Workbook for Methotrexate 2014-15 3
advertisement

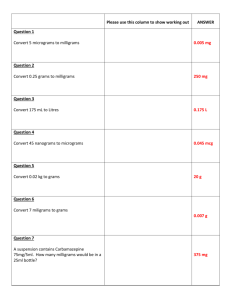
Locally Commissioned Service 2014/15 Provision (Prescribing and Monitoring) of Methotrexate for Camden GP practices Audit Workbook To be completed and returned to Camdenlcs@nhs.net by 17 April 2015. METHOTREXATE Locally Commissioned Service Data Collection Form and AUDIT Practices need to complete the following sections: Date of review: Reviewer: Position of reviewer: Do you have a READ coded register? Yes/No Main READ code used Number of patients prescribed oral Methotrexate in last 12 months Number of patients on the current Methotrexate register Total number of patients on oral Methotrexate that the practice prescribe AND monitor for under the LCS Systems and protocols in place to ensure patients are being monitored for their bloods? Yes/No Prescribers aware of symptoms of toxicity or intolerance Yes/No Practice has updated prescribing software meeting IT criteria in the NPSA Alert Yes/No Document1 1 METHOTREXATE Locally Commissioned Service PRESCRIBING AUDIT Aim of audit: To establish whether the high risk medicine methotrexate is prescribed and monitored appropriately in primary care patients. Audit Criteria Standard 1 Indication for the drug is documented and read coded 100% 2 If a shared care guideline (SCG) is available it is scanned in or alternatively a letter from the hospital clinician with dose, details of monitoring and areas of responsibility etc. is scanned in 80% 3 Monitoring is recorded as per relevant SCG or SPC (SPC Summary of Product Characteristics – Data sheet) 80% 4 Patient aware of risks and benefits of methotrexate, including what sideeffects to watch out for and what to do if they experience any side-effects. NB Confirmation of patient’s understanding should regularly be sought, not just on a one off occasion. 80% 5 Patient and prescriber are aware of the frequency, location and process of conducting blood tests 80% 6 Methotrexate specified dose is prescribed i.e. (in mg and number of tablets and NOT “prn” nor “as directed”) 100% 7 Number of patients prescribed 2.5mg tablets 100% NB: There is a local agreement that only 2.5mg tablets are to be prescribed. To minimise dosing errors 10mg tablets should NOT be prescribed. 8 Repeat prescriptions for methotrexate are retained separately for prescriber review prior to authorising 100% 9 Record of patient held monitoring and information booklet in computerised medical notes 80% 10 Directions on the prescription are in agreement with the current dosage instructions confirmed by the latest hospital letter. 100% 11 Quantity of tablets issued is appropriate and not excessive, consistent with monitoring requirements. 100% NB: Methotrexate The dose should be stated in mg and also the number of 2.5mg tablets required. NB: There is a local agreement that only 2.5mg tablets are to be prescribed. To minimise dosing errors 10mg tablets should NOT be prescribed. All patients should have a methotrexate monitoring and patient information booklet. Document1 2 Audit Process: STEP 1 - Identification of patients Search all patients prescribed methotrexate. STEP 2 - Data collection Print search (computerised practices) for patients on each drug. Photocopy data collection form Complete data collection form using patient records (computerised or manual as appropriate). STEP 3 - Intervention for individual patients Whilst completing the data collection form for each patient identify areas for change, implement changes and document all interventions in patients’ records. Consider the following interventions: Clarify whether prescription for these medicines is by primary care or secondary care. If the latter add note to EMIS re dosing details to ensure interactions are considered when prescribing new medicines. If blood test results to monitor these drugs are unavailable establish a regular process for the patient to attend the practice phlebotomy service or contact the hospital consultant to request blood test results to ensure adherence to the monitoring requirements. Ensure patient is familiar with side-effects and the action to take if experiencing a side effect and the process and importance of monitoring. Add record to EMIS to review this drug at regular intervals. STEP 4 - Analysis Calculate results for the practice. The data collection form has simple yes or no questions and the answers for each patient should be entered into one column. For each of the criteria add up the total number of yes’s divide this by the total number of patients and multiply by 100. Enter the answer into the appropriate summary table column. STEP 5 – Re-audit Re-audit to assess the effect of changes implemented. Develop an action plan for improvement. Document1 3 METHOTREXATE PRESCRIBING AUDIT - DATA COLLECTION FORM Practice: Date of base line audit: Patient Ref no. Date of re-audit: 1 2 3 4 Criteria Total number of patients prescribed methotrexate 1 READ coded indication? 2 SCG or letter from consultant scanned into computer 3 Monitoring recorded as per SCG / SPC 4 Patient aware of side effects & action to take – discussed with patient 5 Patient & Prescriber aware of process for blood tests 6 Specified dose prescribed 7 Prescribed 2.5mg tablets 8 Repeat Rxs retained separately 9 Record of Patient Booklet 10 Directions in agreement with hospital 11 Quantity of tablets appropriate 5 6 7 8 9 10 Enter 1=Yes, 0=No (Photocopy form as necessary – alternatively an electronic version of this form can be used) Comments (Action or follow up required) Document1 4 HIGH RISK MEDICINES AUDIT - SUMMARY TABLE Practice: Audit Criteria Standard 1 Indication for the drug is documented and read coded 100% 2 If a shared care guideline (SCG) is available it is scanned in or alternatively a letter from the hospital clinician with dose, details of monitoring and areas of responsibility is scanned in 80% 3 Monitoring is recorded as per relevant SCG or SPC (SPC Specific Product Characteristics – Data sheet) 80% 4 Patient aware of risks and benefits of methotrexate, including what side-effects to watch out for and what to do if they experience any side-effects. NB Confirmation of patient’s understanding should regularly be sought, not just on a one off occasion. 80% 5 Patient and prescriber are aware of the frequency, location and process of conducting blood tests 80% 6 Methotrexate specified dose is prescribed i.e. (in mg and number of tablets and NOT “prn” nor “as directed”) 100% 7 Number of patients prescribed 2.5mg tablets 100% Practice Baseline % Practice Re-Audit % NB: There is a local agreement that only 2.5mg tablets are to be prescribed. To minimise dosing errors 10mg tablets should NOT be prescribed. 8 Repeat prescriptions for methotrexate are retained separately for prescriber review prior to authorising 100% 9 Record of patient held monitoring and information booklet in computerised medical notes 80% 10 Directions on the prescription are in agreement with the current dosage instructions confirmed by the latest hospital letter. 100% 11 Quantity of tablets issued is appropriate and not excessive, consistent with monitoring requirements. 100% Document1 5