypertonic Sodium Gain Salt Ingestion Hypertonic Sodium Chloride Hypertonic Sodium Bicarbonate Total parenteral nutrition Hypothalamic DI - Pituitary Surgery - Head Trauma - Neoplasia - Vascular Lesion Sheehan’s syndrome - Infection - Granulomas - Autoimmune Nephrogenic DI - Drug Induced Lithium Demeclocycline Amphotrecin B - Electrolyte disturb Hypercalcemia Hypokalemia - Obstructive uropathy - Congenital X-linked TREATMENT The treatment of hypernatremia is water. Water deficit = 0.6 BW (Na/140-1) Rapid correction not allowed only 0.5 mmol/L S. Na reduced in hour. Rapid correction cause intra cranial hemorrhage CDI- treated by AVP NDI- treated by Thiazide Amiloride If hypernatremia with overload & comorbility such as renal failure- hemodialysis is necessary.