Pediatric Neurosurgery Scalp Block Guidelines
advertisement
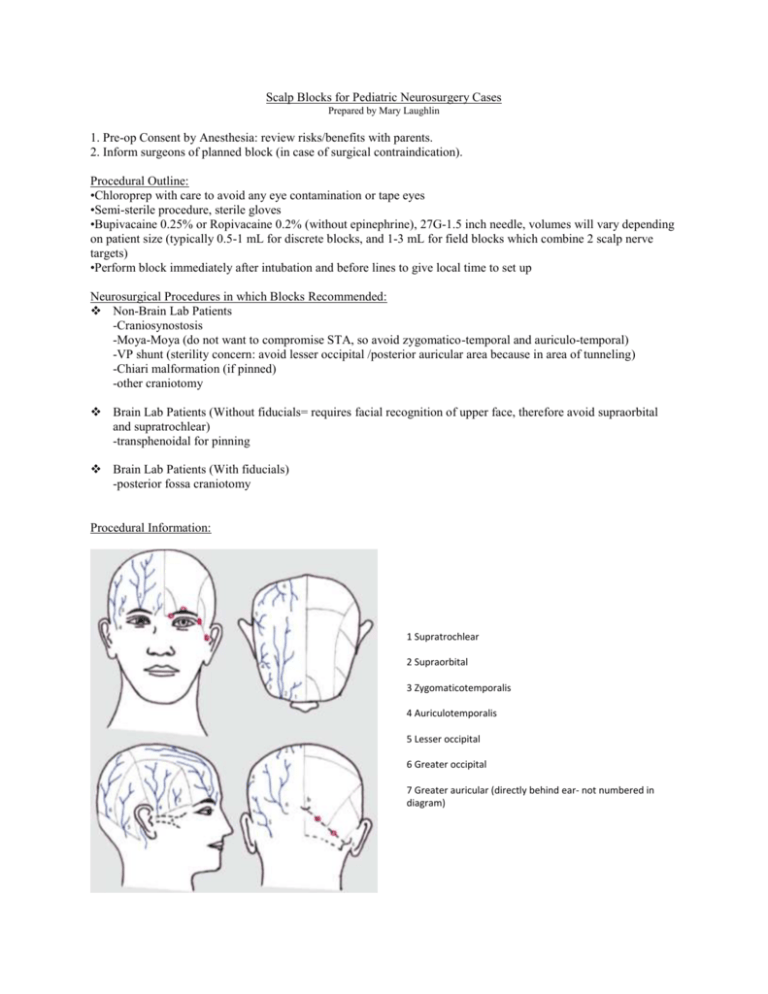
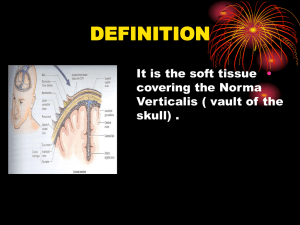
Scalp Blocks for Pediatric Neurosurgery Cases Prepared by Mary Laughlin 1. Pre-op Consent by Anesthesia: review risks/benefits with parents. 2. Inform surgeons of planned block (in case of surgical contraindication). Procedural Outline: •Chloroprep with care to avoid any eye contamination or tape eyes •Semi-sterile procedure, sterile gloves •Bupivacaine 0.25% or Ropivacaine 0.2% (without epinephrine), 27G-1.5 inch needle, volumes will vary depending on patient size (typically 0.5-1 mL for discrete blocks, and 1-3 mL for field blocks which combine 2 scalp nerve targets) •Perform block immediately after intubation and before lines to give local time to set up Neurosurgical Procedures in which Blocks Recommended: Non-Brain Lab Patients -Craniosynostosis -Moya-Moya (do not want to compromise STA, so avoid zygomatico-temporal and auriculo-temporal) -VP shunt (sterility concern: avoid lesser occipital /posterior auricular area because in area of tunneling) -Chiari malformation (if pinned) -other craniotomy Brain Lab Patients (Without fiducials= requires facial recognition of upper face, therefore avoid supraorbital and supratrochlear) -transphenoidal for pinning Brain Lab Patients (With fiducials) -posterior fossa craniotomy Procedural Information: 1 Supratrochlear 2 Supraorbital 3 Zygomaticotemporalis 4 Auriculotemporalis 5 Lesser occipital 6 Greater occipital 7 Greater auricular (directly behind ear- not numbered in diagram) Sensory innervation of the head is supplied by branches of the Trigeminal nerve (branches 1-4 listed above) and C2-C4 cervical roots (branches 5-7 above). Scalp blocks are all essentially subcutaneous field blocks which cover cutaneous innervation of the scalp (they do not cover the periosteal innervation which explains the hemodynamic response sometimes seen during pinning even after effective scalp blocks; this response is typically much milder than in the absence of scalp blocks, and can be supplemented with IV medication if appropriate). Scalp blocks can be accomplished individually by discrete subcutaneous injections at each of the 6 areas noted above in the diagram. These blocks can also be performed together as field blocks by combining them as follows: Supratrochlear and Supraorbital: along the brow line, insert through lateral 1/3rd of brow advancing needle subcutaneously toward medial brow border and injecting local as needle is withdrawn. Zygomaticotemporal (ZT) and Auriculotemporal (AT): injection from ZT site (1cm lateral and superior to canthus of eye above zygomatic arch) to AT site (1 cm anterior to the tragus). Insert needle at AT site and advance subcutaneously to ZT site, injecting local as needle is withdrawn. Lesser occipital (LO) and Greater auricular (GA): injection from the LO site (lateral to occipital artery along superior nuchal line) toward the GA site(1 cm posterior to ear at the level of the tragus). Insert needle at LO site advancing subcutaneously to GA site, inject local as needle is withdrawn. Greater occipital: performed separately Risk and Benefits: Scalp blocks have been shown to decreas pain scores for longer postoperatively than local infiltration of the wound, and may decrease opioid consumption, intraoperative blood loss, and risk of patient movement while in pins. Risks are very low. Nerve damage or infection after these procedures is exceedingly rare. Hematoma may occur so palpation of the superficial temporal artery (STA) and occipital artery during these blocks should be used to decrease this complication, and pressure held if hematoma formation begins to appear. In the case of Moya-Moya it may be prudent to avoid blocks in the area of the STA because of its surgical importance. The article below by Suresh and Voronov provides a good overview of these blocks with additional explanations, anatomical figures, and helpful charts which are posted in the Anesthesia area of Neurosurgery OR 2. References: Brydges, G et al. Awake craniotomy: a practice overview. AANA Journal: Feb. 2012; 80(1), 65-66. Kersher, C. et al. Scalp blocks: a useful technique for neurosurgery, dermatology, plastic surgery and pain therapy. Der Anesthetist 2009: 9; 949-960. Suresh, S. and Voronov, P. Head and neck blocks in infants, children, and adolescents. Pediatric Anesthesia, (2012) 22: 81–87.