Diabetes in Pregnancy - Homerton University Hospital

Diabetes in pregnancy
Patient information
Intro….
What is gestational diabetes?
Sometimes women who are not known to have diabetes develop it during pregnancy. This is called gestational diabetes. It usually occurs after the 13th week of pregnancy and goes away after birth. Women with gestational diabetes have too much glucose (a type of sugar) in the blood which can lead to some complications in pregnancy.
How common is gestational diabetes?
Diabetes developing in pregnancy is very common affecting up to 18 in 100 pregnant women.
Who is at risk of developing gestational diabetes?
These factors put a woman at higher risk of developing gestational diabetes:
• being overweight with BMI 30 or higher
• twin pregnancy
• advanced maternal age - older than 35 years of age
• a family history of diabetes
• ethnicity, particularly if you are from a South Asian, Black Caribbean or Middle Eastern background
• having had a large baby before (over 4.5kg/9Ibs)
• polycystic ovary syndrome (PCOS)
• having had gestational diabetes before.
How will I be checked for diabetes?
We check all pregnant women for diabetes. If you have any of the above risk factors, we will check your blood glucose every time we see you in pregnancy. If your blood glucose starts to go up, we will then arrange a special test called glucose tolerance test.
This test is often used to diagnose gestational diabetes. It involves a blood test before eating anything in the morning (fasting); then again two hours after glucose drink. We also sometimes do this test when we suspect you may be carrying a big baby or if ultrasound scan shows a lot of water around your baby. If you have had gestational diabetes before we will recommend for you to monitor your glucose at home a few weeks earlier than you developed it last time.
How can gestational diabetes or preexisting diabetes affect my baby?
A good number of women with diabetes have uncomplicated pregnancies.
Occasionally it causes problems. It is therefore important to recognize it and to control the level of glucose in the blood .
Pregnancy
As you share a blood supply with your baby through the placenta, when your blood glucose is higher than normal, your baby also receives higher amounts of glucose. Storing this extra energy causes your baby to grow large and weak (macrosomia). There may be a lot of water around the baby (polyhydramnios). This increases the risk of premature labour. You also have an increased risk of developing pre-eclampsia.
Delivery
Large babies have more problems during delivery including shoulder dystocia. Shoulder dystocia is when the baby’s head has been born but one of the shoulders becomes stuck behind the mother’s pubic bone, delaying the birth of the baby’s body. If this happens extra help is needed to release the baby’s shoulders. This can occur in 8-10% of pregnancies complicated by diabetes. In great majority of cases the baby will be born promptly and safely.
Shoulder dystocia is an emergency and therefore when it does occur, speed is of the essence.
The baby’s shoulder needs to be released quickly so that that the baby’s body can be born and he or she can start breathing air into the lungs.
Your midwife will press the emergency bell to summon the other members of the team which include midwives, obstetricians and a doctor for your baby. It is important to remember that obstetricians and midwives who attend the birth are trained in how to deal with shoulder dystocia.
About one in ten babies will have some stretching of the nerves in the neck which may cause loss of movement to the arm. It is usually temporary and movement will return within hours or days. Permanent damage is rare. Even with the best care, in a few cases a baby can suffer damage if he or she did not get enough oxygen because delivery was delayed due to shoulder dystocia.
Mothers are also at risk of having a tear involving the back passage (third degree/ fourth degree tear). This will require repair in theatre and majority of women heal well after this.
More women with diabetes have a caesarean section than the average population. This may be a planned caesarean where the decision is made with you in clinic or an emergency when the need arises in labour.
Stillbirths are rare but more common in pregnancies complicated by poorly controlled gestational diabetes, particularly later in the pregnancy; induction of labour/planned caesarean therefore will be discussed with you.
Just after birth, your baby may have low blood glucose levels (called hypoglycaemia). This can happen if your baby has been making extra insulin to cope with the excess sugar from your blood. We will check for this and treat it if your baby’s sugar is low.
How can gestational diabetes affect me?
It can increase your chance of some problems during pregnancy or later in life, such as:
• pre-eclampsia — a condition which causes high blood pressure in pregnant women
• premature (early) birth
• induced labour
• having a caesarean section
• type 2 diabetes when you are older
• developing gestational diabetes in future pregnancies.
How is gestational diabetes managed?
Once diagnosed, you will be referred to a specialist clinic for the rest of your pregnancy. The risks to you and your baby can be lowered with good control of your condition with the help of the team of obstetricians, diabetic doctors, diabetic nurses, and dieticians. The specialist clinic takes place on Wednesday afternoons. Most women in this clinic will see different professionals and therefore each visit can take a while. We advise that you come with a healthy snack and a book. You may also be asked to have more scans of your baby.
The main way to treat gestational diabetes is through diet and increasing your activity level.
Your first step will be a referral to a dietician who will talk to you about eating well. You will then be taught how to check your blood glucose at regular intervals. If your blood glucose cannot be controlled by diet and increasing your activity level, you may need to take diabetes medication and /or have insulin injections to control your blood sugar.
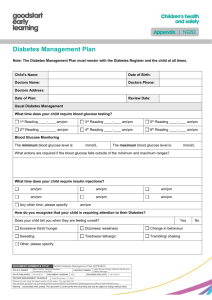
Testing your blood sugar
You will need to check your blood glucose several times a day and will be shown how to do this with a finger prick blood glucose meter. Keeping your blood glucose in the target range will help reduce the risks that are linked with having gestational diabetes.
Monitoring your blood pressure
As you are at increased risk of developing high blood pressure problems, we shall carefully monitor your blood pressure more frequently.
Common questions about gestational diabetes
How does gestational diabetes develop?
During pregnancy the body makes high levels of pregnancy hormones and in some women these can reduce the effectiveness of insulin. This is called insulin resistance. If the women's body cannot make enough insulin, or cannot use the body's insulin properly, her blood glucose rises resulting in gestational diabetes.
How will I have my baby?
Ideally you should have your baby between 37 weeks and 40 weeks depending on your individual circumstance. On occasion we recommend delivery earlier than 37 weeks. If your scans show that the baby is big, we will discuss the risks and benefits of vaginal birth, induced labour and caesarean section with you. When in labour, we will recommend delivery on the labour ward and for the baby’s heart beat to be continuously monitored. We will monitor your blood glucose as well.
What happens after birth?
In most women blood glucose returns to normal after the baby is born. Please talk to your diabetes care team about having your blood glucose checked three months after the birth of your baby to make sure that the diabetes has gone away.
Will I get gestational diabetes if I become pregnant again?
You are more likely to develop it again if you have had it before; but if you are overweight and lose weight, you can reduce your risk of developing it next time.
Will I get diabetes later in life?
Having had gestational diabetes does put you at a higher risk of developing type 2 diabetes later in your life. Keeping trim and doing moderate regular exercise reduces your risks. Having a diabetes check-up from your GP every year is sensible too.
Will my baby have diabetes?
If you had gestational diabetes, your baby will not have a higher risk of developing diabetes in childhood than any other baby. However, your baby has a higher risk of developing diabetes and obesity later in life. If you are worried about this, talk to your GP or health visitor.
Useful contacts
RCOG
Patient Advice and Liaison Service (PALS)
PALS can provide information and support to patients and carers and will listen to your concerns, suggestion or queries. The service is available between 9am and 5pm
Tel: 0208 510 7315
Textphone: 07584 445 400
Email: PALS@homerton.nhs.uk
For information on the references used to produce this leaflet, please ring 0208 510 5302, text:
07584 445 400 or email patientinformation@homerton.nhs.uk
If you require this information in other languages, large print, audio or
Braille please telephone the Patient Information Team on 0208 510
5302, text: 07584 445 400 or email: patientinformation@homerton.nhs.uk
Produced by: Podiatry Service
IMRS
Homerton University Hospital NHS Foundation Trust
Homerton Row, London E9 6SR
T: 0208 8510 5555
W: www.homerton.nhs.uk
E: enquiries@homerton.nhs.uk
Review date: September 2015
Next review date: September 2017