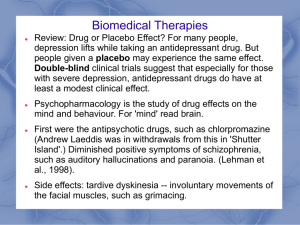
Mood Disorders: Bipolar I and II Learning Objectives 1.Discuss types of mood disorders: Depression, Bipolar Disorder 2.Describe signs and symptoms of mood disorders 3.Discuss treatment approaches for mood disorders 4.Explain mechanism of action, common side effects and nursing considerations related to medications used to treat mood disorders. 5.Use the nursing process to assess and formulate nursing diagnoses and care interventions and teaching for a client with a mood disorder. 6.Articulate the care of the client undergoing electroconvulsive therapy (ECT). What is Bipolar Disorder? • The 2 “poles” are mania and depression • Affects men and women equally • No single gene identified, but a strong genetic component • Can start in childhood or throughout adulthood Mania BP I • VERY elevated mood for at least 1 week, not attributed to other causes meds, substances etc. • Episodic • • • • • • • • Inflated self-esteem, grandiosity Decreased need for sleep Very talkative Flight of ideas, racing thoughts Easily distracted Increased goal-directed activity, agitation Risky behavior, poor judgment May include psychosis • Mood disturbance causing social, work, or interpersonal problems • May need hospitalization Hypomania “Manic Lite” BP II Same symptoms but less severe than mania • At least 4 days’ duration • Not severe enough to warrant hospitalization • Persistent elevated expansive or irritable mood • NEVER psychosis • Symptoms don’t cause major effects on functioning Depressive Episode BP I and II • Unable to focus or concentrate • Thoughts of death and suicide • Excessive sleepiness Mixed Episode • Person may have features of both mania and depression at the same time to varying degrees • Marked impairment in functioning Cyclothymic Bipolar • Rapid Cycling • Swing between a hypomanic episode and depressive symptoms • Symptoms have occurred for at least 2 years • Symptoms have occurred without remission for more than 2 months Bipolar I • Bipolar I – Most Serious • Symptoms: one episode of MANIA !!!! alternating with one episode depression. • May include Psychosis Bipolar II • Bipolar II – More Common • Symptom: one or more hypomanic episodes alternating with depressive episodes • No full mania or psychosis What Bipolar is not… • Moodiness • A Personality Disorder • An Adjective Assessment, Diagnosis and Treatment • Diagnosis based on symptoms meeting DSM-5 criteria • Ask about caffeine, energy drinks, alcohol, steroids, medications including OTC and Illicit drugs • Ask about medical conditions • Assess appearance, thoughts, speech, affect, judgment, behavior • Is it Bipolar ? Misdiagnosis is common • Biological • Medications • • • • Stabilize mood Dampen mania Alleviate depression Treat psychosis (delusions, hallucinations) • Psychological • • • • Supportive therapy May “dig deep” Helps people to deal with the devastation that their manic behavior has wrought ECT Pharmacology: Mood Stabilizing Drugs First line Treatments • LITHIUM treatment of choice for controlling mania in bipolar disorder • Anticonvulsants (Lamotrogine, Valproate and Depakote) • Antipsychotics (mostly SGA) second generation antipsychotics • Benzodiazepines • Antidepressants can be used but with caution! Pharmacology Examples • Acute Mania • • • • Drugs: Lithium carbonate (Eskalith, Lithobid) Must be compliant, requires labs and lifestyle changes Risk of OD and Toxicity Common Side Effects: fine hand tremors, GI upset, polyuria (Diabetes Insipidus), wt gain, Hypothyroidism, Wt gain, kidney toxicity, electrolyte imbalance , leukocytosis • Think LITH ( Leukocytois, insipidus, Tremors, Hypothyroidism) Labs – Lithium (CRITICAL) • • • • • • Plasma - Lithium Toxicity level BUN and Creatinine Hypothyroidism - TSH levels rise when T3 & T4 is low Hypothyroidism - TSH levels rise when T3 & T4 is low TSH (T3 and T4), TSH range 2-10 mu/l Check Na+ need sodium to keep lith levels • AVOID DIURETICS ! Get rids of Na+ and Water, no NSAID too hard on kidneys • 100 % eliminated by kidney • Avoid in Renal disease. Nursing Responsibilities: Lithium • Lithium levels monitored due to the narrow window between therapeutic and toxic!! 1.5 mEq/L Therapeutic range 0.6 – 1.2 mEq/L (varies by textbook, keep range around 1.0 mEq/L) Inpatient check labs prior to administration Labs within 5 days of starting drug, weekly, then monthly, 3, 6 – 12 mos Labs if dosage increases/ Labs if behavior changes Labs in a.m. 8-12 hours after last dose Older adults, very thin clients - start low, go slow Fluids important, Food Important (mania/depression), Assess labs Lithium Toxicity !!! • Ensure adequate salt intake • Decreased sodium in the body can increase risk of lithium toxicity Symptoms: Moves from mild to COARSE Hand tremors, blurred vision, ataxia, SEVERE NV diarrhea, psychomotor retardation, mental confusion, coma, cardiovascular collapse. Treatment: Stop drug, call provider, gastric lavage, hemodialysis Anticonvulsants to Treat Bipolar • Lamotrogine (Lamictal) • Carbamazepine (Tegretol) Black Box Warning ! • Can cause blood dyscrasia (anemia, leukopenia, thrombocytopenia), vision problems, SIADH – syndrome of inapproraiet ADH - causes retention of water and dilutes blood, skin rash. • CBC, infection (WBC may be low) Anticonvulsant • Valproic Acid (Valproate) • Black Box Warning • Hepatotoxcity, pancreatitis, GI upset, Thrombocytopenia, Neural tube defects in developing fetus • Labs: • LFT, ALT, AST, bilirubin – hepatotoxicity Anticonvulsant - Lamotrogine (Lamictal) Black Box Warning Steven Johnson Syndrome Side Effects • Blurred vision • Decreased appetite • Irregular HR/ RR • Decreased urine output • NV • Poor motor coordination • *seizures • STOP MED ! Nursing Assessment • Obtain medical and mental health history • Assess symptoms: subjective and objective data • Assess physical health (re: assess underlying health problems ie: HTN, new or healed scars and bruises, hair pulling, agitation, appearance, weight. • Evaluate lab data: urine drug screen, pregnancy test, BUN and creatinine, liver function, electrolytes / chem profile, CBC and BG. • Assess: ADL’s, sleep, nutrition, musculoskeletal, neurological, GI, GU, reproductive. • Assess: mood, affect and behaviors. • Assess: culture/diet/health care practices/rituals/alternative medicines/language • Assess suicide risk- intent, plan, access to lethal methods, and acts of deceptiveness related to suicide. Nursing Interventions: Bipolar Disorders • Matter-of-fact tone • Clear, concise directions and comments • Limit setting • Remain calm • Avoid arguing and debating • SUICIDE RISK HIGH • Safety • Staff consistency • Reduce environmental stimuli • Do not escalate patients • Reinforce appropriate hygiene, dress • Monitor nutrition and sleep • Establish routines Risk Assessment • Patients with Mood disorders are at high risk for: • Suicidal thoughts and suicide • Substance abuse • Ineffective coping • Physical illness Assessment, monitoring and evaluation of each patient is critical! Nursing Diagnosis • Alteration in thought processes • Ineffective Individual Coping • Alterations in Family Relationships • Risk for Self Harm • Risk for Violence • Imbalanced Nutrition • Sleep deficit • Spiritual Distress Nutrition and Sleep • Provide food to eat on the run • Provide high-protein, highcalorie snacks • Provide daily multivitamins • Weigh regularly • Provide quiet environment for sleep • Structure to avoid stimulating activities during evening • Reduce caffeine intake, especially in evening • Assess sleep-rest patterns Patient Teaching • Illness • Signs of relapse • Medication (need to understand meds and side effects, compliance with meds critical!) • Coping with symptoms • Providing support • Cognitive Behavioral Therapy/ Psychotherapy/ Individual/Group Other medications for Acute Mania • Seroquel (atypical antipsychotic) • Depakote (anticonvulsant) • Tegretol (anticonvulsant) • Risperidal (atypical antipsychotic) • Latuda (atypical antipsychotic) • Saphris (atypical antipsychotic) • Abilify (atypical antipsychotic) • Invega (atypical antipsychotic) INJ • Vraylar (atypical antipsychotic) Acute Bipolar Depression • Seroquel (atypical antipsychotic) • Latuda and Lithium (atypical antipsychotic / mood stabilizer combo) • Latuda and Depakote (atypical antipsychotic / anticonvulsant combo) • Lithium (can treat both mania and depression, BEST for mania) • Lamotrigine (can treat both mania and depression, BEST for hypomania and depression) • Maintenance meds: Lithium, Saphris, Depakote, Seroquel, Abilify, Lamotrigine Questions? Professor Lang email cslang@gwu.edu