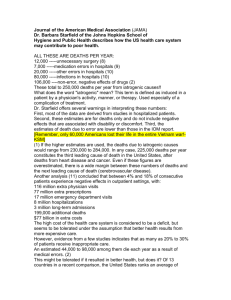
Variations in the Health Status of Population Groups in
advertisement

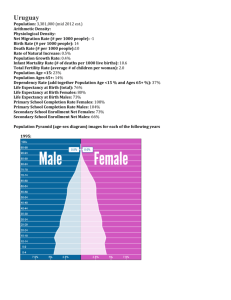
Variations in the Health Status of Population Groups in Australia. Australians generally enjoy good health and are among the healthiest people in the world; however, health is not shared equally by all Australians, and different groups experience different levels of health. When focusing on variations in health status, we will consider four population groups in Australia: > Males and females >Higher and lower socioeconomic status groups >Rural and remote populations, and >Indigenous populations. MALES AND FEMALES There are significant differences in the health status of males and females in Australia, and whether a person is male or female has a complex effect on their health. To begin with, however, it is important to make a distinction between two terms that are frequently used when discussing male and female health – sex and gender: > A person’s sex refers to them being genetically or biologically male or female. > Gender refers to socially constructed roles, behaviours, activities and attributes that a given society considers appropriate for males and females. LIFE EXPECTANCY In terms of life expectancy, Australian females born in 2005 could expect to live an average of 83.3 years and a male could expect to live to 78.5 years. In the past 100 years in Australia, life expectancy has been consistently higher for women than for men, although the size of the difference has varied. In recent years, the gap has narrowed. This has largely been attributed to significant reductions in the death rates of males aged 45 years and over, and particularly to the reduction in the heart disease deaths among males. MORTALITY Gender has a powerful impact on mortality: there are distinct differences in the causes of mortality between males and females. In 2005, male deaths outnumbered female deaths, with a death rate ratio of 107 males to 100 females. >For males, coronary heart disease was followed by lung cancer, cerebrovascular disease, other heart diseases, prostate cancer, chronic obstructive pulmonary disease (COPD), colorectal cancer, unknown primary site cancers, diabetes and suicide/ Injuries. > For females, coronary heart disease was followed by cerebrovascular disease, other heart diseases, dementia and related disorders, breast cancer, lung cancer, COPD, colorectal cancer, diabetes and pneumonia and influenza. > One of the factors that accounted for the increasing differences between male and female death rates is the dramatic decrease in maternal mortality since the early part of last century. > Cancer deaths increased for women, However men with cancer are more likely to die. >In each age group, males are more likely to die of deaths from accidents, poisoning and violence than women. > The suicide rate is higher for males than females. MORBIDITY Despite women having longer life expectancy than men, they have higher rates of illness and disability. They are also more likely to report illness than men, both for recent and long-term conditions. The greater morbidity for women compared to men may be partly explained by biological reasons associated with childbirth, menstruation and menopause. However, even when all aspects of reproductive health are controlled, women still have acute illness rates roughly 20–30 per cent higher than men’s (apart from injury). How can we explain the variations between Males and Females? Socially determined behaviour and the fact that more men typically work in high-risk industries could account for higher male mortality rates. In particular risk-taking behaviour and aggressive behaviour have traditionally been considered more acceptable for men than women in Australian society. During childhood, boys are more prone to accidents due to either preferences for particular types of activities, or differences in maturation of their physical abilities. This may extend to sport and other activities as males get older. Some men, particularly younger ones, think they are indestructible, and this can lead to destructive behaviours, such as alcohol or drug binges, reckless driving or other risky behaviours. Men are more likely than women to avoid medical treatment and less likely to undergo screening for illnesses, such as cancer. Women are more likely to have regular contact with doctors due to menstruation, contraception and pregnancy issues. Men do not have similar issues that require them to regularly see a doctor and are less likely to recognise and act on signs of risk. Men have lower rates of illness because they are less likely to perceive symptoms, communicate about or express them and seek professional help. This may be because of societal expectations for male behaviour. Men are encouraged to be ‘tough’ and in control of their emotions. Complaining of feeling ill or visiting a health professional may be seen as ‘weak’, a threat to their masculinity or simply a waste of time. Factors such as education status, employment and income are important determinants of health. Males from low socioeconomic backgrounds comprise one of the unhealthiest subgroups in Australia. They are more likely to get sick than those from higher socioeconomic backgrounds and are more likely to die from a range of health issues. There is a direct link between employment status and men’s health. For example, rises in unemployment lead to proportional rises in male death rates Male depression is associated with an increased risk of health disorders, such as cardiovascular disease and diabetes. Men are more likely to resort to destructive behaviours to deal with their depression – the suicide rate for males between the ages of 15 and 24 has tripled in the past three decades. Other behavioural factors that impact on health status include physical activity (exercise) and food intake. Figure 2.1.6 Burden (DALYs) by broad cause group, Australia, 2003 Source: Begg, S., Vos, T., Barker, B., Stevenson, C., Stanley, L. and Lopez, A. 2007, The Burden of Disease and Injury in Australia 2003, AIHW,