file
advertisement

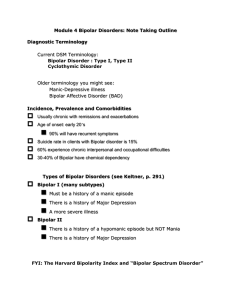
Bipolar Disorder Description: Bipolar disorder (or bipolar affective disorder, or manic depressive illness) is a Mental disorder characterized by episodes or both mania and major depress (Bipolar depression)(2) Classification: 1. Mania 2. Hypomania 3. Mania or Hypomania with episode of depression(1) Diagnosis: A. Sign & Symptom: i. Periods of Hypomania/Mania with: 1. 2. 3. 4. 5. 6. 7. Increased energy and activity Elevated mood or irritability Rapid speech Loss of inhibitions. Decreased need for sleep Increased importance of self The patient may be easily distracted. ii. The patient may also have periods of depression with: 1. Low or sad mood 2. Loss of interest or pleasure. 3. Loss of energy iii. The following associated symptoms are frequently present: 1. 2. 3. 4. 5. 6. Disturbed sleep Poor concentration Guilt or low self-worth Disturbed appetite Fatigue on loss of energy Suicidal thoughts on acts. iv. Either type of episode may predominate. - In severe cases, patients may have hallucinations (hearing voices, seeing visions) or delusions (strange or illogical beliefs) during periods of mania on depression.(2) B. Differential Diagnosis:: Alcohol or drug use may cause similar symptoms. If heavy alcohol or drug use is present, substance uses disorders.(2) Management: 1) Non pharmacological (Psychosocial ) treatment a) During depression, ask about risk of suicide: (Has the patient frequently’ thought of death or dying?) Does the patient have a specific suicide plan? Has he/she made serious suicide attempts in the past? Can the patient be sure not to act on suicidal ideas?) Close supervision b family or friends may he needed Ask about risk of harm to others (see Depression). b) During manic periods: Avoid confrontation unless necessary to prevent harmful or dangerous acts Advise caution about impulsive or dangerous behavior Close observation by family members is often needed If agitation or disruptive behavior is severe, consider hospitalization 2) Pharmacological (Biological) Treatment: If patient displays agitation, excitement on disruptive behaviour, antipsychotic medication may be needed initially (e.g., haloperidol 2—5mg up to three times a day or chlorpnomazine 100—200mg up to three times a day). The dose should be the lowest possible for the relief of symptoms, though some patients may require higher doses, if antipsychotic medication causes acute dystonic reactions (muscle spasms) on marked extrapyramidal symptoms (stiffness, tremors). Antiparkinsonian medication (e.g.,Bipridine 2-5mg 2-3 times daily or trihexephnedyl 2-5 mg 2 -3 times daily) may be helpful. Routine use is not necessary. Benzodiazepines may also be used in conjunction with neuroleptics to control acute agitation (e.g., Diazipam 2-5-10-20 mg up to four times a day). Carbamazepine and Valproate can prevent episodes from recurring. These should be continued for at least six months after symptoms resolve (longer-term use is usually necessary to prevent recurrences). Antidepressant medication is often needed during phases of depression but can precipitate mania when used alone (see Depression)(2) . Referral: Symptoms are severe or patient is disturbed There is a suicide attempt or risk of suicide There is possible associated physical illness Initial treatment was not effective Psychotic symptoms are persistent(1) Prevention: - Prophylactic treatment: Some anticonvulsants have mood stabilizing property and can be used for treatment of bipolar disorder. - Valproic acid: 500 to 750 mg daily; lower dosages may be used in hypomania. Sometimes it is appropriate to give as a single bedtime dose; otherwise twicedaily dosing. - Carbamazepine: 200 to 600 per day; Starting with small doses increase by 200 mg daily every 2 to 4 days , it is appropriate to give a single bedtime dose; otherwise, twice-daily dosing. - Severe Mental Disorders or Psychotic disorders eg Post Partum Psychosis acute psychosis, schizophrenia - Treatment with mood stabilizers requires periodic laboratory tests, initially to monitor the patient's response to the drug(2) Patient’s instructions: 1) General advise to the patient and family: - Educating patient and family members about features and nature of the illness And the importance of compliance with therapy. - Setting limits on impulsive behavior in patients with mania which can be discussed in family meetings(2) 2) Medication instructions: 1. 2. 3. 4. 5. 6. 7. 8. 9. Discuss treatment plan with patient Antipsychotic drugs should be chosen after considering their relative side effects Use only one antipsychotic drug at a time with a mood stabilizer Start low - go slow Use minimum dose required to maintain remission and avoid side effects Monitor symptoms and side effects Switch to another AP if symptoms does not respond to adequate dose in 4 weeks Start mood stabilizer with antipsychotic After acute episode discontinue antipsychotic (1) 3) Follow-up instructions: - Doctor should monitor the patient for signs of psychosis, mood swings, violence and self-harmful behaviors and most important for psychosocial interventions. - When the patient's condition has become stable, the doctor may not need to see the patient as often, although the frequency of follow-up visits depends on the course of the illness, the patient's adherence to treatment, medication requirements, the need for ongoing psychotherapy and patterns of care in a particular geographic area.(2) References: 1. 2. Professional Package For Medical Doctors for Mental Health Working in the BPHS in Afghanistan pages 69-71 MoPH 2009 Mental Health in Primary Care based on the WHO PHC Guide lines pages 160-163 WHO 2010