Document
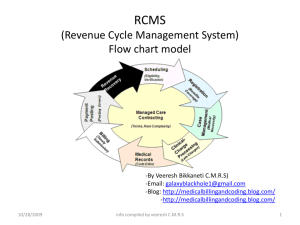
advertisement

Capario & CureMD Partnering to bring clients the best solution for streamlining workflow & increasing cash flow Who is Capario? • Capario has been providing revenue cycle management services to providers for more than 20 years • Easy-to-use, yet advanced, portal toolset that fits seamlessly into existing workflow • Real-time technology that integrates with any practice management system • World-class customer service – Dedicated Support, Enrollment, and Account Manager • EHNAC accredited • CORE Phase I & II certified Reputation of Excellence In recent KLAS® surveys of Capario customers: 100% said they would buy from us again 100% said that Capario is a part of their long-term plans 100% say that we keep our promises. What services do we offer CureMD customers? • Electronic Claims – Both Professional and Institutional – Worker’s Comp with or without attachments • Electronic Remittance Advice (ERA) – ERA is linked to the claim in CaparioOne • Real-Time Eligibility & Claim Status Inquiry • Correct Coding & Medical Necessity Editing (CCI/MNC) • CaparioOne RCM Services – Data is stored for 14 months • Paper Claims Services – Paper to EDI – Secondary Paper Claims & EOB Paper Claim Services Going “Electronic” is now easier than ever Paper to EDI By using Capario’s Paper to EDI service, you can send more of your claims electronically without going through the timeintensive task of researching payer IDs and addresses • It’s easy! • – Send the claim electronically to Capario using the payer ID of PAPER – Capario will perform an address match using the address on your claim and our database of payers. If the system makes a match, we will send the claim electronically, making adjudicating that claim fast and easy. – Once the claim is sent, you will be notified to update your system with the appropriate electronic payer ID. – If the system does not make a match, Capario will take on the task of printing and sending on paper for you. Automating Secondary Paper Claims By using Capario’s secondary paper claims service you can eliminate the daunting task of finding the primary EOB, making a copy and attaching it to the secondary claim prior to mailing. • It’s easy! • – Send your secondary claim electronically to Capario using the payer ID of PAPER, ensuring you have included the necessary primary payment information – Capario will generate a primary EOB based on the payment information in the claim and send the secondary claim along with the primary EOB to the payer for processing Would you like more information? Stop by the Capario booth or contact CureMD at 212-509-6200