Analgesic, sedation, muscle relaxant
advertisement

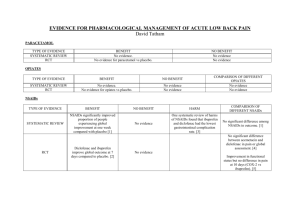
Analgesics An analgesic (also known as a painkiller) is any member of the group of drugs used to relieve pain. In choosing analgesics, the severity and response to other medication determines the choice of agent; the WHO pain ladder, originally developed in cancer-related pain, is widely applied to find suitable drugs in a stepwise manner. The analgesic choice is also determined by the type of pain: for neuropathic pain, traditional analgesics are less effective, and there is often benefit from classes of drugs that are not normally considered analgesics, antidepressants and anticonvulsants. such as tricyclic Major classes: Paracetamol and NSAIDs: The exact mechanism of action of paracetamol is uncertain, but it appears to be acting centrally rather than peripherally (in the brain rather than in nerve endings). Aspirin and the other non-steroidal anti-inflammatory drugs (NSAIDs) inhibit cyclooxygenases, leading to a decrease in prostaglandin production. This reduces pain and inflammation (in contrast to paracetamol and the opioids). also Paracetamol has few side effects and is regarded as safe, although intake above the recommended dose can lead to liver damage, which can be severe and life-threatening, and occasionally kidney damage. Paracetamol is usually taken orally or rectally, an intravenous preparation introduced in 2002 has been shown to improve pain relief and reduce opioid consumption in the perioperative setting. NSAIDs predispose to peptic ulcers, renal failure, allergic reactions, and occasionally hearing loss, and they can increase the risk of hemorrhage by affecting platelet function. The use of aspirin in children under 16 suffering from viral illness has been linked to Reye's syndrome. COX-2 inhibitors: These drugs have been derived from NSAIDs. The cyclooxygenase enzyme inhibited by NSAIDs was discovered to have at least 2 different versions: COX1 and COX2. Research suggested that most of the adverse effects of NSAIDs were mediated by blocking the COX1 enzyme, with the analgesic effects being mediated by the COX2 enzyme. The COX2 inhibitors were thus developed to inhibit only the COX2 enzyme (traditional NSAIDs block both versions in general). These drugs (such as rofecoxib, celecoxib and etoricoxib) are equally effective analgesics when compared with NSAIDs, but cause less gastrointestinal hemorrhage in particular. After widespread use of the COX-2 inhibitors, it was discovered that most of the drugs in this class increased the risk of cardiovascular events by 40% on average. This led to the withdrawal of rofecoxib and valdecoxib, and warnings on others. Etoricoxib seems relatively safe, with the risk of thrombotic events similar to that of non-coxib NSAID diclofenac. Narcotic Analgesics: There are two types of narcotic analgesics: the opiates and the opioids (derivatives of opiates). Opioids are any medication which bind to opioid receptors in the central nervous system or gastointestinal tract. There are four broad classes of opioids: Endogenous opioid peptides (produced in the body: endorphins) Opium alkaloids (morphine, codeine) Semi-synthetic opioids (heroin, oxycodone, hydrocodone, dihydrocodeine, hydromorphone) Fully synthetic opioids (pethidine , fentanyl, tramadol) Opioids are used in medicine as strong analgesics, for relief of severe or chronic pain. There is no upper limit for the dosage of opioids used to achieve pain relief, but the dose must be increased gradually to allow for the development of tolerance to adverse effects (for example, respiratory depression). Some people with intense pain get such high doses that the same dose would be fatal if taken by someone who was not suffering from pain." There have been debates over the addictive potential of opioids vs. the benefit of their analgesic properties for treating non-malignant chronic pain, such as chronic arthritis. Some experts believe opioids can be taken safely for years with minimal risk of addiction or toxic side effects. The enhanced quality of life which opioids may provide the patient must be considered. Common side effects and adverse reactions: nausea vomiting drowsiness dry mouth miosis (contraction of the pupil) orthostatic hypotension (blood pressure lowers upon sudden standing) urinary retention constipation and/or fecal impaction Most severe side effects and adverse reactions: respiratory depression fatal overdose Specific agents: In patients with chronic or neuropathic pain, various other substances may have analgesic properties. Tricyclic antidepressants, have been shown to improve pain in what appears to be a central manner. Anticonvulsants are used to treat neuropathic pain with differing degrees of success. Anticonvulsants are most commonly used for neuropathic pain as their mechanism of action tends to inhibit pain sensation. Sedatives A sedative or tranquilizer is a substance that induces sedation by reducing irritability or excitement. Hypnotic (also called soporific) drugs are a class of psychoactives whose primary function is to induce sleep and to be used in the treatment of insomnia, and in surgical anesthesia. At higher doses of sedatives may result in slurred speech, staggering gait, poor judgment, and slow, uncertain reflexes. Doses of sedatives such as benzodiazepines, when used as a hypnotic to induce sleep, tend to be higher than amounts used to relieve anxiety, whereas only low doses are needed to provide a peaceful and calming sedative effect. Types of sedatives: Barbiturates pentobarbital phenobarbital Benzodiazepines diazepam midazolam alprazolam Herbal sedatives cannabis Nonbenzodiazepine sedatives zaleplon zopiclone (Imovane, Zimovane) Antihistamines diphenhydramine Other chloral hydrate alcohol opiates and opioids Therapeutic use: Doctors often administer sedatives to patients in order to relieve the patient's anxiety related to painful or anxietyprovoking procedures. Although sedatives do not relieve pain in themselves, they can be a useful combination to analgesics in preparing patients for surgery. It is commonly given to patients before they are anaesthetized, or before other highly uncomfortable and invasive procedures like fiber optic bronchoscopy, cardiac catheterization, colonoscopy or MRI. They also increase tractability and compliance of children or demanding patients. Patients in intensive care units are almost always sedated (unless they are unconscious from their condition anyway). Dangers of combining sedatives and alcohol: Sedatives and alcohol are sometimes combined recreationally or carelessly. Since alcohol is a strong depressant that slows brain function and depresses respiration, the two substances compound each other's actions and this combination can prove fatal. Sedatives and amnesia: Sedatives can sometimes leave the patient with long-term or short-term amnesia. Lorazepam is one such pharmacological agent that can cause anterograde amnesia. Intensive care unit patients who receive higher doses over longer periods, typically via IV drip, are more likely to experience such side effects. Muscle Relaxant A muscle relaxant is a drug which affects skeletal muscle function and decreases the muscle tone. It may be used to alleviate symptoms such as muscle spasms, pain, and hyperreflexia. The term "muscle relaxant" is used to refer to two major therapeutic groups: neuromuscular blockers and spasmolytics. Neuromuscular blockers act by interfering with transmission at the neuromuscular end plate and have no central nervous system (CNS) activity. They are often used during surgical procedures and in intensive care and emergency medicine to cause paralysis. Spasmolytics, also known as "centrally acting" muscle relaxants, are used to alleviate musculoskeletal pain and spasms and to reduce spasticity in a variety of neurological conditions. While both neuromuscular blockers and spasmolytics are often grouped together as muscle relaxants Uses of muscle relaxants: - Use in intensive surgeries and emergency procedures to induce paralysis - Antispasmodic - Treats symptoms of fibromyalgia i.e. stiffness, fatigue, and body aches - Alleviate back pain and neck pain - Used as a treatment for tension headaches Commonly used muscle relaxants list: Carisoprodol: muscle relaxant that works by blocking the pain sensations from the nerves by acting on the central nervous system. It is used to temporarily relieve pain from muscle pain, spasms, sprains, and strains. It is also used as an antidepressant. Diazepam: aside from relieving muscle pains and spasms, it also alleviates acute alcohol withdrawal, convulsion, and anxiety related symptoms. It acts on the brain and nerves and produced a temporary calming effect on the user. Cyclobenzaprine: used to treat muscle spasm and pain associated with acute musculoskeletal conditions. Metaloxone: relatively strong muscle relaxants that produced little side effects, it is used to relax muscle and lessen muscle pain and spasms. Increased viability is impressed when taken with food. Methacarbamol: a central muscle relaxant used to treat skeletal spasm and helps to relax muscles and reduce muscle pains associated from sprains, strains, and muscle stress. The most common side effects of muscle relaxants are: Vision changes, such as double vision or blurred vision Dizziness, drowsiness Dry mouth Less common side effects, such as stomach cramps or pain, nausea and vomiting, constipation, diarrhea, hiccups, confusion, nervousness, restlessness, irritability, flushed or red face, headache, heartburn, weakness, and sleep problems also may occur and do not need medical attention unless they do not go away or they interfere with normal activities. More serious side effects are not common, but may occur. Anyone who experiences breathing problems, facial swelling, fainting, unusually fast or unusually slow heartbeat, fever, tightness in the chest, rash, itching, burning, red, or bloodshot eyes, or unusual thoughts or dreams after taking muscle relaxants should seek medical help. Muscle relaxants may interact with some other medicines. When this happens, the effects of one or both of the drugs may change or the risk of side effects may be greater. Anyone who plans to take muscle relaxants should let the physician know all other medicines, including over-the-counter medicines, that he or she is taking. or nonprescription Thank You