Handout – Hypertensive Emergencies Hypertensive Emergency BP
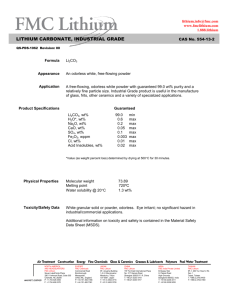
advertisement

Handout – Hypertensive Emergencies Hypertensive BP goals Emergency Hypertensive Encephalopathy Medical Therapy The Evidence Clinical Pearls Hypertension w/ CHF,MI Intracranial Hemorrhage Ischemic Stroke Aortic Dissection Pre-eclampsia Eclampsia Case 1: You are at the PLC seeing a patient in WRC. Mrs. Dhaliwal is a 53 yo female who speaks limited English, and is in with her daughter. She had been seen at FMC by a colleague 3 days prior, and referred to urgent neurology clinic. She has been experiencing headache and numbness to her right arm intermittently for the past week, and has had episodes of dizziness and poor coordination. She has returned today feeling unwell. You are waiting to receive the chart from FMC with the details of this visit. You scan her vitals and her BP is 170/105. Her neurological and cardiovascular examination is normal. Her ECG is unremarkable. 1) What do you want to do about this blood pressure? 1 2) What investigations do you want to order? (EO dysfunction) You order your tests and go and see another patient. The nurse pages you back to RAZ, who tells you her blood pressure is even higher, at 190/115. She is complaining of a worsening headache, and her daughter tells you she seems to be a bit confused. You re-examine her and find new right-sided upper extremity weakness and some poor coordination in her right hand. You search for the panoptic for fundoscopy, but it has taken a walk-about and you can’t find it. You also arrange a CT head. 3) What is her diagnosis? 4) How do you want to treat her blood pressure? What 2 agents can you use in this case, and what is your BP / MAP goal? 5) What are 2 contra-indications to using sodium nitroprusside? Case 2: It’s a Friday night at PLC, and it has been slow. You are wishing you had taken the shift at FMC, you hear there’s been 2 stabbings and a thoracotomy over there! Damn. After seeing your fifth WRC patient, you sign up for a patient in B2. Julius is a 55 yo male from Kenya. He has been feeling unwell for several days, with some shortness of breath and uncomfortable sensation in his chest. You are concerned as you eyeball him. He is in moderate respiratory distress. You quickly examine him and find bilateral crackles, an elevated JVP and mild pitting edema. His BP on the monitor reads 235/130, HR120, SaO2 99% 8L NP. Your ECG and CXR are below, trops are pending. 2 1) How do you calculate the mean arterial pressure? What is Julius’s MAP? 2) Are you worried about his vital signs in this clinical context, why? 3) Your tnt comes in and is 0.90. How are you going to manage this patient? What are your BP goals and what is your first line agent? 4) Would you beta block this patient? 3 Case 3: You decide to do an elective in Cranbrook. After all the great trauma and interesting medical cases you see coming from there, you figure it’s the place to be. Your first patient is a 59 yo long haul trucker named Dave. On the way to the bathroom this morning Dave had sudden onset of weakness his left arm and leg and a facial droop. He called 911 and is now sitting in your emergency department 30min after the onset of his symptoms. Upon his arrival to the ER, he is taken urgently to the CT scanner. CTA shows a right MCA occlusion. You decide he needs tpa then transfer to FMC. Dave is awake, alert, and oriented. His VS are as follows: HR 90 BP225/115 RR16 SaO2 99% NP 1. What do you think about Dave’s BP? 2. What is your BP goal? 3. As your nurse is drawing up the tpa, you learn that Dave had a trauma 1 month ago in a dirt bike accident where he sustained a small traumatic subdural hematoma, resolved on CT today. Does this change the management of his BP? 4. What 3 agents can you use to treat his blood pressure in either scenario, and which is your first line therapy? Dave does not get TPa and is transferred to FMC. He recovers some of his function, but has persistent disability. He goes back to Cranbrook for ongoing stroke rehab. Case 4: You are working at FMC when Linda, a 75 yo woman with a history of hypertension presents with headache, confusion, and dysphasia. Her husband called 911 and she is brought to the ED. Before you have a chance to see her, the stroke team rushes her off to the scanner, and her head CT is below. 4 When she returns from CT she has a decreased level of consciousness, with a GCS 8 so you intubate her. 10 minutes after intubation and despite being on propofol her BP is still 230/110. 1) Are you going to lower her BP? If so, what are your BP goals? 2) What agent are you going to use? What agent should you avoid and why? 3) If anything, what worries you the most about lowering the BP? Case 5: You are working at FMC. Your next patient is in bed 15. She is a 71yo F who felt weak and dizzy and had a syncopal episode at home, associated with some chest and back pain. Initially with EMS there had been a question of left sided weakness, which has now resolved. Her past medical Hx is significant for hypertension and dyslipidemia. You are concerned about the possibility of aortic dissection given the story, and send her for CT angio of chest and neck. Her CT is below. When she gets back from CT the BP in her left arm remains persistently elevated at 160/100, but the BP on the right is 90/50. 1) What do you see on CT? Who you gonna call? 5 2) You have called cardiac surgery and they are on their way in. They ask you to manage the BP. Are you concerned about the BP in this scenario? Which BP reading should you use to guide therapy? 3) What agent will you use first and why? What are your BP goals? 4) You treat her BP and it is now 130/90, HR 60. What’s your plan now doctor? 5) You treat her BP to a goal you are happy with, and she now has persistent left sided weakness. You repeat a CT scan of here head, which shows a right sided cerebral infarct. What do you want to do with her BP management now? Case 6: You are a disgruntled resident, a bit fed up with life half way through residency. As a favor to yourself and your loved ones, you decide to leave town for an elective in Revelstoke, BC. You are so stoked for all the skiing you are going to do. It’s your first night on call for the emergency department, and you are called in to see a young woman who is unwell. Chalrie is a 25 yo female who presents with nausea, vomiting, and is achy all over, especially her head. The nurse tells you she has gastro. You see she is holding a cute little baby in her arms, and Charlie tells you she is 3 weeks old. 6 You glance at the chart before examining her. Her BP is 160/105. You think that’s a little odd. 1. What else do you want to know on history and physical exam? 2. What investigations do you wan to order? Your lab technician is sleeping at home, but you can get a urine right now. 3. What is your diagnosis? You call your preceptor for help, but to your dismay he has taken off to Rogers pass for the night; they figured you are a resident form the city, you got it covered. 4. How are you going to manage Charlie? If any, what are your BP goals, and if you treat her BP what 2 agents will you use? 5. Will you give Charlie magnesium sulfate? 7