InteractionofMultipleSedatingMedications
advertisement

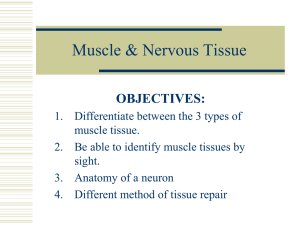
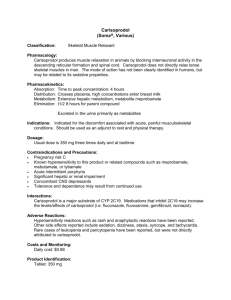
Interaction of Multiple Sedating Medications There are many classes of sedating medications that can interact with one another to amplify the sedative, dysphoric, respiratory depressant properties of the many sedating drugs on the market. Within the class of muscle relaxants, are many potential interactions when these medications are mixed with opioids. They potentiate the respiratory depressant effects of the opioids and may lead to severe adverse effects. Some doctors are unaware of the potential for interactions with medications that are not opioids, that could nonetheless produce life threatening respiratory depression or effects. The supplements also have potential sedation from their effects yet in many cases these are not revealed by the patient to the physician unless the physician inquires about this drug class. The recognition that sedating drugs are spread across many drug classes and often prescribed by several simultaneous physicians/practitioners may enhance the safety of patients, especially when being prescribed opioids. Muscle Relaxants Cyclobenzaprine (Flexeril) Was introduced in the US in 1977, it has a chemical structure almost identical to amitriptryline (Elavil) and shares some of the same properties. The structure of cyclobenzaprine is shown on the left while amitriptyline is on the right. The only difference is one double bond in the central ring. Functionally, it behaves like a tricyclic producing sedation in 39%, dry mouth in 27%, dizziness in 11% and between 1-3% develop fatigue, constipation, nausea, dyspepsia, headache, unpleasant taste, and confusion. Agitation is commonly seen in the elderly. Urinary retention occurs in less than 1%. Overdose may cause bundle branch blocks, congestive heart failure, confusion, visual hallucinations, agitation, hyperactive reflexes, muscle rigidity, vomiting, and hyperpyrexia. It is contraindicated in patients with hyperthyroidism, recent myocardial infarction, bundle branch block or heart block, arrhythmia, or congestive heart failure. It seems to work at the brainstem influencing both muscle tone (gamma) and muscle contraction (alpha) motor systems by its actions on the locus cereleus causing an increased release and probable reuptake inhibition of norepinephrine in the ventral horn of the spinal cord thus inhibiting motor neurons. Cyclobenzaprine also is related to the antihistamine cyproheptadine and causes inhibition of descending serotonergic systems in the cord by blocking 5-HT 2a and 2c receptors thereby inhibing the alpha motor neurons in the ventral spinal cord. It is not useful for upper motor neuron or central spasticity conditions such as cerebral palsy. The drug has a half life of 18 hours but up to 2-3 days so dosage has an enormous impact on blood and tissue levels. It is metabolized to the glucuronide and excreted by the kidney. Withdrawal symptoms are mild on sudden cessation. CAUTION should be used if administered with tricyclic antidepressants, antihistamines, or other sedating drugs, or when used in the elderly (agitation). Use with tramadol may initiate seizures. CONTRAINDICATIONS: arrhythmias, recent MI, CHF. BEFORE PRESCRIBING: ECG and check for history or symptoms of CHF or hyperthyroidism Baclofen (Lioresal) Baclofen (left below) is an analog of GABA (right below). The oral form was first synthesized in 1962, released to the market 1972, and obtained FDA approved in 1977 and the injectable/intrathecal forms in 1992. It exerts muscle relaxant properties as an agonist at the GABA-B receptors (protein G linked receptor resulting in opening of potassium channels leading to hyperpolarization and stops neurotransmitter release. Therefore, GABA-B receptors are inhibitory neuroreceptors. The drug is only metabolized 15% and is excreted largely unchanged in both feces and urine. It has a half life of 1.5-4 hours. It is used to treat spasticity from cerebral palsy, multiple sclerosis, and spastic movement disorders. It is also used to treat hiccoughs, alcoholism and cocaine abuse, and temperature rise from MDMA. In mice studies it has the potential to reducing craving for nicotine. While it has been shown to attenuate neuropathic pain, diabetic peripheral neuropathy pain, and migraine pain, continued use results in tolerance to the drug, therefore it may have more use in the acute neuropathic pain or acute migraine treatment with subsequent dosage cessation. It is not recommended for use in those with CVA or Parkinson’s disease. Adverse reactions include drowsiness (up to 63%), dizziness (5-15%), weakness (5-15%), fatigue (24%), confusion (up to 11%), insomnia (up to 7%), nausea (up to 12%), constipation (up to 6%). Hypotension was reported in up to 9%. Higher doses lead to euphoria, excitement, hallucinations, slurred speech, coordination disorders, tremors, rigidity, dystonia, ataxia, miosis, diplopia, and seizures. Overdose produces coma, hypothermia, bradycardia, seizures, and hyporeflexia. Maximum dosage is usually 80mg per day and especially the elderly may have significant ataxia and confusion on that dosage. Withdrawal symptoms may be severe (hallucinations) or even life threatening (seizures) so the drug should be tapered if the patient has been on the medicine for more than a few days. BEFORE PRESCRIBING: Check for hx of parkinsons or CVA, other sedating drugs, and supplements DRUG INTERACTIONS: Phenibut is a supplement drug sold in the US and is unregulated by the FDA. It is a phenyl derivative of GABA and acts on the GABA-B receptor and at higher doses on the GABA-A receptor producing sedation. It is a drug frequently prescribed for “stress, anxiety, or insomnia” when less sedation than benzodiazepines is required. It is prescribed 250-1500mg BID. GHB (Xyrem) is a drug acting as an excitatory agent on the GHB receptors and weak inhibitory agent on the GABA-B receptors. It is used legally as a Schedule II drug approved only for the treatment of catalepsy associated with narcolepsy. As a street drug it is used in the rave scene and clubs acting as both a stimulant and aphrodesiac, but when mixed with alcohol becomes a date rape drug and can have fatal respiratory depression. It is very difficult to detect postmortem or in urine or blood, but can be detected in hair analysis. It is easily synthesized in home labs and may also be produced in the stomach and blood from the prodrugs gamma-butyrolactone (GBL) or 1,4 butanediol. GHB causes euphoria, disinhibition, and enhanced sensuality at lower doses while higher doses cause vomiting, drowsiness, agitation, respiratory depression, amnesia, unconsciousness, and death. Ref: http://physrev.physiology.org/content/84/3/835.full Tizanidine (Zanaflex) First approved for use by the FDA in 1996, it is a central acting alpha 2 adrenergic agonist in the same class as and structurally somewhat related to clonidine (Catapress). Other alpha 2 adrenergics include guanabenz (Wytensin), guanfacine (Tenex) and methyldopa (Aldomet). It is used to treat muscle spasms, low back pain/central spasticity, and migraine headaches/chronic tension headaches off label. It works by inhibiting release of excitatory amino acids and inhibits cerebralspinal pathways, probably due to action on polysynaptic pathways. Its effect on BP is short lived after a single dose and is at most 1/10 that of clonidine. Has a half life of 2.5 hours and is metabolized 95% by CYP1A2 with 60% excreted renally. Max dose is 36mg a day. Adverse effects (dose related) include dry mouth, somnolence/sedation, asthenia, and dizziness. CONTRAINDICATED WITH CIPRO or other FLUOROQUINOLONES, FLUVOXAMINE (LUVOX), CIMETADINE, AMIODARIONE, or VERAPAMIL. Oral contraceptives reduce clearance by 50%. BEFORE PRESCRIBING: LFTs and recheck 2-4 weeks after initiation, check for other alpha blockers and history of hypertension treated with medications. It has enhanced effects on lowering blood pressure in those with orthostatic hypertension. Carisoprodol (Soma) First approved by the FDA in 1959, is a Schedule IV controlled substance used to treat non-upper motor neuron lesion induced muscle spasms. It is metabolized by the CYP450 system into meprobamate, that is an active major tranquilizer, and therefore has some abuse potential. Carisoprodol Meprobamate It functions by interrupting neuronal communication with the reticular system in the spinal cord. The drug also potentiates the analgesic and side effects of opioids, making it both useful and dangerous at the same time when used in combination with opioids. Therefore starting a person on carisoprodol that is already taking opioids can lead to potential overdose. It is used as a date rape drug in combination with benzodiazepines and is used recreationally due to heavy sedation, relaxation, and anxiolytic effects, and with opioids due to the potentiation of their effects. The effects on respiratory depression can be profound with opioids or with alcohol. Dosage 350mg QID typical CONTRAINDICATIONS: elderly (relative), alcohol use, history of addiction (relative) Withdrawal effects are usually mild. BEFORE PRESCRIBING: Consider drug screening urine or blood, and obtain history of substance abuse. Those hospitalized previously due to drug related overdose or significant respiratory depression effects from medications should not be given carisoprodol. Consider trying other alternatives before resorting to carisoprodol. Metaxolone (Skelaxin) Approved initially in 1962 by the FDA, it was not heavily marketed until after 2000. The mechanism as a muscle relaxant is unknown but appears due to generalized central nervous system depression. Its half life averages 9 hours. The onset is relatively slow with a peak concentration in the blood occurring at 2.5 hours in fasted patients but 4.2 hours in those taking the medication with food. Also, taking the medication with food will double its concentration in the blood. It is metabolized by 4 major different cytochrome P450 enzymes so action of other drugs on one enzyme will be less likely to affect the overall metabolic rate. Caution using with triprolidine or other H1 blockers or in patients with drug induced anemia. Respiratory depression may result when used with other sedating drugs such as benzodiazepines, opioids, other muscle relaxants, or barbiturates. Less sedation is seen than other commonly used muscle relaxants. Max dose 3200mg/day Chlorzoxazone (Parafon Forte) Approved by the FDA in 1958 indicated for relief of discomfort associated with acute painful musculoskeletal conditions. It acts primarily in the CNS by undefined mechanisms and may produce relief due to its sedative properties. It is not chemically related to other commonly found medications. Dosage 250-750mg QID The half life is 1.1 hours and it is metabolized by the liver. Adverse effects: dizziness, drowsiness, produces liver dysfunction, red or orange urine, GI irritation Overdose symptoms include vomiting and diarrhea, drowsiness, lightheadedness. DTRs may be decreased or absent and respiratory depression with rapid irregular respirations is seen. CONTRAINDICATION: Hepatic impairment BEFORE PRESCRIBING: LFTs and 2-4 weeks after first dose then long term Orphenadrine (Norflex) It was first approved by the FDA in 1959. Orphenadrine (left below) is an antihistamine structurally almost identical to diphenhydramine (right below). The only difference is one single methyl group on the benzene ring. Therefore its properties are virtually identical to that of diphenhydramine (Benadryl). It binds to both NMDA receptors and has a mild antihistaminic/local anesthetic effect, mainly centrally rather than peripherally. Indications are for the treatment of drug induced parkinsonism, motor disturbances induced by neuroleptic drugs, and in the treatment of painful muscle spasms. The plasma half life is long, over 14 hours and after 24 hours, less than 1/3 of the drug or its metabolites have been excreted primarily as demethylated hepatic metabolites. It is available as a component of Norgesic or Orphengesic. Adverse effects are common: drowsiness, dry mouth, urinary retention, increased intraocular pressure. Less commonly is GI irritation, tachycardia, hypersensitivity reaction (high doses), and rare aplastic anemia. Because of the long half life, it is prudent to reduce doses or avoid this medicine in the elderly and in patients taking medications with anticholinergic effects (TCAs, antihistamines) and to using orphenadrine with haloperidol. BEFORE PRESCRIBING: Check history for glaucoma, myasthenia gravis, and cardiospasm (esophageal reflux/obstruction with dysphagia). Avoid the drug in these patients. Dose: 100-200mg BID Methocarbamol (Robaxin) Methocarbamol was approved by the FDA in 1957 after approving guaifenesin in 1952. Methocarbamol (left) is structurally related to guaifenesin (right). The drug is the carbamate of guaifenesin, but does not produce guaifenesin as a metabolite. The drug is metabolized in the liver by hydroxylation and demethylation followed by conjugation then renal excretion. The half life is a very short 1.2 hours. It may produce drowsiness (but less than most other muscle relaxants), dizziness, blurred vision, and fever. Slowing of the heart rate, severe skin rash, nausea/vomiting, difficulty urinating, and clumsiness may occur less commonly. May produce black, brown, or green urine, cause mental status impairment, and possibly exacerbate myasthenia gravis patients. CAUTION: prescribing for the elderly with this drug due to side effects. BEFORE PRESCRIBING: Check history for myasthenia gravis. Dose 750mg QID chronic dosing. Respiratory depression may result when used with other sedating drugs such as benzodiazepines, opioids, other muscle relaxants, or barbiturates. However, given the short half life, the medication may be safer to use than other muscle relaxants.