8 A, B, C VCH Unit Practice

Nursing Documentation Revisions
Unit-Based Practice Scenario
VUH 8 th Floor Inpatient Medicine
Name: ____________________ Unit: ______________ Date: ___________________
Directions for Completing Practice Scenario
You have completed the LMS Nursing documentation modules and here is your chance to practice. Please use the content provided in the following scenario to practice nursing documentation to become more familiar with the layout and flow. In this scenario, the Nursing Admission History has already been completed and you will begin with an Admission Assessment.
Open HED Train, choose any training patient with last name of ZTRAINHEDUP on your unit to complete documentation.
Practice Scenario: for patient with Age: _26__ & Diagnosis(es): __Cystic Fibrosis_exacerbation____________
Background: 26
year old white male w/ past medical history of Cystic Fibrosis who presents w/ 1 week of worsening SOB, productive cough anorexia, and pleuritic chest pain concerning for subacute CF exacerbation and pneumonia. Treating with tobra, zosyn and linezolid.
1.
Admission Baseline Assessment Data:
PAST MEDICAL HISTORY:
Cystic fibrosis; Malnutrition; Exocrine pancreatic insufficiency; Chronic pain; Depression
Vital Signs: T98.0, RR 22, HR 83, Sp02 96% on 3L/min NC, BP 109/64, weight 50Kg, height 173 cm, BMI 16.8
Pain: rates pleuritic chest pain 7/10 on numeric scale. 1 mg Dilaudid IV given 1 hr ago in ED. Patient has been c/o severe pain for several days.
Neuro: AA&O x4.
Cardiac/Tissue Perfusion: RRR; No murmur, rub, S3, S4; Cap refill <3s; Pulses +2, x4 extremities.
Respiratory: Diminished breath sounds throughout; Course crackles bilateral bases; Cough productive yellow sputum;
Dyspnea on exertion.
GI: Soft; Normoactive BS x4 quads; last BM 2 hrs ago; no N/V. Appetite poor.
Skin: Last Braden 20. Warm, dry; Turgor w/ decreased elasticity; No cuts bruises or lesions.
Renal/UR: Voiding without difficulty; Concentrated urine.
Activity/Musculoskeletal: Activity ad lib.
Fluid/Nutrition: CF diet, boost plus x2 tid cc. Snacks ordered daily. Appetite poor. Ate 50% of breakfast.
Falls Risk/Safety: Emergency equipment at bedside; No signs of abuse; moderate fall risk d/t medications.
Lines: PIV 20 g to R cephalic started in ED. Infusing d51/2ns @ 125mL/hr.
Psychosocial: Patient is withdrawn; distracted by social media on his laptop. Depressed mood; flat affect. Family present and planning to stay overnight. Patient is noncompliant with BG checks as ordered.
Saving: As you save your assessment, denote two (max of 3) Priority Problems by clicking the !! on the review screen before saving and confirming.
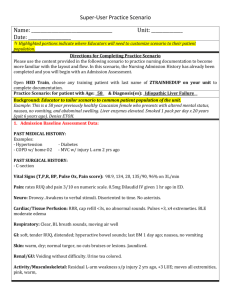
2.
Plan (Hint: PLAN tab)
Select a goal for each of the priority problems. For example:
Pain: Goal 3/10 on numeric scale.
Respiratory: will use incentive spirometer independently and regularly.
Nursing Documentation Revisions
Unit-Based Practice Scenario
3.
Education & Nursing Interventions: Document the following (Hint: Education & Interventions tab)
Care Contact: preferred language: English, learning mode: web-based, Care contact name: Betty White, role: Mother, phone #:
615-936-0332
Education Session: patient and Care contact 1, were given handouts,and verbalized understanding of VUMC general & unit specific education and education re: meds for pain management.
Interventions
Pain control care : medication & positioning
Strict Intake & Output
O2 increased to 4L/min NC
Incentive spirometer
4.
Re-Assessment: You have just performed a focused re-assessment. Document the following:
Re-assessment to denote unchanged except. There would not typically be data in all of these categories.
Please select 1-2 areas for documentation of assessment changes specific to your patient.
Cardiac/Tissue Perfusion: Tachycardic, HR 135.
Notification of the Provider: document that Dr Smith was notified of the HR of 135. Reports that they will come see pt and will enter orders for EKG. Hint: Communication/ Event Note
Respiratory: Breath sounds inspiratory wheeze & rhonchi noted throughout; Dyspnea at rest.
GI: still eating dinner.
5.
End of Shift: It is now the end of your shift. Document the following:
Response to Care/Recommendations (Hint: PLAN tab)
Goal attainment – address goals set at beginning of shift o Pain goal: pain 8/10 numeric scale o Resp goal: used incentive spirometer q2 hours this shift
Question: Since there will be several weeks before all units have transitioned to the new tabs and documentation model, if your unit has gone live but a patient transfer to you from a NON IMPLEMENTED unit, what will be the best way to view the documentation from the sending unit?
(Remember, documentation will not be shared between the old and the new tabs)
Answer:
Upon completion, please sign and return to CSL by 9/14/15 .
Signature: Date: