Bipolar Disorders - Austin Community College
advertisement

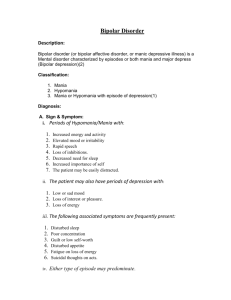
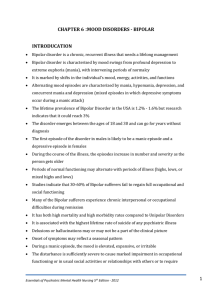
Module 4 Bipolar Disorders: Note Taking Outline Diagnostic Terminology Current DSM Terminology: Bipolar Disorder : Type I, Type II Cyclothymic Disorder Older terminology you might see: Manic-Depressive illness Bipolar Affective Disorder (BAD) Incidence, Prevalence and Comorbidities Usually chronic with remissions and exacerbations Age of onset: early 20’s 90% will have recurrent symptoms Suicide rate in clients with Bipolar disorder is 15% 60% experience chronic interpersonal and occupational difficulties 30-40% of Bipolar have chemical dependency Types of Bipolar Disorders (see Keltner, p. 291) Bipolar I (many subtypes) Must be a history of a manic episode There is a history of Major Depression A more severe illness Bipolar II There is a history of a hypomanic episode but NOT Mania There is a history of Major Depression FYI: The Harvard Bipolarity Index and “Bipolar Spectrum Disorder” Comparison of Mania and Hypomania MANIA A Manic Episode may happen suddenly, with little warning. or, may be preceded by a longer period of hypomania Mood/affect: Euphoric and/or Hostile, may be argumentative, aggressive Rapidly changing or alternating = labile Activity: Hyperactive: too busy to eat or sleep Disorganized activity Speech: pressured, hyperverbal, loud Cognition: Poor judgment and impulse control: esp. with rewarding activity AEB: Loud clothing, excessive make-up, promiscuity, excessive spending Flight of ideas, tangential, loosening of associations Delusions of grandeur, persecution HYPOMANIA Similar to Mania But to a Lesser Degree Energetic; less need for sleep Meets criteria for both Mania and Major Depression Increased goal-directed behavior: may be highly productive Mood: elevated or irritable Lowered inhibitions No delusions or hallucinations Bipolar I: Mixed Episode Rapidly alternating moods Not caused by drugs or alcohol Client is miserable, may be highly suicidal and/or may be violent CYCLOTHYMIC DISORDER (aka Cyclothymia) Frequent episodes of hypomania and numerous periods of depressed mood Chronic: Never symptom free Manic Behaviors that Result in Altered Relationships Manipulation Find vulnerability in others Exploit weaknesses and create conflict Shift responsibility Limit testing Denial of illness Abusiveness Biologic Theories of Mania and Bipolar Illness Ion dysregulation: oversensitivity of neuron to stimuli Alteration in transcription of messengers in nerve cell nucleus Neurotransmitters involved in mania/bipolar disorders: Excessive Dopamine and Norepinephrine availability of GABA and Serotonin NURSING DIAGNOSES FOR MANIA Risk for Violence (Directed toward self, others) Insomnia or Sleep Deprivation Altered Nutrition: Less than Body Requirements Acute Confusion Disturbed Thought Processes Impaired Social Interaction Ineffective family coping INTERVENTIONS: Psychotherapeutic Management (Focus of presentation is primarily on management of mania except where otherwise noted) Nurse-Patient Relationship and Communication Matter-of-fact tone Clear, concise directions Set firm limits Avoid power struggles De-escalate the client Communication techniques Focusing and redirecting Milieu Management Maintain safe environment Issue: milieu balance Reinforce appropriate hygiene and dress Consistency among staff Reduce environmental stimuli Support adequate Nutrition and Sleep Provide outlets for excessive energy level Psychotherapeutic Management: Medications A Common Diagnostic Mistake Diagnosing Major Depressive Disorder when the client is in the Depressive Aspect of Bipolar Disorder Giving an antidepressant can push the client into Mania Medications for Mania: Antipsychotics Atypicals*: e.g. olanzepine: Zyprexa, quetiapine: Seroquel, ziprasidone: Geodon, risperidone: Risperdal and Risperdal Consta, aripiprazole: Abilify are FDA approved mood stabilizing agents. Used alone or with other mood-stabilizing agents (*Excluding clozapine/Clozaril) Lithium: Drug of Choice Mechanism of action unknown: similarity to action of Na /replaces cellular Na Slow onset: 2 weeks Narrow range of therapeutic level 0.6 to 1.2 mEq/L; the optimum maintenance level is 0.8 mEq/L Toxic over 1.5 mEq/L “Usual side effects”- weight gain, fine hand tremor, nausea, metal taste Lithium Toxicity Narrow therapeutic range: therapeutic dose is close to a toxic dose. Mild to Moderate toxic reactions: 1.5 to 2 mEq/L Diarrhea Vomiting Drowsiness Muscular weakness Lack of coordination Dry mouth Moderate to Severe reactions: 2 to 3 mEq/L All previous symptoms & Ataxia Tinnitus Blurred vision High urinary output (osmotic diuresis) Delirium Nystagmus Severe reactions: than 3 mEq/L All previous symptoms Seizures Organ failure Renal failure Coma Death Mood Stabilizing Medications: Anticonvulsants valproic acid/divalproex: Depakote and Depakene carbamazepine: Tegretol Side effects: many drug interactions; CNS effects; blood disorders ( RBC, bone marrow, WBC’s), liver failure; toxic reactions common Monitoring of serum levels is necessary Other Anticonvulsants topiramate: Topamax gabapentin: Neurontin oxcarbazepine: Trileptal lamotrigine: Lamictal-best for bipolar depression. May cause severe rash. PRN and Emergency Medications Treatment of Acute Agitation or Aggression/Violence Sedating antipsychotic agent and/or Benzodiazepine: lorazepam (Ativan), clonazepam (Klonipin) May also use “cocktail” with addition of Benadryl Patient and Family Teaching Manage lifestyle factors and stress: Regular sleep/activity schedules Early recognition of changes in mood; seeking help Meds: Regular blood draws, Non-adherence issues Referrals, Resources Self-help groups: e.g. Depression and Bipolar Support Group Family: NAMI, family support groups Comorbid Disorders: Treat substance abuse