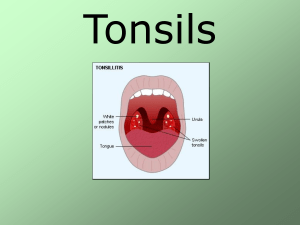
3-Tonsillitis
advertisement

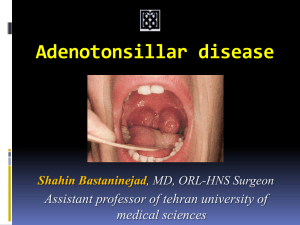
3rd year/Analytical Invest. Dr.Hawraa A.Ali Ad-Dahhan Transmitted Diseases Lecture 4-5 Tonsillitis Tonsillitis, sometimes referred to as pharyngitis,is inflammation of the pharyngeal tonsils that may also extend to the adenoids. The condition can be acute, recurrent, or chronic. The uncomplicated acute form, which often follows an upper respiratory infection, usually lasts 4 to 6 days and affects children between ages 5 and 10. Tonsillitis is considered recurrent if the patient experiences seven episodes in 1 year, five episodes in 2 consecutive years, or three episodes yearly for 3 consecutive years. Chronic tonsillitis is persistent infection of the tonsils. CAUSES Tonsillitis generally results from infection with beta-hemolytic streptococci but can also result from other bacteria or viruses, such as herpesvirus, cytomegalovirus, or adenovirus. COMPLICATIONS Chronic tonsillitis may result in chronic upper airway obstruction, causing sleep apnea or sleep disturbances, failure to thrive, eating or swallowing disorders, and speech abnormalities. otitis media, cardiac valvular disease, abscesses,glomerulonephritis, subacute bacterial endocarditis, and abscessed cervical lymph nodes may also be noted. Scarlet fever, rheumatic fever, and heart disease may also occur, but these conditions are not as common as they were before the widespread use of antibiotics. ASSESSMENT FINDINGS The patient with acute tonsillitis may complain of mild to severe sore throat. In a child who is too young to complain about throat pain, the parents may report that the child has stopped eating. The patient or parents also may report muscle and joint pain, chills, malaise, headache, and pain that is frequently referred to the ears. Fever of 100_ F (37.8_ C) or higher may be present Patients with chronic tonsillitis may report recurrent sore throats and attacks of acute tonsillitis. They may present with purulent drainage in the tonsillar crypts, foul breath, and persistently tender cervical nodes. DIAGNOSTIC TESTS ◗ Throat culture may reveal the infecting organism and indicate appropriate antibiotic therapy. 1 ◗A complete blood count usually reveals leukocytosis. ◗Needle biopsy helps differentiate cellulitis from abscess. TREATMENT Management of acute tonsillitis stresses symptom relief and requires rest, adequate fluid intake, aspirin or acetaminophen and, for bacterial infection, an antibiotic. For infection with group A beta-hemolytic Streptococcus, penicillin is the drug of choice. (Erythromycin or another broad-spectrum antibiotic may be given if the patient is allergic to penicillin.) To prevent complications, antibiotic therapy should continue for 10 days. Patients with chronic tonsillitis or complications may require tonsillectomy—but only after they are free of tonsillar or respiratory tract infections for 3 to 4 weeks. Otitis media Otitis media is inflammation of the middle ear that may be suppurative or secretory, acute or chronic, persistent, or unresponsive. With prompt treatment, the prognosis for acute otitis media is excellent; however, prolonged accumulation of fluid can cause chronic otitis media and perforation of the tympanic membrane. Patient risk factors for otitis media include age, anatomic anomalies, gastroesophageal reflux, the presence of adenoids, and genetic predisposition. Environmental risk factors include upper airway infections or allergies, seasonality (the incidence is higher in fall and winter), day-care center attendance, bottlefeeding, exposure to passive smoking, and use of pacifiers. Common pathogens associated with otitis media include Streptococcus pneumoniae, Haemophilus influenzae,Moraxella catarrhalis, Staphylococcus aureus, group A Streptococcus, and mixed anaerobes. CAUSES Otitis media results from disruption of Eustachian tube patency. In the suppurative form, bacterial infection is usually the cause; other causes include respiratory tract infection, allergic reaction, nasotracheal intubation, or positional changes that allow flora to reflux through the eustachian tube and colonize the middle ear. Chronic suppurative otitis media results from inadequate treatment for acute otitis episodes, infection by resistant bacteria or, rarely, tuberculosis. Obstruction of the eustachian tube causes a buildup of negative pressure and eustachian tube dysfunction. Chronic suppurative otitis media may result from mechanical obstruction (adenoidal tissue overgrowth or tumors), edema (allergic rhinitis or chronic sinus infection). COMPLICATIONS Complications include spontaneous rupture of the tympanic membrane, mastoiditis, 2 meningitis, cholesteatomas (cystlike masses in the middle ear), septicemia, abscesses, vertigo, lymphadenopathy ,facial paralysis, otitis externa, tympanosclerosis, and permanent hearing loss. ASSESSMENT FINDINGS Many patients are asymptomatic. Clinical features of acute suppurative otitis media include severe, deep, throbbing pain; signs of upper respiratory tract infection; mild to very high fever; hearing loss; tinnitus; dizziness; nausea;and vomiting. Bulging of the tympanic membrane with erythema may occur; purulent drainage may be present from tympanic membrane rupture. Pain may stop suddenly when the membrane ruptures. DIAGNOSTIC TESTS ◗ Otoscopic or neuroscopic examination is used to diagnose the disorder. Pneumatoscopy shows decreased tympanic membrane mobility. ◗ Culture and sensitivity testing of exudates is used to identify the causative organism. ◗ Radiographic studies or computed tomography depict mastoid involvement. ◗ Tympanometry and audiometry measure how well the tympanic membrane functions. ◗ Biopsy is used to rule out malignancy and identify tissue. . Treatment for chronic otitis media includes elimination of eustachian tube obstruction and surgery. TREATMENT Antibiotics are given in infants younger than 6 months or in older children if the diagnosis is certain or is severe.Alternatively, the patient may be observed for 48 to 72 hours and given analgesics . Infants with frequent recurrences may be prescribed antibiotic prophylaxis. ALERT Patients with persistent pain or fever should be reexamined within 48 hours. If the child fails to improve, antibiotic therapy should be initiated. If the patient fails to improve with antibiotic therapy, an alternate antibiotic should be initiated 3