Supplementary Information 1 (docx 16K)

SUPPLEMENTARY METHODS AND PATIENTS
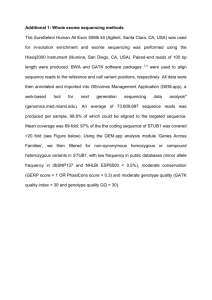
Whole Exome Sequencing:
Whole exome sequencing was performed on exon targets isolated by capture using the Agilent
SureSelect Human All Exon V4 (50 Mb) kit (Agilent Technologies, Santa Clara, CA). One microgram of DNA from blood specimens was sheared into 350-400bp fragments, which were then repaired, ligated to adaptors, and purified for subsequent PCR amplification. Amplified products were then captured by biotinylated RNA library baits in solution following the manufacturer’s instructions. Bound DNA was isolated with streptavidin-coated beads and reamplified. The final isolated products were sequenced using the Illumina HiSeq 2000 or 2500 sequencing system with 100-bp paired-end reads (Illumina, San Diego, CA). DNA sequence was mapped to the published human genome build UCSC hg19/GRCh37 reference sequence using
BWA with the latest internally validated version at the time of sequencing (v0.5.8 through
BWA-Mem v0.7.8). Targeted coding exons and splice junctions of known protein-coding
RefSeq genes were assessed for average depth of coverage with a minimum depth of 10X required for inclusion in downstream analysis. Local realignment around insertion-deletion sites was performed using the Genome Analysis Toolkit v1.6. Variant calls were generated simultaneously on all sequenced family members using SAMtools v0.1.18. All coding exons and surrounding intron/exon boundaries were analyzed. Automated filtering removed common sequence changes (defined as >10% frequency present in 1000Genomes database). The targeted coding exons and splice junctions of the known protein-coding RefSeq genes were assessed for the average depth of coverage and data quality threshold values. Whole exome sequence data for all sequenced family members was analyzed using GeneDx’s XomeAnalyzer (a variant annotation, filtering, and viewing interface for WES data), which includes nucleotide and amino
acid annotations, population frequencies (NHLBI Exome Variant Server and 1000 Genomes databases), in silico prediction tools, amino acid conservation scores, and variant references.
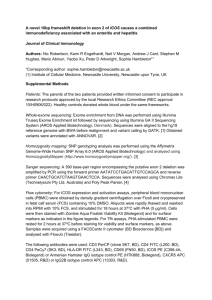
Detailed clinical information
Patient 1. The male proband was 20 years-old at the time of ascertainment and the first child born to his non-consanguineous Hispanic parents. He was delivered after an uneventful pregnancy at term with a birth weight of 2.92kg. During childhood, he received the diagnosis of global developmental delay and spastic quadriplegic cerebral palsy. Other medical problems included epilepsy diagnosed at 3 years of age that continues to require medical management, scoliosis with rods placement, and multiple aspiration pneumonias necessitating gastrostomy tube feedings. The patient was also diagnosed with severe obstructive sleep apnea and hypoventilation, bilateral sensorineural hearing loss, and myopia with astigmatism. Global developmental delay was noted during infancy. No history of regression has been documented.
During his most recent examination, his head circumference and weight were 54cm and 54kg, respectively. An initial brain MRI at age 3 showed diffuse cerebral atrophy. A subsequent brain
MRI with spectroscopy at age 14 revealed severe diffuse brain atrophy and moderate cerebellar atrophy with thinning of the corpus callosum. The most recent brain MRI at age 20 showed not only these changes but also findings suggestive of iron deposition on heavily T2-weighted sequences at the level of the globus pallidus and substantia nigra. Other evaluations included karyotype, fragile X testing, acylcarnitine profile, and urine organic acids, all within normal limits. Initial lactate and pyruvate elevations at age 3 were not persistently documented over time.
Patient 2.
She was born full term after an uncomplicated pregnancy with a birth weight of
3.34kg. Developmental concerns appeared during the first year of life. She walked at 16 months, started saying her first words at 2 years of age, and speaking in short sentences by age 8 years.
She was diagnosed with mild bilateral sensorineural hearing loss at age 9 that has remained stable overtime. Her medical history has otherwise been unremarkable and with no previous seizures. On physical exam at 14 years of age, her weight was 61.4kg (84 th
centile), her height was 151cm (5 th centile), and head circumference was 56 cm (90-97 th centile). The first brain MRI at age 7 years showed only thinning of the corpus callosum. However, the repeat image at age 14 revealed iron deposition on heavily T2-weighted sequences at the level of substantia nigra and globus pallidus.
Other studies included karyotype, oligonucleotide chromosomal microarray (44K Array, Agilent
Technologies, Santa Clara, CA) , transferrin isoelectric focusing, DNA methylation for Angelman syndrome, and MECP2 sequencing and del/dup by MLPA, all with normal results. Like her brother, she was found to have mild elevations of her lactate and pyruvate at 7 years of age that were not subsequently replicated. Her creatine kinase and liver function studies were normal at age 14 years. A n ext generation sequencing X-linked intellectual disability panel that includes 81 genes was performed, and an intronic variant of unknown significance in the OFD1 gene was detected. The c.2929-18C>T change was interpreted as unlikely to be pathogenic and not found in her brother.