pubdoc_10_4622_1660
advertisement

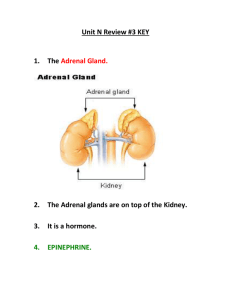
Endocrine Lec: 1 Dr. Mohammed Alhamdany Functional anatomy and physiology: Most hormone release from endocrine glands are under the control of pituitary gland and hypothalamus except for example the adrenal zona glomerulosa (regulated by the renin–angiotensin system), parathyroids (regulated by calcium concentrations) and pancreas(regulated by glucose level). Anterior pituitary hormone secretion is controlled in turn by substances produced in the hypothalamus and released into portal blood, which drains directly down the pituitary stalk. Posterior pituitary hormones are synthesized in the hypothalamus and transported down nerve axons, to be released from the posterior pituitary. Hormone release in the hypothalamus and pituitary is regulated by numerous stimuli and through feedback control by hormones produced by the target glands which are either positive or negative feedback, this is called axes. Paracrine is defined as hormone release from cell to affect adjacent cell such as neurotransmitter, while autocrine define as hormone secrete from cell to affect same cell. The endocrine axes include: 1- Thyroid: thyrotrophin-releasing hormone TRH (in H.) TSH (in anterior P.) T4 and T3 (in T. gland) Metabolism. Feedback: T3 can feedback TRH. 2- Sex hormone: GnRH (gonadotrophin-releasing hormone) in H LH, FSH ( in anterior P) Oestrogen, Progesterone, Androgen in Gonads: testes or ovaries Reproduction. feedback: estrogen, Progesterone ,Androgen, Prolactin, Inhibin can feedback GnRH. 3- Lactation: TRH and Dopamine (suppress) Prolactin (ant. P) Breast Lactation. Feedback: Estrogen and Stress can feedback Dopamine. 4- Growth: GHRH and Somatostatin GH in (ant. P.) IGF1 and IGFBP3 (insulin like growth factor -1 and its binding protein (in the liver) Growth, IGF-1 can feedback GHRH. 5- Adrenal: CRH in H ACTH in ant. P. Cortisol and Androgen in Adrenal cortex Stress. Feedback: Stress and Cortisol can feedback CRH (which secrete in Circadian rhythm). 6- Water balance: ADH in hypothalamus secrete to post. P. (also affect ACTH) Distal nephron Water balance. Feedback: Osmolality and Intravascular volume can feedback ADH. 1 7- Parturition and Lactation: Oxytocin in hypothalamus secrete to post. P. Uterus and Breast Parturition and Lactation Endocrine pathology: Classification of endocrine disease: A-Hormone excess 1- Primary gland over-production 2- Secondary to excess trophic substance B-Hormone deficiency 1- Primary gland failure 2- Secondary to deficient trophic hormone C-Hormone hypersensitivity 1- Failure of inactivation of hormone 2- Target organ over-activity/hypersensitivity D-Hormone resistance 1- Failure of activation of hormone 2- Target organ resistance E-Non-functioning tumors: incidentinoma. Pathology arising within the gland is often called ‘primary’ disease (for example, primary hypothyroidism in Hashimoto’s thyroiditis), while abnormal stimulation of the gland is often called ‘secondary’ disease (for example, secondary hypothyroidism in patients with a pituitary tumour and thyroidstimulating hormone deficiency). Principles of endocrine investigation: Timing: Release of many hormones is rhythmical (pulsatile, circadian or monthly), so random measurement may be invalid and sequential or dynamic tests may be required. Choice of dynamic biochemical tests • Abnormalities are often characterized by loss of normal regulation of hormone secretion. • If hormone deficiency is suspected, choose a stimulation test. • If hormone excess is suspected, choose a suppression test. • The more tests there are to choose from, the less likely it is that any single test is infallible, so avoid interpreting one result in isolation. Imaging • Secretory cells also take up substrates, which can be labelled • Most endocrine glands have a high prevalence of ‘incidentalomas’, so do not scan unless the biochemistry confirms endocrine dysfunction or the primary problem is a tumour 2 Biopsy • Many endocrine tumors are difficult to classify histologically (e.g. adrenal carcinoma and adenoma) THE THYROID GLAND: Diseases of the thyroid predominantly affect females and are common, occurring in about 5% of the population. The thyroid axis is involved in the regulation of cellular differentiation and metabolism in virtually all nucleated cells. The parafollicular C cells secrete calcitonin, which is of no apparent physiological significance in humans. The follicular epithelial cells synthesize thyroid hormones by incorporating iodine into the amino acid tyrosine on the surface of thyroglobulin (Tg), a protein secreted into the colloid of the follicle. Iodide is a key substrate for thyroid hormone synthesis; a dietary intake in excess of 100 μg/day is required to maintain thyroid function in adults. The thyroid secretes predominantly thyroxine (T4) and only a small amount of triiodothyronine (T3); approximately 85% of T3 in blood is produced from T4 by a family of monodeiodinase enzymes. T4 can be regarded as a pro-hormone, since it has a longer half-life in blood than T3 (approximately 1 week compared with approximately 18 hours), and binds and activates thyroid hormone receptors less effectively than T3. T4 can also be converted to the inactive metabolite, reverse T3. T3 and T4 circulate in plasma almost entirely (> 99%) bound to transport proteins, mainly thyroxine-binding globulin (TBG). A circadian rhythm of TSH secretion can be demonstrated with a peak at 0100 hrs and trough at 1100 hrs, but the variation is small so that thyroid function can be assessed reliably from a single blood sample taken at any time of day and does not usually require any dynamic stimulation or suppression tests. Presenting problems in thyroid disease: Thyrotoxicosis: It's defined as clinical features arising from elevated circulating levels of thyroid hormone. The most common causes include: 1- Graves’ disease. 2- Multinodular goiter. 3- Solitary thyroid adenoma. 4- Thyroiditis: including Subacute (de Quervain’s) and Post-partum thyroiditis. 5- Iodide-induced include the Drugs induced eg: amiodarone, and Radiographic contrast media. Clinical feature: common: 1- Weight loss despite normal or increased appetite 2- Heat intolerance, sweating 3- Palpitations, tremor 3 4- Dyspnoea, fatigue 5- Irritability, emotional lability. Less common 1- Osteoporosis (fracture, loss of height) 2- Diarrhoea 3- Muscle weakness and Periodic paralysis 4- Amenorrhoea/oligomenorrhoea. Common sign: 1- Weight loss. 2- Tremor. 3- Palmar erythema. 4- Sinus tachycardia. 5- Lid retraction, lid lag. Less common 1- Goitre with or without bruit. 2- Atrial fibrillation( irregular irregularity). 3- Systolic hypertension/ increased pulse pressure. 4- Hyper-reflexia. Sign specific to graves' disease as a cause of thyrotoxicosis: 1- Goitre with bruit. 2- periorbital oedema. 3- conjunctival irritation. 4- exophthalmos. 4- diplopia. 5- Pretibial myxedema. 6- Thyroid acropachy (periosteal hypertrophy, indistinguishable from finger clubbing). 4