Popham_potassium_12.4.09
advertisement

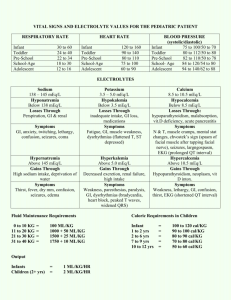
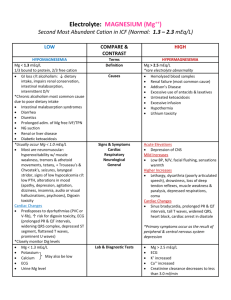
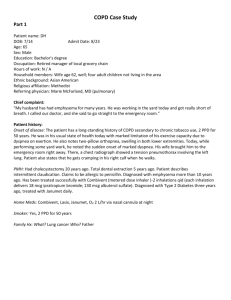
1 Popham – Potassium Renal – 12.04.09 K+ balance -Normal body stores (70 kg adult) are 3000 to 4000 meq K+ (50-55 meq/kg) -98% of K+ is INTRACELLULAR -Intracellular K+ concentration 140 meq/l -Extracellular K+ concentration 4-5 meq/l -Daily intake averages 40-120 meq -Kidney can reduce K+ excretion to less than 15-25 meq/day K+ levels -Normal K+ 4-5 meq/l -K+ decrease by 1 meq/l reflects 200-400 meq total body deficit -K+ increase by 1 meq/l reflects 100-200 meq total body excess K+ functions: -Cell function: has a role in protein & glycogen synthesis -Maintains resting membrane potential in muscle cells and neurons via 3:2 Na+K+ATPase -Determines membrane excitability -Allows actions potentials to be generated Symptoms of high/low K+: -Relates to inability to generate action potentials in muscles -Cramps -Muscle weakness/paralysis: starts in legs -EKG changes & Cardiac Arrhythmias -Variable effects at different levels of hyper/hypokalemia: watch EKG for toxicity –PAC’s, PVC’s, bradycardia, atrial or junctional tachycardia, AV block, v-tach/v-fib EKG Hypokalemia hyperkalemia PR interval prolongation ST Depression --T waves Flat or inverted (hypoK pulls T wave down) Elevated (hyperK pushes T wave up) QRS widened U waves After T waves, ONLY in HypoK! ---- hyperkalemia Hypokalemia Modifiers of K+ effect on Action Potentials Better tolerated Chronic HypoK & hyperK Hypercalcemia inc threshold potential & protects against hyperK which has dec resting potential Worse tolerated Acute hypoK & hyperK Metabolic acidosis exacerbates hyperkalemia, by causing K+ to be released from cells as HCl is buffered into cells Metabolic alkalosis exacerbates hypoK – shift into cells as the bicarb goes out. Regulation of K+ balance: -Distribution of K+ between cells and extracellular fluid –Concentration dependent –Acid-base status dependent –Insulin/catecholamines move K into cells •Type I diabetes w/o insulin high K -Renal excretion of K+ from dietary sources and cellular breakdown –Catecholamines & insulin increase activity of Na+K+ ATPase, uptake of K+ into skeletal muscle & liver –K+ concentration causes passive movement of K+ in or out of cell Popham – Potassium Renal – 12.04.09 2 K+ & Acid/base balance: -Acidemia: K+ moves out of cells as H+ is buffered into cells -Alkalosis: K+ moves into cells as H+ is buffered into the extracellular fluid K+ Elimination: -Major route of elimination is by the kidneys -Some K+ lost in stool or sweat (if clinically important, it’s pathologic) Determinates of K+ Secretion by Kidneys: -Plasma K+ concentration -Aldosterone: causes K+ secretion by principal cells of collecting tubule –Outer medulla, cortical & inner medulla -Urine flow in distal tubule (permissive effect to allow you to excrete K) -Vol depleted can have high K due to low urine flow by principle cells. K+ handling in Renal Tubules: -K is filtered at glomerulus -Reabsorbed proximal tubule, following water and sodium -Reabsorbed loop of Henle (thick ascending limb), via NaK2Cl carrier in luminal membrane -Secreted distally: distal tubule, collecting tubule by principal cells -In severe hypoK, K can be reabs in collecting duct by intercalated cells -wont have aldostrone to tell you to get rid of K+ Distal tubule Secretion of K+ -Principal cells –Luminal membrane: Na+ & K+ channels –Basolateral membrane: Na-K ATPase -Aldosterone –Released in response to 0.1 meq/l increase in K+ –Increases # of open Na+ & K+ channels –Increases activity of Na-K ATPase (Na out, K in to urine) -K concentration in blood (tubule cell): gradient -Distal flow is permissive – if nothing is going by you cant clear K Hypokalemia: -Causes: Dec intake (rare), Inc entry into cells, inc GI losses, inc urninary loses, inc sweat losses, dialysis. -dietary causes -Rare to get hypokalemia from inadequate diet alone (poverty, clay, diuretics & HTN) -Rare to get hyperkalemia from dietary sources if adrenals and kidneys are working properly -Hypokalemia: increased entry into cells -Metabolic alkalosis -Hyperinsulinemia -Increased catecholamines/beta agonists -Hypokalemia due to Increased GI Losses -Normally 3-6 liters/day GI secretions, but almost all reabsorbed usually only 100-200 ml water lost in stool -Nausea/vomiting : exacerbated by metabolic alkalosis (lose acid secretions form stomach) & urinary K+ losses -Nasogastric (NG) tube suction -Diarrhea/intestinal fistulas/tube drainage -Hypokalemia due to Increased Urinary Losses -Inc distal flow d/t impaired salt & water reabs: Diuretics, Salt wasting nephropathies, Polydipsia/polyuria (from permissive K loss in CT) -Hypercalcemia (increased distal flow) -Mineralcorticoid excess: aldosterone -Hypomagnesemia: inhibits ATPase Popham – Potassium Renal – 12.04.09 3 -Other causes of hypokalemia -Increased sweat losses: 5-10 meq/l (Chronic heavy exertion in hot climates) -Dialysis –Potassium bath set too low –Correction of acidosis with HD can cause hypokalemia even if no net K+ removal, in the setting of total body K+ depletion –Peritoneal dialysis patients can lose 30 meq/day K+ in peritoneal fluid -Evaluation of Hypokalemia (when not obvious by H&P) -Determine if loss is GI or renal -GI losses should be obvious, except in cases of anorexia/bulemia/laxative abuse -24 hour urine K+ when hypokalemic –Kidney can decrease urine excretion of K+ to 25-30 meq in 24 hours –If urine K is low, then loss is not from kidney -Acid/base status: acidosis or alkalosis -Hypokalemia organized by acid-base status and GI vs renal K losses -Low urinary K (therefore GI losses) –Acidosis: lower GI losses (laxatives/villous adenoma) –Alkalosis: upper GI losses (Vomiting) -High urinary K (therefore kidney losses) –Acidosis: Ketoacidosis, type I or II RTA –Alkalosis: •Normotensive: vomiting, diuretics (early), Bartter’s (lose K) •Hypertension –High renin: diuretics,renovascular disease, reninoma, Cushings –Low renin: measure aldosterone »Low aldosterone: exogenous mineralcorticoid »High aldo: adrenal adenoma or hyperplasia -Complications of Hypokalemia -Muscle weakness, cramps, cardiac arrhythmias -Rhadomyolysis (K+ < 2.5 meq/l) -Renal dysfunction: loss of urinary concentrating ability -Increase in urinary NH3 and NH4+ production/excretion -Hypokalemic nephropathy/Interstitial fibrosis -Hypertension: low K+ diet causes uptake of Na+ –Initial Tx is high K diet (fruits & veggies) -Treatment of Hypokalemia -Replace to get pt out of danger initially, then more gradually replace entire K deficit -K+ deficit can only be approximated: –Roughtly 200-400 meq for each 1 meq/l drop in K+ –Below 2, K+ deficit can be much greater due to shifts out of cells to compensate -Treat underlying cause of low potassium -Potassium replaced orally or intravenously -Hyperkalemia: -Causes -Increased Intake: oral or IV - hyperK from diet rare if kidneys and adrenal glands work properly -Shift: Movement from cells into extracellular fluid -K+ intake initially buffered by uptake into skeletal muscle and liver cells, mediated by insulin and beta-adrenergic receptors -K+ elevation of 0.1 meq/l triggers release of aldosterone, and urinary excretion of excess K+ within 6-8 hours Popham – Potassium Renal – 12.04.09 4 -Decreased urinary excretion -K+ adaptation -Normal kidney function –the kidneys can adapt to excrete as much as 5x the normal K+ intake (400 meq/day) –more rapid excretion of K+ -Chronic Kidney Disease (CKD): reduced nephron mass –increased K+ excretion per remaining nephron as long as distal urine flow is maintained and aldosterone secretion occurs -K Shifts: Serum K+ can be elevated even if total body K+ is normal -Insulin deficiency with hyperglycemia -Metabolic acidosis -Muscle/tissue breakdown -Hyperkalemia: decreased urinary excretion -Renal failure: most common cause -Effective circulating volume depletion (Decreased distal flow) -Hypoaldosteronism -Hypoaldosteronism -Secondary decrease in aldosterone due to decreased activity of renin-angiotensin system •Hyporeninemic hypoaldosteronism (diabetics with Chrinoic kidney disease) •Drugs: ACEi, NSAID’s, cyclosporine •HIV disease/clinical AIDS -Primary decrease in adrenal synthesis of aldosterone -Aldosterone resistance –Drugs: K+ sparing diuretics, Trimethoprim (HIV) -Diagnosis of Hypoaldosteronism: Transtubular K+ Gradient (TTKG) TTKG= Urine K+ / (Uosm/Posm) Plasma K+ -use equation ONLY in hyperK -Accurate as long as urine is not dilute and urine Na+ > 25meq/l -Aldosterone present: TTKG 8-9 on normal diet, >11 after K+ load -TTKG <7, and especially <5 suggests hypoaldosteronism -Treatment of Hyperkalemia -EKG changes: begin treatment immediately -Concomitant acidemia or hyponatremia will potentiate K+ toxicity -Antagonize K+ effects (seconds/minutes) w/ Calcium IV -- antagonize -Shift K+ into cells (minutes): Glucose & insulin, NaHCO3, β-agonists: albuterol nebs, 3% NaCl if hyponatremia present -Remove excess K+ (hours): Loop diuretics if patient makes urine, Cation-exchange resins (kayexalate): avoid rectal use, Hemodialysis/peritoneal dialysis -Hypokalemia/Hyperkalemia -Look primarily to adrenal glands (mineralcorticoids) and kidneys for causes: not usually dietary cause -K shifts from ECF to CF: Insulin, Catecholamines, Conc grad, Acid-base status -Major determinants K excretion by kidney: –K concentration –Aldosterone –Distal urine flow (permissive) -Treatment -Cardiac arrhythmias are major toxicity of both hypokalemia and hyperkalemia -Hypokalemia –Concomitant digoxin use increases risk –Treat to get out of danger, replace losses, and prevent further losses Popham – Potassium Renal – 12.04.09 –Check for hypomagnesemia -Hyperkalemia –Antagonize membrane effects: Calcium IV –Shift K+: insulin/glucose/NaHCO3 –Remove K+: diuretics, Kayexylate, dialysis Practice Questions: 1. Which of the following regarding postassium are true? a. 98% of K+ is intracellular b. normal K+ levels are 4-5 meq/L c. maintains resting potential in skeletal & muscle cells d. role in protein & glycogen synthase e. all of the above 2. Symptoms common to hyperkalcemia & hypokalcemia include: a. Increased ability to generate action potentials in muscles b. Cramps c. Muscle hyperexcitability, starting in arms d. EEG changes 3. Which of the following EKG findings would help you distinguish between hyperkalcemia & hypokalcemia? (2) a. PR interval prolongation b. Elevated T waves c. Widened QRS interval d. U waves 4. Identify in your answers to #3 which is associated with hyperkalcemia & hypokalcemia 5. Which of the follow exacerbate hyperkalcemia? a. metabolic acidosis b. metabolic alkalosis c. hypercalcemia d. digoxin use 6. Fill in the blanks with acidosis or alkalosis: -A: ________________: K+ moves into cells as H+ is buffered into the extracellular fluid -B: ________________: K+ moves out of cells as H+ is buffered into cells 7. A the transtubular gradient value of ___________ is indicative hypoaldosteronism. a. < 7 meq/L b. 8-9 meq/L c. 10-11 meq/L d. >12 meq/L Answers: 1. E 2. B 3. B & D 4. B = hyperkalcemia; D: hypokalcemia 5. A 6. A = Alkalosis; B = Acidosis 7. A. 5