MH Presentation
advertisement

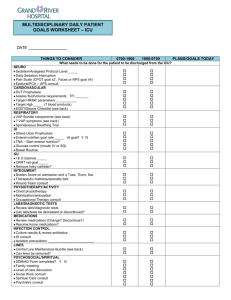
The Eradication of VAP in Scotland Martin Hughes Nov 2010 Plan • • • • • • • Definition Diagnosis Importance Strategies to reduce VAP Why don’t they work? What does work? Eradication in Scotland Definition • Inflammation of lung parenchyma > 48 hours post intubation, due to organisms not present or incubating at the time mechanical ventilation was commenced. • Early onset within first 4 days: usually due to antibiotic sensitive • Late onset > 5 days: commonly multi-drug resistant pathogens. Pathophysiology • Aspiration of pathogenic organisms from the oropharynx. • Normal flora replaced by pathogenic organisms (S. aureus, P. aeruginosa, H. influenzae, and Enterobacteriaceae (e.g. E. coli, Proteus, Enterobacter, Klebsiella, Serratia) • This change directly related to the severity of illness • Mixed infection in 50% • ‘Endotracheal tube associated pneumonia’ Diagnosis • • • • • • • • • Clinical Pulmonary Infection Score (CPIS) Temperature Leucocyte (cells/µL) PaO2/FiO2 (mmHg) CXR Tracheal secretions Culture 89% sensitive; 47% specific Rx CPIS > 6, stop if < 6 at day 3. Diagnosis • BAL, PSB, PCS • BAL cultures have a high sensitivity and specificity, resulting in a high positive predictive value. • 104 CFU/mL is usual threshold for BAL cultures. • More expensive • Complications • Less Antibiotics? Diagnosis • No gold standard • A Randomized Trial of Diagnostic Techniques for Ventilator-Associated Pneumonia. The Canadian Critical Care Trials Group. N Engl J Med 2006; 355:2619-2630, 2006 • No difference in mortality or antibiotic use • Excluded known MRSA/pseudomonas Importance • Incidence 9 – 28% • Risk per day: 3% day 5, 2% day10, 1% day 15 • Prolonged ventilation and ICU stay • 50% antibiotics in ICU for respiratory infections • Attributable mortality debated • Common sense? Strategies to reduce VAP • Elevation of bed • One study (1+), 90 pts, 1999. NNT of 4-5 to prevent one VAP • Daily sedation break • One study (1+), 150 pts, 2000. 2.4 vent days, 3.5 ICU days saved • More recently – sedation break + weaning assessment. http://www.sicsebm.org.uk Evidence • Sub-glottic ETT: • One review, 4 studies, Grade A recommendation, NNT 12 to prevent one VAP • Chlorhexidine oral care: • One meta- analysis. NNT 14 to prevent one VAP. Evidence • Weaning trial: – In combination with sedation holiday – One study (1+) 336 patients. Daily sedation holiday and weaning trial. • NNT Death (1 yr) 7 • Reduced ICU & hospital stay Others • NIV – avoiding intubation • Kinetic beds – no evidence • HME vs Heated Water Humidification – equally effective • SDD? Bundles • Structured way of improving the processes of care and patient outcomes • Small, straightforward set of evidencebased practices • Three to five in set - when performed collectively and reliably, have been proven to improve patient outcomes Bundles • • • • • • Every patient, every time. ‘All necessary and all sufficient’ Level 1 evidence All-or-nothing measurement of elements At a specific place and time Success means the whole bundle Safe: Timely: reduce waits and delays for those who receive and give care safety is a system property Efficient: avoid waste Quality In Effective: evidence based and applied to all who could benefit ICU Equitable: care does not vary in quality Patient Centered: care that is respectful and responsive to individual patient preferences and needs SRI Experience – Nov 2005 • VAP Prevention Bundle • 30 - 45o positioning • daily sedation holiday • daily weaning assessment • chlorhexidine mouthwash • subglottic aspiration tube • tubing management – appropriate humidification – avoidance of contamination Additionally • S/C enoxaparin pre-printed • Ranitidine pre-printed • Enteral feeding encouraged – if tolerated ranitidine cessation considered. SRI experience • At launch – – – – – Consultant buy in Laminated charts by every bed space Unit posters Surveillance programme (Helics) Ahead of the game nationally Job done? • What is the VAP rate? • What is the bundle compliance? • Hawe, Ellis, Cairns, Longmate ICM, 2009 G chart 350 250 200 Upper control limit (3SDs) 150 Upper warning line 100 50 Centreline (mean) 67 64 61 58 55 52 49 46 43 40 37 34 31 28 25 22 19 16 13 10 7 4 0 1 Number of at risk ventilation days between. 300 Process Postinterventions FV VAP Bundle (*SICS Bundle) * Patient at 30 -45 Chi-squared p value (Nov 2006 vs Oct 2007) Nov 2006 May 2007 Oct 2007 54% 80% 94% <0.001 Subglottic ETDT 72% 92% 92% <0.001 * Oral chlorhex 8% 94% 100% <0.001 Tubing/HMEF 98% 98% 100% 0.31 * Daily weaning plan * Sedation stop 52% 72% 72% 0.039 72% 86% 82% 0.23 All elements 0% 48% 54% <0.0001 o o Problem? • Passive interventions don’t work • Educational interventions to reduce VAP • Structure, Process, Outcome Active Implementation • Education: workshops: definition, epidemiology, pathogenesis, risk factors, consequences of VAP, evidence-base for the bundle. • Written material distributed. • Over 90% of the unit’s medical and nursing staff by April 2007. • Repeat cycles of process and outcome measurement and feedback. Sequential Process Measurements Baseline FV VAP Bundle (*SICS Bundle) * Patient at 30 -45 Postinterventions Chi-squared p value (Nov 2006 vs Oct 2007) Nov 2006 May 2007 Oct 2007 54% 80% 94% <0.001 Subglottic ETDT 72% 92% 92% <0.001 * Oral chlorhex 8% 94% 100% <0.001 Tubing/HMEF 98% 98% 100% 0.31 * Daily weaning plan * Sedation stop 52% 72% 72% 0.039 72% 86% 82% 0.23 All elements 0% 48% 54% <0.0001 o o 67 64 61 58 55 52 49 46 43 40 37 34 31 28 25 22 19 16 13 10 7 4 1 Number of at risk ventilation days between. 350 Study Period 300 250 200 150 100 50 0 Passive Sept 2005 Feb 2007 patients ventilated for > 48hrs Active March – Dec 2007 374 215 2556 1327 episodes of VAP 49 10 VAP/1000 vent days 19.17 7.5 4.5 5.0 (112/374) 30% (49/215) 23% Vent days Median LOS Mortality rd=11.6 99% CI 2.3-21.0 rr=0.39 99% CI 0.16,0.96) p=0.06 Lessons • Passive implementation of the VAP prevention bundle failed. • Compliance improved during an active multimodal implementation. • This was associated with a significant reduction in the occurrence of VAP. Since then……………….. The Scottish Patient Safety Programme VAP Prevention Bundle Sedation reviewed and stopped if appropriate Y N Exclusion Patient assessed for weaning and extubation Y N Exclusion Supine position avoided Y N Exclusion Chlorhexidine 1-2% QID Y N Exclusion Use of subglottic drainage ETT Y N Exclusion Post spsp improvements VAP: % All Bundle Compliance % 100 90 80 70 60 50 40 30 20 10 0 96 100 78 62 41 March April May Month 08 June July Calendar days between VAP acquisition Sep 2005 - Jun 2009 calendar days between UCL CL UWL 180 Scottish Patient Safety Programme Calendar days between 160 140 120 100 Active intervention & compliance feedback Passive intervention period 80 60 40 20 0 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 41 43 45 47 49 51 53 55 57 59 61 63 65 67 69 71 73 75 77 VAP Incidence: Bundle Compliance 8 HELICS surveillance 90% 6 70% VAP bundle prompts added to daily goals sheet. 5 60% Continuous measurement initiated 4 50% VAP - Long term pt vent for more than 150 days 3 Patient Safety Programme begins 40% VAP - poorly compliant pt, refusing to sit up refusing chlohex. Handling trachy and tubing. Not clear cut! VAP - Pt constantly pulling at trachy, poorly compliant with head up & mouthwash 30% 2 20% 1 10% Oct-09 Sep-09 Aug-09 Jul-09 Jun-09 May-09 Apr-09 Mar-09 Feb-09 Jan-09 Dec-08 Nov-08 Oct-08 Sep-08 Aug-08 Jul-08 Jun-08 May-08 Apr-08 Mar-08 Feb-08 Jan-08 Dec-07 Nov-07 Oct-07 Sep-07 Aug-07 Jul-07 Jun-07 May-07 Apr-07 Mar-07 Feb-07 Jan-07 Dec-06 0% Nov-06 0 Oct-06 VAP Incidence 80% Tw ice daily w ean screen sticker added to 24hr chart Active period: Bundle implementation, audit & education Bundle Compliance 7 100% VAP – Key points • Evidence is the starting point • Implementation is difficult – efficacy vs effectiveness • Process measure identifies failings • SPSP methodology leads to sustained process improvement VAP – key points • • • • • • Education Feedback Process measurement / management You need the correct clinicians The result is outcome improvement Resources – without the above, bundles are “futile” VAP - eliminated • VAP still here • So rare that we can now discuss the reasons for individual cases • Huge reduction in the problem • Scottish ICU clinicians and SPSP/IHI • Effective healthcare does not need to cost more