Ventilator Associated Pneumonia Reduction in a Medical ICU
advertisement

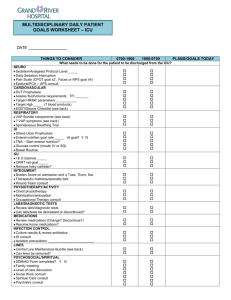
Ventilator Associated Pneumonia Reduction in a Medical ICU Bela Patel, MD Tammy Campos, RN, MSN Ruth Siska, RN B e l a P a t “Nosocomial” Infections • Nosocomial Infections – Not present or incubating upon admission to the hospital (48hr rule) • Preferred: Hospital Acquired Infections (HAIs) • 5-10% of patients admitted to hospital or 2 million patients • 88,000 deaths per year • Costs exceed 4.5 billion/year • 1 outbreak per 10,000 discharges From a public health issue to… A very public issue On the horizon for us • Texas reporting – Law passed requiring mandatory reporting of HAI to TDSHS starting 2008 – Rates will be publicly available • Federal reporting – Bill introduced requiring mandatory reporting to CDC through NHSN – New national guidelines on infection control 2008 • Medicare – SCIP as core measure – Lower rate reimbursement for patients with HAI starting 2008 VAP • Leading cause of death amongst hospitalacquired infections • Mortality 46% compared to 32% percent for ventilated patients who do not develop VAP • Increased ventilator days • Increased ICU LOS VAP defined • Patients mechanically ventilated for greater than 48 hours • Exhibit at least 3 or 5 following symptoms: – Fever – Leukocytosis – Change in sputum (color and/or amount), – Radiographic evidence of new infiltrates – Worsening oxygen requirements CDC 2003 Cost of VAP at MHH Cocanour, et al. Surgical Infections 2005. Prognosis VAP prevention “Vent Bundle” • Suctioning • Head of bed > 30o • Oral care • “Sedation holiday” Memorial Hermann -MICU • 16 bed unit admitting 1100 patients per year • 60% ventilated >3 days putting them at greater risk for VAP • Chief diagnoses include septicemia, respiratory failure, HIV/AIDS, renal failure, and multisystem organ failure secondary to multiple co-morbid conditions • Previous improvement work had made respectable reductions in VAPs from 2-3 per month to <10 per year, however it was felt more was achievable Aim and Measures Aim To reduce VAPs in the MICU to Zero within six months. Measures • Reduction in number of VAPs per 1000 ventilator days • Increased compliance with all aspects of the ventilator bundle. Where to start? MICU - VAP Fishbone People Policies Believed “Zero” was not possible Lack of communication between unit Nursing, RT and MDs Inconsistent in practice recommendations Lack of communication about policy and processes PRN staff and off service physicians did not capture importance “This is an expected complication” Didn’t know rates Policy not readily available “Our patients are too sick” Thought we were good enough No understanding of national benchmarks Isolation equipment not readily available Oral hygiene supplies not readily available Supplies No way to track oral care Off service patients not following protocol Processes Ventilator Associated Pneumonia Occurs Inconsistent bundle implementation Staff misunderstand bundle elements Lack of accountability for bundle implementation Interventions: Education • MICU “Huddles” on VAP and mortality • Posted rates in the unit for staff and MDs to see • Posted rates in public areas for patients and family members to see • Reviewed bundle compliance regularly in multidisciplinary team meetings • Reviewed compliance and VAP rates at local and system critical care committees Interventions: Implementation • Developed physician Rounding Tool to address VAP bundles • Appointed unit champions to assure patients were out of bed on daily basis • Formalize oral care process using chlorahexadine • Trained Patient Care Assistants (PCAs) in oral care • Mandated that oral care be a shared responsibility by RNs, Respiratory Therapists and PCAs increasing oral care from 4 times per day to 10 times per day • Computerized reminder alert for the care team • Located all oral care supplies near ventilators • Located isolation supplies –gowns, gloves, masks at entrance to every patient room Interventions: Implementation • Increased isolation practices for all infected patients to include booties, head coverings • Implemented glycemic protocol to keep glucose between 80 and 150 • Implemented automatic insulin drip for all patients who had 2 consecutive finger sticks above 150 • Implemented standardized sedation protocol • Improved Sedation holiday practices by team approach to assessment • Improved transportation practices Interventions: Audits • Implemented daily manager rounds to assure bundle compliance • Assured compliance with unit protocols by PRN staff and consulting MDs • Implemented a mini-RCA process for all VAPs to detect specific patient characteristics and system risk factors • Infectious Disease Dept conducts random weekly audits for bundle compliance • Infectious Disease Dept reviews all cases to diagnose VAPs based on CDC criteria Results: Bundle Compliance VAP Bundle Compliance - Jan06-Jul09 100 Percent compliance 95 90 85 80 75 70 Variable HOB Sxn Oral Care Peptic Ulcer Disease Px Sedation Holiday DVT PX 65 Q1-06 Q2-06 Q3-06 Q4-06 Q1-07 Q2-07 Q3-07 Q4-07 Q1-08 Q2-08 Q3-08 Q4-08 Q2-09 Q2-09 Does “vent bundle” work? More to do: FMEA • Aspiration during transport • Cuff leaks • Unplanned extubations requiring reintubation Results: VAP Rate Results: Overall • VAP rate went from 8-12 per year to zero within three months. • No VAPs have occurred in the MHH-TMC MICU for 26 consecutive months • Compliance with all aspects of the VAP bundle is between 98 - 100%. Results: Cost Savings • A financial analysis completed by our infectious disease and financial departments concluded that a VAP in any of our ICUs adds $57,000 in additional costs for additional antibiotics, ventilator time and ICU stay. • Cost avoidance for this project based on avoiding 8 VAPs per year is $456,000. Sustainability • Takes a Village to raise a “Zero” – Culture Changed • • • • Goal became Expectation Work flow changes became routine Reporting of “near misses” Created a highly functioning multidiciplinary team Conclusions and Next Steps • With concerted and focused effort “zero” is possible as an outcome. • As with any major improvement, the challenge is to maintain this level of performance. • Build on this methodology to achieve similar improvements for other hospital acquired infections in the Intensive Care Units. Acknowlegements • UT Divisions of Critical Care, Pulmonary and Sleep Medicine • MHH ICU Nursing Staff • MHH Respiratory Therapy • MHH Nutrition Support • UT-MHH Academy of Patient Safety & Effectiveness