Microsoft Word - 11.5 2015 Initial Evaluation CF
advertisement

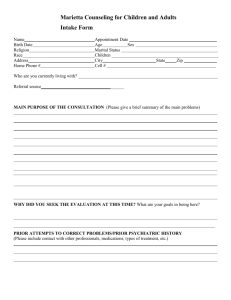
CHILDREN FIRST INITIAL EVALUATION (complete after 1st session with parent) Client: Date: Date of Birth: Gender: Therapist/Evaluator: Race/Ethnicity: Returning Client: Sources of Information: (names and relationship to client ie: parent, teacher, etc.) Presenting Problem: (brief history, precipitating events) Client Strengths, Skills, Interests, Involvement in School Activities: Family History and Functioning: (may include genogram) Cultural Assessment: (age, development, disability, religion, ethnicity(race), sexual orientation, socioeconomic status, indigenous heritage, national heritage, gender identity) EDUCATIONAL INFORMATION: Grade: Name of School: Current Grades/GPA: Attendance Issues: Quality of Relationships with School Staff: (cooperative, withdrawn, defiant, other) Quality of Relationships with Peers at School: (friendly, aggressive, victimized, bullies, other) 08/15 11.5 Identified Learning Problems: IEP: Yes No School Behaviors: (enjoys school, follows rules, inattention, disruptive behaviors, withdrawn, other) Educational and Career Goals: PSYCHOSOCIAL RISK ASSESSMENT OR FACTORS: Circle best response and include additional information in comments section Failure to thrive: Child abuse/sexual abuse/neglect Exposure to Domestic Violence History of out-of-home placement At risk of out-of-home placement Exposure to community violence Victim of community or other violence Unsafe neighborhood Homeless Living in poverty Parental divorce or separation Loss of parent to (circle one): Death Incarceration Deportation Familial substance abuse Serious illness in family Caregiver developmental disability Family history of mental illness Impulsivity/acting out bxs Legal difficulties Sexual acting out Lack of Resources (please list) N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A Current Current Current Current Current Current Current Current Current Current Current Past Past Past Past Past Past Past Past Past Past Past N/A N/A N/A N/A N/A N/A N/A N/A N/A Current Current Current Current Current Current Current Current Current Past Past Past Past Past Past Past Past Past Comments: Current danger to self: High Moderate Low None Current danger to others: High Moderate Low None Current impulsivity: High Moderate Low None PRESENT MENTAL, PHYSICAL, DENTAL HEALTH STATUS (include dates of last physical, dental, etc.): PREVIOUS COUNSELING (include voluntary/involuntary hospitalizations, suicidal behavior, other): 08/15 PRELIMINARY DIAGNOSIS: ICD-10-CM DISORDER (including DSM-5 Specifiers) OTHER CONDITIONS THAT MAY BE A FOCUS OF CLINICAL ATTENTION: CONDITION/PROBLEM: Z Z Z Z Parent/Guardian Signature Therapist Signature (with credentials) Supervisor Signature 08/15