Adenotonsillar Disease: Diagnosis & Treatment
advertisement

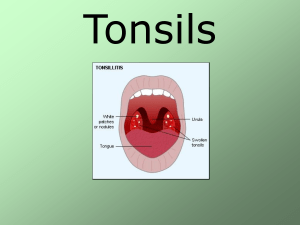
Adenotonsillar disease Shahin Bastaninejad, MD, ORL-HNS Surgeon Assistant professor of tehran university of medical sciences Anatomy Tonsil boundary Plica triangularis Adenoid boundary Posterior aspect of the nasal septum Fossa of Rosenmüller Passavant’s ridge Waldeyer’s Ring Presentation outlines Acute Infections Chronic diseases Obstructive hyperplasia Mass Surgery Acute Infections Acute Adenotonsillitis Etiology 85% of this problem is due to the viral infection (less in children) In bacterial infections there is about 40% antibiotic resistancy (due to beta-lactamaseproducing germs) GABHS is the most important pathogen because of potential sequelae Bacteriology of adenotonsillitis Group A beta-hemolytic is most recognized pathogen This organism is associated with a risk of rheumatic fever and glomerulonephritis Many other organisms are involved : H.influenza S. aureus Streptococcus pneumoniae GABHS More common in 5 to 15 years old children Not seen in less than 3 years Diagnosis Viral pharyngitis symptoms: Coryza Hoarseness Cough Conjunctivitis Centor criteria for GABHS: Hx of fever more than 38 Anterior cervical LAP Pharyngeal or Tonsillar exudate Absence of cough Approach to the Centor scoring 0-1 Abx not needed 2-4 perform Cx Clue : when all 4 scores are present in 44% of the patients there is no GABHS Treatment Plan Delay in treatment up to 9 days can be acceptebale When empiric txy? Lack of Pt .f/u Lack of Lab. access Toxic presentation In some extends when all 4 measures present In parentheses!!! When culture is positive there are two possibilites: True infection Carrier state In this scenario, serological evaluation with ASO(anti-streptolysin O) will be usefull (in true infection it will be more than 3 times than its usual range) Medical Management Penicillin is first line treatment oral medication is preferable (penicillin V) Other choices: Amoxicillin (wide spectrum than Pencillin V) Macrolides Clindamycin Recurrent or unresponsive infections require treatment with beta-lactamase resistant antibiotics such as Clindamycin Augmentin Penicillin plus rifampin (or Erythro + Metro) If no response after 48 hr, re-evaluate patient for the followings: Sequelea Patient’s incompliance Other underlying disease Abx failure Peritonsillar abscess Abscess formation outside tonsillar capsule Signs and symptoms: Fever Sore throat Dysphagia/odynophagia Drooling Trismus Unilateral swelling of soft palate/pharynx with uvula deviation Be aware of ICA Aneurysm! Peritonsillar abscess… Thought to be extension of tonsillitis to involve surrounding tissue with abscess formation Recently described to be an infection of small salivary glands in the supratonsillar fossa called Weber’s glands Would explain superior pole involvement and the usual absence of tonsillar erythema/exudates Candidiasis Infectious Mononucleosis IMN Clinical diagnosis can be made from the characteristic triad of fever, pharyngitis, and lymphadenopathy lasting for 1 to 4 weeks Laboratory tests are needed for confirmation Serologic test results include a normal to moderately elevated white blood cell count, an increased total number of lymphocytes (more than 50%), greater than 10% atypical lymphocytes, and a positive reaction to a "mono spot" test IMN When "mono spot" or heterophile test results are negative, additional laboratory testing may be needed to differentiate EBV infections from a mononucleosis-like illness EBV-Specific Laboratory Tests: IgM and IgG to the viral capsid antigen IgM to the early antigen antibody to EBNA IMN – Test interpretation Primary Infection: Primary EBV infection is indicated if IgM antibody to the viral capsid antigen is present and antibody to EBNA is absent Past Infection: If antibodies to both the viral capsid antigen and EBNA are present, then past infection (from 4 to 6 months to years earlier) is indicated IMN – Test interpretation Reactivation: In the presence of antibodies to EBNA, an elevation of antibodies to early antigen suggests reactivation Chronic EBV Infection: Reliable laboratory evidence for continued active EBV infection is very seldom found in patients who have been ill for more than 4 months Diphtheria Chronic disease Chronic Tonsillitis Chronic sore throat Malodorous breath Presence of tonsilliths Persistent tender cervical lymphadenopathy Lasting at least 3 months Be aware of Anaerobic infections Cryptic tonsils Hyperkeratosis, mycosis leptothrica Tonsilloliths Obstructive Hyperplasia Obstructive Adenoid Hyperplasia Signs and Symptoms Obligate mouth breathing Hyponasal voice Snoring and other signs of sleep disturbance Obstructive Tonsillar Hyperplasia Snoring and other symptoms of sleep disturbance Muffled voice Dysphagia Tonsillar Mass Malignant Neoplasms Most common is lymphoma Non-Hodgkin’s lymphoma Rapid unilateral tonsillar enlargement associated with cervical lymphadenopathy and systemic symptoms Lymphoma SCC Congenital tonsillar masses Teratoma Hemangioma Lymphangioma Cystic hygroma Surgery Tonsillectomy (2010-AAOHNS) Infection indications: Pharyngitis more than 7 / yr in 1 yr More than 5 / yr for 2yrs More than 3 / yr for 3yrs Recurrent infections with modifying factors: Multiple Abx allergy / intolerance PF.ASP.A: periodic fever/aphthous stomatitis and pharyngitis/adenitis History of peritonsillar abscess Tnosillectomy Cont… Persistent foul taste or breath due to chronic tonsillitis not responsive to medical therapy Chronic or recurrent tonsillitis associated with streptococcal carrier state and not responding to betalactamase resistant antibiotics Unilateral tonsil hypertrophy presumed to be neoplastic Adenotonsillectomy ATH and Sleep disordered breathing (SDB) Severity of the SDB depends on adenotonsillar size and/or Craniofacial anatomy and/or neuromuscular tone Ask for comorbid conditions: Growth retardation / poor school performance / enuresis / behavioral problems (ADHD,…) Polysomnography indications (PaO2 less than 85% and/or AHI>5) check PSG in obese patient/down syndrome/craniofacial anomaly &… Infection: Adenoidectomy Purulent adenoiditis Adenoid hypertrophy associated with: Chronic otitis media with effusion Chronic recurrent acute otitis media Chronic otitis media with perforation Otorrhea or chronic tube otorrhea Obstruction (next slide) Other: Suspected neoplasia Adenoid hypertrophy associated with chronic sinusitis Adenoidectomy Cont… Obstruction: Adenoid hypertrophy associated with excessive snoring and chronic mouth-breathing Sleep apnea or sleep disturbances Adenoid hypertrophy associated with: Cor pulmonale Failure to thrive Dysphagia Speech abnormalities Craniofacial growth abnormalities Occlusion abnormalities Speech abnormalities Pre-Op Evaluation of Adenoid Disease Triad of hyponasality, snoring, and mouth breathing Rhinorrhea, nocturnal cough, post nasal drip “Adenoid facies” long face, crowded incisors Pre-Op Evaluation of Adenoid Disease Evaluate palate Symptoms/FH of CP or VPI Bifid uvula CNS or neuromuscular disease Preexisting speech disorder? Pre-Op Evaluation of Adenoid Disease Lateral neck films are useful only when history and physical exam are not in agreement. Accuracy of lateral neck films is dependent on proper positioning and patient cooperation. Any questions !?