Blood
advertisement

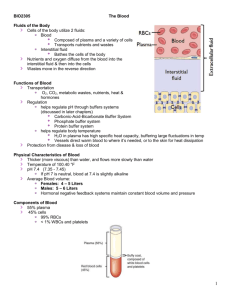
BIO2305 The Blood Fluids of the Body Cells of the body utilize 2 fluids: Blood Composed of plasma and a variety of cells Transports nutrients and wastes Interstitial fluid Bathes the cells of the body Nutrients and oxygen diffuse from the blood into the interstitial fluid & then into the cells Wastes move in the reverse direction Functions of Blood Transportation O2, CO2, metabolic wastes, nutrients, heat & hormones Regulation helps regulate pH through buffers systems (discussed in later chapters) Carbonic-Acid-Bicarbonate Buffer System Phosphate buffer system Protein buffer system helps regulate body temperature H2O in plasma has high specific heat capacity, buffering large fluctuations in temp Vessels direct warm blood to where it’s needed, or to the skin for heat dissipation Protection from disease & loss of blood Physical Characteristics of Blood Thicker (more viscous) than water, and flows more slowly than water Temperature of 100.40 °F pH 7.4 (7.35 - 7.45) If pH 7 is neutral, blood at 7.4 is slightly alkaline Average Blood volume: Females: 4 – 5 Liters Males: 5 – 6 Liters Hormonal negative feedback systems maintain constant blood volume and pressure Components of Blood 55% plasma 45% cells 99% RBCs < 1% WBCs and platelets 1 Hematocrit (Hct) & Hemoglobin (Hb) Hematocrit (Hct) - percentage of blood volume occupied by RBCs volume of red blood cells ÷ total blood volume Normal Hematocrit range: adult female: 38 - 46% (average of 42%) adult male: 40 - 50% (average of 45%) Hemoglobin (Hb) – the protein responsible for transporting oxygen in the blood Normal Hemoglobin range: adult females: 12 – 16 g/1 dL of blood adult males: 13.5 – 18 g/1 dL of blood Anemia - not enough RBCs, hemoglobin Polycythemia - too many RBCs (over 50%) 2 Blood Plasma Over 90% water 7% plasma proteins created in liver confined to bloodstream albumin Blood osmotic pressure Transporter substances globulins Immunoglobulins (antibodies) Defense against foreign proteins fibrinogen Clotting protein precursor 2% other substances electrolytes, nutrients, hormones, gases, waste products Formed Elements of Blood Red blood cells (erythrocytes) Platelets (thrombocytes) White blood cells (leukocytes) Granular leukocytes Neutrophils Eosinophils Basophils Agranular leukocytes Lymphocytes (T cells, B cells, and natural killer cells) Monocytes Normal RBC count: ~ 5 million/µL Males: 5.4 million/µL Female: 4.8 million/µL Platelet count: 150,000-400,000/µL WBC count: 5,000 - 10,000/µL Ratio: 700 RBC’s and 40 Platelets to every 1 WBC. 3 Hematopoiesis: Formation of Blood Cells Most blood cell types need to be continually replaced Blood cells die within hours, days, or weeks Hematopoiesis (or hemopoiesis) – the process of blood cell formation In adults: Occurs only in red marrow of flat bones (pelvis, sternum, ribs, vertebrae, & skull, and in ends of long bones) Hematopoiesis of All Blood Cells All blood cells develop from the same uncommitted stem cells in bone marrow Red Blood Cells or Erythrocytes Contain oxygen-carrying protein hemoglobin that gives blood its red color 1/3 of cell’s weight is hemoglobin Biconcave disk Increased surface area:volume ratio Flexibility for narrow passages No nucleus or other organelles No mitochondrial ATP formation New RBCs enter circulation at 2-3 million/second 4 Hemoglobin Hemoglobin Molecule: >> 4 globular protein subunits >> each containing 1 heme group (red pigment) >> each containing 1 iron ion (Fe+2) >> each capable of binding (reversibly) to 1 oxygen (O2) molecule Hemoglobin carrying capacity: 1 RBC = ~ 280 million Hemoglobins 1 Hemoglobin = 4 Heme Groups 1 Heme Group = 1 Iron atom = 1 O2 molecule Therefore, 1 RBC can hold up to ~1.12 x 109 O2 molecules The iron ion (Fe2+) wiithin a heme group is the site of oxygen binding. The binding sites for CO2 molecules as well as H+ ions are located distal to the central O2 binding site on the globular subunits. At the tissue level, hemoglobin binds to H+ and CO2, which causes a conformational change in the protein and facilitates the release of oxygen. H+ ions bind at various places on the protein, while carbon dioxide binds at the α-amino groups within the α and β protein subunits. Function of Hemoglobin Each hemoglobin molecule can carry four O2 or CO2 molecules Hemoglobin also acts as a buffer and balances pH of blood by transporting H+ ions away from tissues Hemoglobin transports 23% of total CO2 waste from tissue cells to lungs for release Forms of Hb: Oxyhemoglobin: hemoglobin + O2 Deoxyhemoglobin: hemoglobin – O2 Carbaminohemoglobin: hemoglobin + CO2 Normal hemoglobin range Infants have 14 to 20 g/1 dL of blood Adult females have 12 to 16 g/1 dL of blood Adult males have 13.5 to 18g/1 dL of blood 5 Hemoglobin Affinity CO2 vs O2 Deoxyhemoglobin’s affinity for carbon dioxide (CO2) is greater than its affinity for oxygen (O2) Carbon dioxide (CO2) can lower O2-Hb affinity through changes in its partial pressure (pCO2) or pH (carbonic acid reaction) CO vs O2 (Carbon Monoxide Poisoning): Hemoglobin’s affinity for carbon monoxide (CO) is 250 times greater than its affinity for oxygen (O2) CO is colorless, odorless, flammable, and highly toxic CO binds irreversibly to the Fe2+ in hemoglobin. Treatment requires oxygen therapy, or hyperbaric oxygen therapy, depending on severity of poisoning The drop in Hb O2 saturation goes unnoticed for a while because chemoreceptors rely primarily on [CO2] for the “urge to breathe” Erythropoiesis: Production of RBCs Multipotent stem cell differentiates into Proerythroblast Proerythroblast begins producing hemoglobin, becoming erythroblast Erythroblast ejects nucleus, becoming a reticulocyte Reticulocyte escapes from bone marrow, enters blood stream In 1-2 days, reticulocyte ejects remaining organelles, becoming Erythrocyte Factors required for Erythropoiesis: Erythropoietin (EPO) from kidneys Vitamin B12 (cobalamin) Iron (Fe) Negative Feedback Control of Erythropoiesis Hypoxia – inadequate oxygen supply to tissues generalized hypoxia – systemic oxygen deprivation tissue hypoxia – local oxygen deprivation Common Causes: High altitudes decreased atmospheric pressure Anemia RBC or hemoglobin production < RBC destruction Kidney response to hypoxia: Release Erythropoietin (EPO) Speeds up cell division of erythroblasts, and maturation and release of erythrocytes 6 Negative Feedback Control of Erythropoiesis Negative Feedback Control of Erythropoiesis 7 RBC Life Cycle WBC Physiology Less numerous than RBCs 5,000 to 10,000 cells per µL of blood 1 WBC for every 700 RBC Only 2% of total WBC population is in circulating blood at any given time Heavily populate lymph, lymph nodes, skin, lungs, & spleen Requires colony stimulating factor (local bone marrow/WBC hormone) 8 Neutrophil Function Fastest response of all WBC to bacteria and parasites Direct actions against bacteria release lysozymes which destroy/digest bacteria release defensin proteins that act like antibiotics release strong oxidants (bleach-like, strong chemicals ) that destroy bacteria Basophil Function Involved in inflammatory and allergy reactions Leave capillaries (diapedesis) & enter tissues Release heparin, histamine & serotonin heighten the inflammatory response and account for hypersensitivity (allergic) reaction Heparin is a potent anti-coagulant that does not allow clotting within vessels Eosinophil Function Leave capillaries to enter tissue fluid Attack parasitic worms Release histaminase slows down inflammation caused by basophils Phagocytize antibody-antigen complexes Monocyte Function Take longer to get to site of infection, but arrive in larger numbers Become wandering macrophages, once they leave the capillaries Destroy microbes and clean up dead tissue following an infection Lymphocyte Functions B cells destroy bacteria and their toxins turn into plasma cells that produce and release antibodies T cells attack viruses, fungi, transplanted organs, cancer cells Natural killer cells (NKC) attack many different microbes & some tumor cells destroy foreign invaders by direct attack Differential WBC Count Detection of deviations in normal ranges of circulating WBCs indicates immune response to infection, poisoning, leukemia, chemotherapy, parasites, or allergens Normal WBC counts: Neutrophils: 60-70% (up if bacterial infection) Lymphocyte: 20-25% (up if viral infection) Monocytes: 3 - 8 % (up if fungal/viral infection) Eosinophil: 2 - 4 % (up if parasite or allergy reaction) Basophil: < 1% (up if allergy reaction) 9 Thrombocytes (Platelets) Disc-shape cell fragment with no nucleus, Normal platelet count is 150,000-400,000/µL of blood. Platelets form in bone marrow: Myeloid stem cells eventually become megakaryocytes whose cell fragments form platelets Short life span - 5 to 9 days in bloodstream Aged platelets removed by fixed macrophages in liver and spleen. Platelets release ADP and other chemicals needed for platelet plug formation Hemostasis Hemostasis - stoppage of bleeding in a quick & localized fashion when blood vessels are damaged Prevents hemorrhage (loss of a large amount of blood) Three major steps of Hemostasis: 1. Vascular spasm 2. Platelet Plug Formation Aggregation and adhesion of platelets 3. Blood Clotting Fibrin threads entangle platelets and RBCs to form blood clot Vascular Spasm Damage to blood vessel stimulates pain receptors Reflex contraction of smooth muscle of small blood vessels Can reduce blood loss for several hours, allowing other mechanisms to take over Effective only for small blood vessels or arterioles, not major arteries 10 Platelet plug formation Platelet Plug Formation steps: 1. Platelet Adhesion Platelets stick to exposed collagen of vessel 2. Platelet Release Reaction Platelets extend projections Platelets release Thromboxane A2, Serotonin & ADP activating other platelets 3. Platelet Aggregation Platelets stick together forming a platelet plug 1) Platelet Adhesion Platelets stick to exposed collagen underlying damaged endothelial cells in vessel wall 2) Platelet Release Reaction Platelets activated by adhesion Extend projections to make contact with each other Release Thromboxane A2, Serotonin & ADP activating other platelets Serotonin & Thromboxane A2 are vasoconstrictors decreasing blood flow through the injured vessel. ADP causes stickiness 11 3) Platelet Aggregation Activated platelets stick together and activate new platelets to form a mass called a platelet plug Plug reinforced by fibrin threads formed during clotting process Platelet plug formation Blood Clotting Blood drawn from the body thickens into a gel if not mixed with anticoagulant Blood separates into liquid (serum) and a clot of insoluble fibers (fibrin) in which the blood cells are trapped Substances required for clotting: Ca+2 Clotting Factors (enzymes made by liver) Substances released by platelets or damaged tissues Clotting is a cascade of reactions Each clotting factor activates the next, in a specific sequence, resulting in the formation of fibrin threads 12 Coagulation A set of reactions in which blood is transformed from a liquid to a gel Coagulation follows intrinsic and extrinsic pathways Common Pathway: The final three steps Prothrombinase (Prothrombin activator) is formed from Factor X Prothrombinase converts Prothrombin into Thrombin Thrombin catalyzes polymerization of Fibrinogen into a Fibrin mesh Two Pathways to Prothrombin Activator May be initiated by either the intrinsic or extrinsic pathway Triggered by tissue-damaging events Involves a series of procoagulants Each pathway cascades toward Factor X Once Factor X has been activated, it complexes with Ca+2 ions, PF3, and Factor V to form Prothrombin activator (Prothrominase) 13 Coagulation Phase of Hemostasis Coagulation Pathway Prothrombinase & Ca+2 catalyze the conversion of Prothrombin to Thrombin Thrombin & Ca+2 catalyze the polymerization of Fibrinogen into Fibrin Insoluble fibrin strands form the structural basis of a clot Fibrin causes RBCs and Platelets to become a gellike plug Thrombin & Ca+2 also activate Factor XIII (F13) that: Cross-links fibrin mesh Strengthens and stabilizes the clot 14 Coagulation Pathway Clot Dissolution Inactive plasminogen becomes plasmin, a fibrinolytic enzyme Plasmin dissolves small clots at site of a completed repair Clot formation remains localized blood flow disperses clotting factors Basophils release heparin (anticoagulant), preventing inappropriate clots Intravascular Clotting Thrombosis Clot (thrombus) formed in an unbroken blood vessel Attached to rough inner lining of blood vessel Blood flows too slowly (stasis) allowing clotting factors to build up locally & cause coagulation May dissolve spontaneously or dislodge & travel Embolus – free floating clot in the blood Low dose aspirin blocks synthesis of thromboxane A2 & reduces inappropriate clot formation, Helps to prevent strokes, myocardial infarctions 15 Blood Types Agglutinogens – surface antigens on cells Presence or absence of surface antigens determines Blood Type Composed of glycoproteins & glycolipids Antigens: A, B and Rh (D) Agglutinins – antibodies in the plasma Cross-reactions occur when antigens meet antibodies ABO Blood Groups Based on 2 glycolipid isoantigens called A and B found on the surface of RBCs display only antigen A -- Blood Type A display only antigen B -- Blood Type B display both antigens A & B -- Blood Type AB display neither antigen -- Blood Type O Plasma contains isoantibodies or agglutinins to the A or B antigens not found in your blood Anti-A antibody reacts with antigen A Anti-B antibody reacts with antigen B 16 Blood Type Testing RH blood groups Antigen was discovered in blood of Rhesus monkey People with Rh isoantigens on RBC surface are Rh+ Normal plasma contains no anti-Rh antibodies Antibodies develop only in Rh- blood type & only after exposure to the antigen Transfusion reaction upon 2nd exposure to the antigen results in hemolysis of the Rh+ RBCs HDN Rh negative mom and Rh+ fetus will have mixing of blood at birth Mom's body creates Rh antibodies unless she receives a RhoGam shot soon after first delivery, miscarriage or abortion In 2nd child, Hemolytic Disease of the Newborn may develop causing hemolysis of the fetal RBCs 17 Universal Donors and Recipients People with type AB+ blood called “universal recipients” since have no antibodies in plasma AB+ blood cells contain all three surface antigens (A, B & D). Hence, their immune system will not make antibodies to those markers. Only true if cross match the blood for other antigens People with type O- blood cell called “universal donors” since they have no antigens on their cells O- RBCs have no surface antigens. RBCs are “naked” and remain undetected by recipient immune systems. Anemia = Not Enough RBCs Symptoms oxygen-carrying capacity of blood is reduced fatigue, cold intolerance & paleness Types of anemia: iron-deficiency =lack of absorption or loss of iron pernicious = lack of intrinsic factor for B12 absorption hemorrhagic = loss of RBCs due to bleeding (ulcer) hemolytic = defects in cell membranes cause rupture thalassemia = hereditary deficiency of hemoglobin aplastic = destruction of bone marrow (radiation/toxins) Sickle-cell Anemia (SCA) Genetic defect in hemoglobin molecule (Hb-S) that changes 2 amino acids at low very O2 levels, RBC is deformed by changes in hemoglobin molecule within the RBC sickle-shaped cells rupture easily = causing anemia & clots Found among populations in malaria belt Mediterranean Europe, sub-Saharan Africa & Asia Person with only one sickle cell gene increased resistance to malaria because RBC membranes leak K+ & lowered levels of K+ kill the parasite infecting the red blood cells 18 Hemophilia Hemophilia - inherited deficiency of genes for clotting factors synthesis bleeding spontaneously or after minor trauma subcutaneous & intramuscular hemorrhaging nosebleeds, blood in urine, articular bleeding & pain Types: Hemophilia A lacks factor VIII (males only) most common Hemophilia B lacks factor IX (males only) Hemophilia C (males & females) less severe because alternate clotting activator exists Treatment is transfusions of fresh plasma or concentrates of the missing clotting factor Leukemia Acute leukemia uncontrolled production of immature leukocytes crowding out of normal red bone marrow cells by production of immature WBC prevents production of RBC & platelets Chronic leukemia accumulation of mature WBC in bloodstream because they do not die classified by type of WBC that is predominant---monocytic, lymphocytic. 19