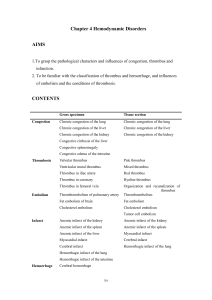
Practical classes
advertisement

I. INTRODUCTION. NECROSIS, GANGRENE. 1. Recent myocardial infarction: An example of coagulative necrosis. Judging from the lack of staining of the nuclei of cardiac muscle cells (with increased eosinophilia of the cytoplasm) and the diffuse neutrophilic infiltrate in the interstitium, it has to be more than 24 hours old. Subendocardial layers survive (supplied through diffusion through the endocardium). 2. Older myocardial infarction: This infarction may be 2-3 weeks old. Necrotic tissue, now completely devoid of nuclei, is being slowly resorbed by macrophages (see residual granules of lipofuscin from necrotic muscle cells in their lysosomes) and replaced by graulation and by fibrous tissue. 3. Postinfarction scar of the myocardium: Necrotic muscle has been completely resorbed and the granulation tissue has been replaced by connective tissue scar. Note residual muscle fibers included in the scar tissue (possible source of arrhythmia). 4. Renal infarct: Coagulative necrosis of the kidney usually secondary to arterial occlusion, caused by a thrombotic embolus. Note preservation of the basic architercture of the necrotic renal parenchyma. Necrotic area is usually surrounded by a zone of leukocytic infiltration, haemorrhage and a zone of selective necrosi of epithelium of proximal tubules, which is most sensitive to hypoxia. In an older infarct, central necrosis is surrounded by a layer of fibrosing nonspecific granulation tissue. 5. Caseous tbc lymphadenitis: Central necrosis in the lymph node is surrounded by a rim of the so-called epithelioid cells and large multinucleated giant cells of the Langhans type. Note the cheomatin dust from the destroyed nuclei in some areas of necrosis. 6. Cerebral infarct (encephalomalacia): Ischemic colliquative necrosis, vital reaction – activated microglia (enlarged cells with vacuolated cytoplasm) so called “granular cells” (rich in lipids), healing by formation of a pseudocyst. Causes: thrombosis, embolism. Hemorrhagic infarct (usually caused by embolism, small, cortical) through reflux of blood into the necrotic focus – red encephalomalacia. Diagnostic features – leucostasis, diapedesis of leukocytes and erythrocytes, activated microglia disintegration of necrotic tissue. 7. Lung tromboembolism and haemorrhagic infarct: Pyramidal shape, note a branch of pulmonary artery occluded by trombembolus. Develops only in congested lung. 8. Chronic peptic ulcer of stomach: Chronic peptic ulcer, note three layers at the base – necrotic debris with leukocytes, layer of fibrinoid necrosis, layer of non-specific granulation tissue, then peripheral fibrosis. Thickened walls of adjacent arteries, hyperthrophy of nervous fibres and fibrosis in the basal part of wall are signs of chronicity. II. INTRODUCTION. ATROPHY, DYSTROPHY. 1. Atrophy of the heart muscle: Simple atrophy – cardiac muscle cells become smaller but their number does not decrease. Sudan B Black stain shows accumulation of the lipid pigment lipofuscin in the perinuclear lysosomes (“wear and tear pigment”), PAS-positive, insoluble pigment resulting from breakdown of cellular membranes. Elderly patients, chronic wasting diseases. 2. Atrophy of the hepatis: 3. Follicular amyloidosis of liver: AA amyloid, Congo-positive, apple green fluorescence in polarized light. Deposition mostly in the white pulp (in follicles). 4. Amyloid nephropathy: Deposition of amyloid in the walls of arteries and arterioles, less in the glomeruli and under the tubular epithelium. Both in the AA and AL amyloidosis, morphologically indistinguishable. 5. Fatty change of the liver: Intracellular accumulation of neutral triglycerides in large vacuoles in the liver cells. Various causes: hypoxia, toxic effects (mushroom poisoning, carbon tetrachloride), starvation etc. 6. Atherosclerosis: Principal morphological envents: fatty streaks, fibrous plaques, atheromas, ulceration, dystrophic calcification. Mostly intimal involvement. The section shows popliteal artery with a large atheromatous plaque. The lumen is partly filled with red thrombus (amputation spcimen, gangrene of the leg caused by arterial obstuction). 7. Fatty infiltration of the heart muscle: Fat cells dispersed in the myocardial interstitium. In obese patients, physiologically in the anterior wall of the right ventricle. No clinical significance. Do not confuse with fatty degeneration (see below). 8. Renal cell carcinoma (tumor of Grawitz): Assesment of malignancy is unreliable on morphological grounds, since malignant tumours may appear differentiated and encepsulated. Small tumours (under 2cm in diameter) considered benign (clear cell adenoma). Vascular, sometimes cystic, consisting mostly of celar cells containing glycogen. Sometimes with oxyphilic cells, sarcomatoid variant. III. INTRODUCTION. CRYSTALS, PIGMENTATION. 1. Haemosiderosis and haemochromatosis of the liver: The section of the liver tissue shows micronodular cirrhosis and severe deposition of the coarsely granular greensh-brown haemosiderin mostly in the lever cells. In some areas pigmentation can be located to lysosomes on the biliary pole of hepatocytes. There is no pigmentation of Kupffer cells and of the macrophages in the fibrous septa, which show proliferation of bile ducts and mononuclear infiltrate. Haemosiderosis – from excessive destruction of erythrocytes in the RES (e.g.after multiple blood transfudions). Haemochromatosis – from excessive absortion of iron in the intestine. 2. Chronic pulmonary congestion: Mostly in chronic insufficiency of the left ventricle and left atrium. Accumulation of macrophages with haemosiderin in the cytoplasm (blue in the Pearls reaction) - brown induration. 3. Biliary cirrhosis: This lesion is often called biliary fibrosis (there is no nodular transformation of the liver tissue), it appears with severe long-lasting intrahepatic bile stasis. Bile plugs in biliary capillaries between the hepatocytes in liver cell cords, bile stasis in interlobular bile ducts, formation of bile lakes. Staining of bilirubin with the Fouchet's reagent (oxidation to dark green biliverdin – sections bleache out, the staining is not permanent). 4. Biliary nephrosis: Secondary to severe obstructive jaundice (conjugated bilirubin excreted in the urine). Look for pigmented casts in the renal tubules, pigmentation of epithelium of the proximal tubules. 5. Intradermal naevocellular naevus: Clinically small, variably pigmeted, slightly elevated lesion in the skin. Histological types: junctional (with nests of naevus cells in the dermo-epidermal junction. Compound naevus – with more pronouced dermal component. Dermal naevus – no junctional activity, naevus cells are only in the dermis. 6. Malignant melanoma: Increasing in frequency, relation to sunlight. Often developing on the basis of a naevocellular naevus. Variable histological composition, differences in amount of melanin. In nonpigmented variants, Fontana's silver stain for melanin and immunohistology (S100 protein, HMB45 antibody) help in establishing correct diagnosis. Superficial spreading, nodular type. Prognostic assessment according to the depth of infiltation on the dermis (Clark, Breslow grading). 7. Antracosis of the lungs - Chronic bronchitis (hypertrophic type) with emphysema (COPD), exacerbating: Lungs have emphysematous configuration with perivasal and peribronchial antrakosis. The bronchi are lined by hypertrophic mucosa with an increase in goblet cells. Bronchial walls are oedematous, thickened by hyperplastic and hypertrophic mucus-secreting glands, increase amounts of smooth muscle and capillaries. Basement membranes are also thickened. An increase in chronic inflammatory infiltration has been documented (lymphocytes, plasma cells, eosinophils). In airways there is excess mucus with small amount of polymorphonuclear leukocytes. 8. Antracosis of lymph node: Many macrophages filled with black pigment in the area of lymphatics (periarterial, peribronchial location), intraalveolar pigmented macrophages. 9. Silicosis of the lungs: Coniofibrosis with three stages: 1-stigmatization with SiO2 crystals in similar location as antracotic pigment. 2-formation of silicotic nodules, 3-massive fibrosis. Silica crystals can be observed as fine needles in polarized light. IV. INTRODUCTION. CIRCULATORY DISTURBANCES. PART I. 1. Hypertrophy of the myocardium: Increased size of cardiac muscle cells, enlarged rectangular nuclei or binucleated cells, ultrastructure generally preserved. In severe hypertrophy widening of the interstitium. 2. Chronic congestion of the liver: Most pronounced in the lobular centers, sometimes accompanied by centrilobular steatosis and zonal fibrosis. 3. Chronic pulmonary congestion: Mostly in the patients with chronic insufficiency of the left ventricle. Accumulation of the macrophages with haemosiderin in the cytoplasm (blue in the Pearls reaction) - brown induration. 4. Red (stagnation) thrombus: Most often in veins, clotted blood with all its constituents, red colour from the presence of numerous red blood cells. 5. Mixed (stratified) thrombus: Layers of fibrin with blood platelets alternating with layers of whole clotted blood. Note old, mostly resorbed myocardial infarction with formation of an aneurysm filled with the thrombus (effect of slow and turbulent flow of blood). 6. Organising thrombus: Cross section through popliteal vessels (Weigert's elastica stain). The artery shows signs of atherosclerosis, the vein is blocked by a red (stagnation) thrombus with signs of organization (ingrowth of fibroblasts, capillaries). 7. Organised thrombus: The thrombus was replaced by an immature granulation tissue, rich in newly formed capillaries, fibroblasts, collagen and reduced inflammatory infiltrate. 8. Recanalised thrombus: The fusion of capillaries in the granulation tissue during the process of organisation. Anastomosis of the vascular lumina proximal and distal to the occluded segment. Functionally insufficient, often complicated by re-thrombosis. Popliteal vein affected, note the normal structure of popliteal artery. Weigert's elastica stain.