Chapter 14-Payments (RA/EOB) Appeals and Secondary Claims
advertisement
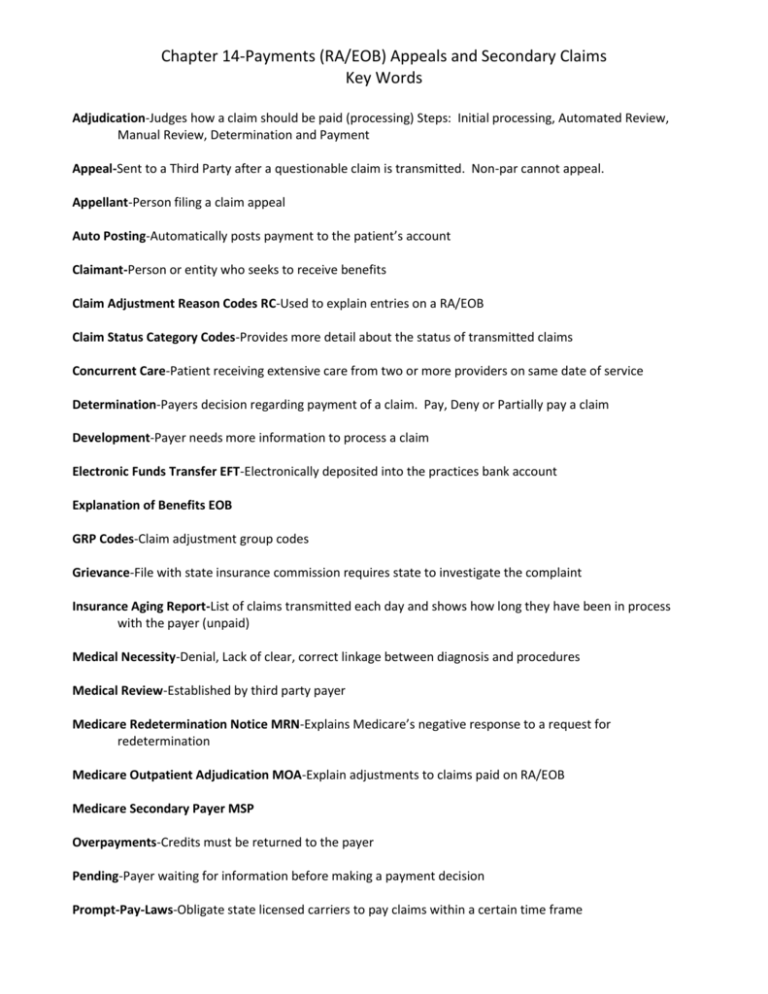
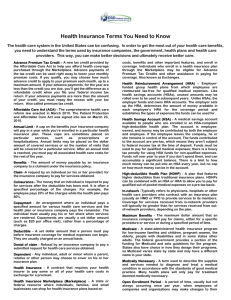
Chapter 14-Payments (RA/EOB) Appeals and Secondary Claims Key Words Adjudication-Judges how a claim should be paid (processing) Steps: Initial processing, Automated Review, Manual Review, Determination and Payment Appeal-Sent to a Third Party after a questionable claim is transmitted. Non-par cannot appeal. Appellant-Person filing a claim appeal Auto Posting-Automatically posts payment to the patient’s account Claimant-Person or entity who seeks to receive benefits Claim Adjustment Reason Codes RC-Used to explain entries on a RA/EOB Claim Status Category Codes-Provides more detail about the status of transmitted claims Concurrent Care-Patient receiving extensive care from two or more providers on same date of service Determination-Payers decision regarding payment of a claim. Pay, Deny or Partially pay a claim Development-Payer needs more information to process a claim Electronic Funds Transfer EFT-Electronically deposited into the practices bank account Explanation of Benefits EOB GRP Codes-Claim adjustment group codes Grievance-File with state insurance commission requires state to investigate the complaint Insurance Aging Report-List of claims transmitted each day and shows how long they have been in process with the payer (unpaid) Medical Necessity-Denial, Lack of clear, correct linkage between diagnosis and procedures Medical Review-Established by third party payer Medicare Redetermination Notice MRN-Explains Medicare’s negative response to a request for redetermination Medicare Outpatient Adjudication MOA-Explain adjustments to claims paid on RA/EOB Medicare Secondary Payer MSP Overpayments-Credits must be returned to the payer Pending-Payer waiting for information before making a payment decision Prompt-Pay-Laws-Obligate state licensed carriers to pay claims within a certain time frame Remittance Advice RA-Group of claims RA Remark Codes REM-Explain adjustment to claims paid on RA/EOB Reason Codes –RC Reconciliation-Making sure all totals on RA/EOB check out mathematically. Ex-total amount billed-adjustment-patient responsibility=payment Utilization Review-Conducted by payer to check medical necessity of claim after claim is transmitted