Psych Exam 2 Outline: Schizophrenia, Depression, Bipolar
advertisement

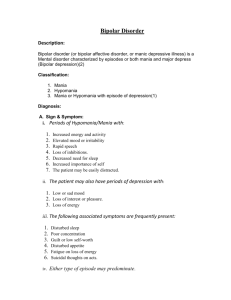
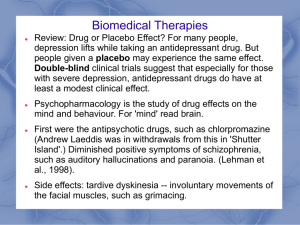
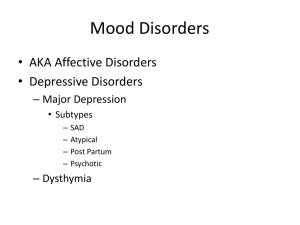
***Please see last page note before editing*** Psych Exam 2 Outline Schizophrenia ● ● ● disorder characterized by personality disorganization, impairment in social functioning & loss of contact with, or distortion of reality (hallucinations & delusions). Considered the major mental illness Comprises most of the inpatient population ● 4 phases of development ● Phase 1 (Premorbid Phase) ● ● ● ● ● ● Phase 2 (Prodromal Phase) ● ● ● ● ● ● ● not specific symptoms quiet, passive introverted children social maladjustment socially withdrawn irritable withdrawing further possible paranoid ideation may begin to self medicate functional impairments begin positive symptoms (perceptual abnormalities / suspiciousness) provide early interventions to avoid psychosis! Phase 3 (Schizophrenia) ● ● ● ● most intensive stage! often times where we first see the Pt Positive Symptoms (Excess or distortion of normal function) ● refers to symptoms that most individuals do not normally experience but are present in schizophrenia ● experiencing things others do not ● ex: hallucinations | delusions | thought disorders | movement disorders | word salad | flight of ideas | clang associations | Negative Symptoms (A deficit of function) ● lose the ability to do or feel things that are present in schizophrenic persons but are NOT normally found in healthy persons ● symptoms that reflect the loss or absence of normal traits or abilities. ● contribute more to poor quality of life, functional disability & the burden of others. ● these symptoms tend to stay ● ex: no emotion | just doesn’t care | loss of interest in everyday activities | lack emotion | neglect of personal hygiene | social withdrawal | PHASES OF SCHIZOPHRENIA(within this 3rd stage of development) ● ACUTE-onset or exacerbation of symptoms ● STABILIZATION- symptoms are diminishing, movement toward previous lvl of functioning ● MAINTENANCE-at or near baseline functioning ● Phase 4 (Residual Phase) ● ● ● ● may not need to be in the hospital follows an active phase of the illness symptoms of the acute stage are absent or no longer prominent negative symptoms may remain Major Depressive Disorder ● ● ● ● ● persistently depressed mood lasting a minimum of 2 weeks symptoms include: fatigue, sleep disturbances, changes in appetite, feelings of hopelessness or worthlessness, persistent thoughts of death or suicide, inability to concentrate or make decisions, change in physical activity leading cause of disability in the US Signs & Symptoms: ● Loss of Energy ● Self-loathing ● Reckless behavior ● Concentration Problems ● Somatic - Unexplained aches and pains Relationship between Depression & Medical illness - depression may present with physical symptoms / problems, rule out the physical problems first. DO not just assume someone is depressed. Persistent Depressive Disorder (Dysthymia) ● ● ● Sad no evidence of psychotic symptoms essential feature is chronically depressed mood for most of the day for at least 2 years Premenstrual Dysphoric Disorder (PDD) ● ● Symptoms: depressed mood | anxiety | mood swings | decreased interest in activities | symptoms begin during week prior to menses, start to improve within a few days after the onset of menses, and become minimal or absent in the week post-menses. Nursing Diagnosis in Depression ● ● ● ● ● ● ● ● Safety is priority diagnosis!! Risk for suicide complicated grieving low self esteem powerlessness social isolation disturbed thought process self-care deficit ECT - Electroconvulsive Therapy ● ● ● ● ● ● ● ● ● ● ● ● ● ● induction of a grand mal seizure through application of electrical current to the brain. Indications: Major Depression, Bipolar-mania, Schizophrenia duration of seizure should be 15-25 seconds 6-12 treatments place Pt side lying after ECT! Assess for suicide even after ECT! Only absolute contraindication for ECT is increased intracranial pressure from brain tumor, recent CVA, or other cerebrovascular lesion. Most common side effect is temporary memory loss and confusion Nurse must ensure informed consent has been granted by the MD! Nurse must assess mood, level of anxiety, thought and communication patterns, and vital signs. Nurse helps to orient Pt to time and place after procedure and what has occurred Nurse monitors vitals every 15 minutes for the first hour MOA: ECT increases the circulating level of neurotransmitters Dopamine, Serotonin, Norepinephrine, Glutamate, GABA Nursing Responsibilities: Safety & Manage Anxiety! Transcranial Magnetic Stimulation ● ● ● ● Noninvasive therapy that uses magnetic pulsations to stimulate the cerebral cortex of the brain only indicated in Major Depressive Disorder Frequency of treatment - everyday for 4 - 6 weeks. Relatively safe / no anesthesia ● Most anti-depressive agents take 2-6 weeks to act! Bipolar / Mood Disorders ● ● ● manifested by cycles of mania and depression characterized by mood swings from profound depression to mania with periods of normalcy delusions or hallucinations may or may not be part of clinical picture Manic Episode ● ● ● ● This is NOT caused by any substances or medical condition. period of abnormally and persistent elevated, expansive or irritable mood. more talkative / rapid pressured speech flight of ideas / racing thoughts Hypomania ● ● ● ● ● ● It is a milder form of mania may emerge after antidepressant therapy or ECT period of abnormally and persistent elevated, expansive or irritable mood decreased need for sleep increase goal direction or psychomotor agitation unrestrained buying sprees, sexual indiscretions / foolish business decisions Bipolar I ● ● ● ● Experience manic episodes or more manic episodes may have depressive episodes 1st episode of Mania, hypomania, mixed (recurrent mood episodes) psychosis or catatonia may be present Bipolar II ● ● ● Recurrent MDD with hypomania never experienced a full manic episode psychosis or catatonia may be present Planning Care (nursing approaches) ● ● ● ● Acute Phase ● medical stabilization ● maintaining safety ● self-care needs Continuation Phase ● maintain medication adherence ● psychoeducational teaching ● referrals Maintenance Phase ● prevent relapse Main diagnosis in Mania and Depression = SAFETY!!! Suicide - Prevention & Protective Factors ● ● ● Most at risk for suicide = Most specific / Lethal Plan! suicide is not a diagnosis but rather a behavior Risk Factors: ● marital status - single 2x> married person / divorced, separated or widowed 4-5x> risk than married ● males over 80 years old are at greatest risk ● previous suicide attempt ● co-occuring mental disorders ● substance abuse disorders ● experiencing a loss - death, marriage, job etc. ● family history of suicide, mental illness, substance abuse / dependency ● family violence - physical / sexual abuse ● psychiatric hospitalization in the last year ● feelings of hopelessness ● impulsive / aggressive tendencies ● incarceration ● physical illness consisting of extreme pain, loss of function, or poor diagnosis Suicide Risk Assessment ● Demographics | presenting symptoms | medical- psychiatric diagnosis | suicidal ideas or acts | interpersonal support systems | analysis of the suicide crisis | psychiatric / medical / family history | ● Observe the client - is the client agitated or restless? ● Is the client withdrawn and apathetic ● Did the clients affect change to a brightened affect? ● Clues or cries for help - verbal and nonverbal clues ● “I just can't take it anymore.” ● “There is no reason to go on.” ● Gives away prized possessions ● feels hopeless ● cancels social events ● Obtain thorough history + Mental status exam! Assess For Suicide Potential ● ● ● Lethality - does the clients plan have a high potential to cause death? Intent - has planned exactly when Access - to method of suicide Pharmacology Lithium ● ● ● ● ● ● ● ● ● ● ● Mood Stabilizer Anti-manic Therapeutic Level: 0.6-1.2 mEq/L Manic Therapeutic Level: 1.0-1.5 mEq/L Toxic Level: >1.5 mEq/L Mild Toxicity ● 1.5-2.0 mEq/L ● blurred vision, ataxia, tinnitus, persistent N/V, severe diarrhea ● Treatment: IV solution Moderate Toxicity ● 2.0-3.5 mEq/L ● excessive output of dilute urine, increasing tremors, muscular irritability, psychomotor retardation, mental confusion, giddiness ● Treatment: hydrate, give Kayexalate NOT charcoal. Severe Toxicity ● >3.5 mEq/L ● impaired consciousness, nystagmus, seizures, coma, oliguria/anuria, arrhythmias, myocardial infarction, cardiovascular collapse ● Treatment: hemodialysis may be indicated in severe cases. Precautions ● Toxicity risk! ● drink 6-8 glasses of water a day ● maintain consistent salt consumption / meals / caffeine Adverse Side Effects ● EPS ● Tardive Dyskinesia ● Neuroleptic Malignant Syndrome *If Pt cannot tolerate Lithium , switch to Depakote or other Anti-convulsant class.* Notes From Class ● Everyone please add what notes you have from lecture for the test review below. ● After you cover a topic in the above outline please delete it off the list of notes below so everyone knows what is missing and still needs to be added in, that way we can all know what still needs to be done / covered. Thanks! ● 3 groups of ppl need to eat appropriate - depressed / manic / schz 1. MAJOR DEPRESSION 2. BIPOLAR MANIA 3. SCHIZOPHRENIA ● If starting someone on maoi - adhere to diet / drug to drug restrictions - make sure they are a good candidate - ex: not an Alzheimer's pt ● Food to avoid with MAOIs 1. BAR FOODS, HAPPY HOUR FOODS, YEAST, BEER, EDAMAME, TYRAMINE 2. MAINTAIN SODIUM, CAFFEINE LVLS 3. CAN LEAD TO HYPERTENSIVE CRISIS-GIVE ANTIHYPERTENSIVE MEDS SLOWLY ● Symptoms of neuroleptic malignant syndrome ● “FARM” FEVER (SUDDEN AND HIGH) AUTONOMIC CHANGES RIGIDITY OF MUSCLES MENTAL STATUS CHANGES ● Nursing interventions for auditory hallucinations -REALITY ORIENTATION ● Review the SEs of LAMICTAL- anticonvulsant RASH (BIGGEST SIGN) ● Diff between onset / 3 gross - Benzes / antihistamines / anxiety meds ???? ● Review anticonvulsants TEGRETOL (4-12)<---therapeutic range DEPAKOTE (50-150)<---therapeutic range LAMICTAL (40 questions / lots of select all) EXAM 2 – OUTLINE (From Blackboard) S & S of Schizophrenia (- & +) ● ● Positive Symptoms (Excess or distortion of normal function) ● refers to symptoms that most individuals do not normally experience but are present in schizophrenia ● experiencing things others do not ● ex: hallucinations | delusions | thought disorders | movement disorders | word salad | flight of ideas | clang associations | Negative Symptoms (A deficit of function) ● lose the ability to do or feel things that are present in schizophrenic persons but are NOT normally found in healthy persons ● symptoms that reflect the loss or absence of normal traits or abilities. ● contribute more to poor quality of life, functional disability & the burden of others. ● these symptoms tend to stay ● ex: no emotion | just doesn’t care | loss of interest in everyday activities | lack emotion | neglect of personal hygiene | social withdrawal | Schizoaffective ● ● ● ● ● ● Thought disorder mixed with a mood disorder Presents with severe mood swings either of mania or depression with psychotic symptoms For at least 2 weeks the client must have experienced psychotic symptoms only Usually occurs later in life Prognosis is better than schizophrenia but worse than mood disorders Catatonic features may also be present Antipsychotics (Typical & Atypical) Typical Atypical ● ● ● ● 1st Generation For (+) S&S Blocks dopamine Sedation ● ● ● ● 2nd / 3rd Generation For (+) and (-) S&S Blocks dopamine & Serotonin Sedation ● ● ● Chlorpromazine (Thorazine) Haloperidol (Haldol) Fluphenazine (Prolixin) ● ● ● ● ● Clozapine (clozaril) - 1st Atypical Risperidone (Risperdal) Olanzapine (Zyprexa) Paliperidone (invega) Abilify (3rd Generation) ● ● ● ● ● Disadvantages EPS NMS Anticholinergic side effects Tardive Dyskinesia Weight gain, sexual dysfunction, endocrine disturbances ● ● ● Disadvantages Tendency to cause significant weight gain Agranulocytosis Orthostatic hypotension EPS & treatment ● ● ● ● ● ● ● Extrapyramidal Symptoms Main side effects of 1st Gen Typical Antipsychotics Makes it difficult for Pt to stay compliant with meds Pseudo Parkinson's “Thorazine Shuffle” Acute Dystonias (painful muscle contractions) / Oculo Crisis Akathisia - can't sit still / agitation Treatment: CABI RIDE ○ C- Cogentin (for pseudo parkinson's & acute dystonia) ○ A - Artane (for alternative to cogentin) ○ B - Benadryl (for acute dystonias) ○ I - Inderal (for akathisia) TD ● Tardive Dyskinesia ○ Long term, chronic condition which appears over time if EPS goes untreated! ○ Most common with typical antipsychotics (neuroleptics) ○ Involuntary muscle movements ○ Condition affecting the nervous system, often side effect of long term use of psychiatric drugs. ○ AIMS - Abnormal Involuntary Muscle Movement Scale ○ Part of EPS NMS ● Neuroleptic Malignant Syndrome ○ ○ ○ ○ ○ ○ Life threatening reaction to antipsychotic medications! Most commonly occurs in 1st to 2nd week of treatment Idiosyncratic reaction to neuroleptic medications Symptoms: Characterized by fever (over or around 104), muscular rigidity, altered mental status, and autonomic dysfunction Often occurs shortly after initiation of Neuroleptic treatment or after dose increase. Treatment: Stop Medications! Give dantrolene (Dantrium) & bromocriptime (Parlodel) . ECT –Procedure & nursing responsibilities ● Electroconvulsive Therapy ● ● ● ● ● ● ● ● ● ● ● ● ● ● induction of a grand mal seizure through application of electrical current to the brain. Indications: Major Depression, Bipolar-mania, Schizophrenia duration of seizure should be 15-25 seconds 6-12 treatments place Pt side lying after ECT! Assess for suicide even after ECT! Only absolute contraindication for ECT is increased intracranial pressure from brain tumor, recent CVA, or other cerebrovascular lesion. Most common side effect is temporary memory loss and confusion Nurse must ensure informed consent has been granted by the MD! Nurse must assess mood, level of anxiety, thought and communication patterns, and vital signs. Nurse helps to orient Pt to time and place after procedure and what has occurred Nurse monitors vitals every 15 minutes for the first hour MOA: ECT increases the circulating level of neurotransmitters Dopamine, Serotonin, Norepinephrine, Glutamate, GABA Nursing Responsibilities: Safety & Manage Anxiety! TMS treatment ● Transcranial Magnetic Stimulation ○ ○ ○ ○ ○ Noninvasive therapy that uses magnetic pulsations to stimulate the cerebral cortex of the brain only indicated in Major Depressive Disorder Frequency of treatment - everyday for 4 - 6 weeks. Relatively safe / no anesthesia Least Invasive!! S & S of Depression ● ● ● ● Signs & Symptoms: ○ Loss of Energy ○ Self-loathing ○ Reckless behavior ○ Concentration Problems ○ Somatic - Unexplained aches and pains ○ Feelings of helplessness and hopelessness ○ Loss of interest in daily activities ○ Appetite or weight changes ○ Sleep changes ○ Anger or irritability Relationship between Depression & Medical illness - depression may present with physical symptoms / problems, rule out the physical problems first. DO not just assume someone is depressed. Self Destructive Direct Behavior - wrist cutting, self mutilation Self Destructive Indirect Behavior - drinking, drugs etc. Premenstrual Dysphoric D/O ● ● Symptoms: depressed mood | anxiety | mood swings | decreased interest in activities | symptoms begin during week prior to menses, start to improve within a few days after the onset of menses, and become minimal or absent in the week post-menses. SSRIs- side effects ● Selective Serotonin Reuptake Inhibitors ○ Antidepressant ○ First-line therapy ○ Drowsiness | nausea | dry mouth | insomnia | diarrhea | nervousness, agitation or restlessness | dizziness | sexual problems | headache | blurred vision ○ Serotonin Syndrome Serotonin Syndrome ● ● ● Side effect of SSRIs High levels of Serotonin accumulated in body S&S - confusion | agitation / restless | tachycardia | hypertension | dilated pupils | muscle rigidity | sweating | fever | seizures | headache | shivering | goosebumps MAOIs/ Hypertensive Crisis ● Monoamine Oxidase Inhibitors ○ Neurotransmitter effects ○ Regulate intake of Tyramine !! - MAOIs block enzyme that breaks down excessive levels ○ Leads to hypertension Bipolar 1 & 2 Bipolar I ● Experience manic episodes or more manic episodes ● may have depressive episodes ● 1st episode of Mania, hypomania, mixed (recurrent mood episodes) ● psychosis or catatonia may be present ● In order to be Bipolar 1, you have to have 1 manic episode in your life for at least 2 weeks! Bipolar II ● Recurrent MDD with hypomania ● never experienced a full manic episode ● psychosis or catatonia may be present ● In order to be Bipolar 2 , you only have to have 1 episode of hypomania in your life for 2 weeks! Mood Stabilizers (Li- Lamictal) ● Lamotrigine (Lamictal) ○ Anticonvulsant (antiepileptic) drug ○ Contraindicated with MAOIs ○ Do not D/C abruptly ○ Indicated for treatment of mania & depressive episodes Cognitive Behavioral Therapy ● ● Cognitive behavioral therapy (CBT) is a short-term, goal-oriented psychotherapy treatment that takes a hands-on, practical approach to problem-solving. Its goal is to change patterns of thinking or behavior that are behind people's difficulties, and so change the way they feel. CBT works by changing people’s attitudes and their behavior by focusing on the thoughts, images, beliefs and attitudes that are held (a person’s cognitive processes) and how these processes relate to the way a person behaves, as a way of dealing with emotional problems.



![[100% HDQ]**[VIDEO] Sully Full HD online streaming Watch](http://s2.studylib.net/store/data/018201909_1-d9e42526408b40da0a9798833ad4d3be-300x300.png)
