Reading Assignment 1 Odds
advertisement

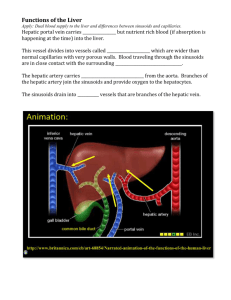
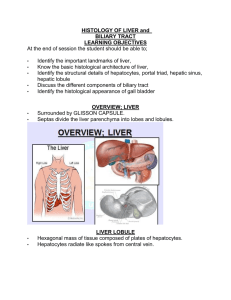
Reading Assignment 1 Odds Short Answer and Discussion 1) Briefly explain what occurs in the liver when fibrosis progresses to cirrhosis. What effect does this have on liver function? Hepatic fibrosis (scaring) occurs in response to chronic liver injury and is characterized by the accumulation of excessive amounts of fibrous tissue, specifically fibrilforming collagens type I and III, and a decrease in normal plasma membrane collagen type IV. Fibrosis can develop around central veins and portal tracts or within the space of Disse. The excessive extracellular matrix protein deposition and the loss of sinusoidal endothelial cell fenestrae and of hepatocyte microvilli limit exhange of nutrients and waste material between hepatocytes and sinusoidal blood.With continuing collagen deposition, the architecture of the liver is disrupted by interconnecting fibrous scars. When the fibrous scars subdivide the remaining liver mass into nodules of regenerating hepatocytes, fibrosis has progressed to cirrhosis and the liver has limited residual capacity to perform its essential functions. Central to the development of fibrosis is the activation of hepatic stellate cells (HSC) (Fig. 13-2), which are the main cell type producing extracellular matrix proteins. Products formed during liver cell injury initiate HSC activation. Activating signals can be reactive oxygen species and lipid peroxidation products generated in injured hepatocytes. In addition, Kupffer cells can release reactive oxygen and proinflammatory cytokines during the phagocytosis of cell debris or apoptotic bodies thereby recruiting more inflammatory cells and enhancing the injury and oxidant stress. 3) Explain the source of bile and the functions of bile once it is produced. *Produced by hepatocytes in the liver and aids in digestion of lipids in the small intestine; protects small intestines from oxidative insult; excretion of endogenous compounds and xenobiotics. Bile is a yellow fluid containing bile acids, glutathione, phospholipids, cholesterol, bilirubin and other organic anions, proteins, metals, ions, and xenobiotics. Formation of this fluid is a specialized function of the liver. Hepatocytes begin the process of bile formation by transporting bile acids, glutathione, and other osmolytically active compounds including xenobiotics and their metabolites into the canalicular lumen. These molecules are the major driving force for the passive movement of water and electrolytes across the tight junctions and the hepatocyte epithelium. The canalicular lumen is a space formed by specialized regions of the plasma membrane between adjacent hepatocytes. The canaliculi are separated from the intercellular space between hepatocytes by tight junctions, which form a barrier permeable only to water, electrolytes, and to some degree to small organic cations. Under physiological conditions, tight junctions are impermeable to organic anions allowing the high concentrations of bile acids, glutathione, bilirubin-diglucuronide, and other organic anions in bile. The structure of the biliary tract is analogous to the roots and trunk of a tree, where the tips of the roots equate to the canalicular lumens. Canaliculi form channels between hepatocytes that connect to a series of larger and larger channels or ducts within the liver. The large extrahepatic bile ducts merge into the common bile duct. Bile can be stored and concentrated in the gallbladder before its release into the duodenum. Functions: Adequate bile formation is essential for uptake of lipid nutrients from the small intestine, for protection of the small intestine from oxidative insults, and for excretion of endogenous and xenobiotic compounds. ***MORE DETAILS ON P 559-562 (NOT SURE HOW DETAILED THIS IS SUPPOSED TO BE) 5) How is fibrosis formed in the liver and what is the primary cause of hepatic fibrosis/cirrhosis in humans worldwide? Hepatic fibrosis (scaring) occurs in response to chronic liver injury and is characterized by the accumulation of excessive amounts of fibrous tissue, specifically fibrilforming collagens type I and III, and a decrease in normal plasma membrane collagen type IV. Fibrosis can develop around central veins and portal tracts or within the space of Disse. The excessive extracellular matrix protein deposition and the loss of sinusoidal endothelial cell fenestrae and of hepatocyte microvilli limit exhange of nutrients and waste material between hepatocytes and sinusoidal blood.With continuing collagen deposition, the architecture of the liver is disrupted by interconnecting fibrous scars. When the fibrous scars subdivide the remaining liver mass into nodules of regenerating hepatocytes, fibrosis has progressed to cirrhosis and the liver has limited residual capacity to perform its essential functions. The primary cause of hepatic fibrosis/cirrhosis in humans worldwide is viral hepatitis. 7) Name the two types of nonciliated cells formed in the proximal airways of humans & describe each. 1. Mucous cells produce respiratory tract mucus, a family of high-molecular-weight glycoproteins with a sugar content of 80% or more. They coat the epithelium with a viscoelastic sticky protective layer that traps pollutants and cell debris. 2. Serous cells produce a fluid in which mucus may be dissolved, or upon which a mucus layer may be floated. The action of the respiratory tract cilia continuously drives the mucus layer toward the pharynx, where it is removed from the respiratory system by swallowing or expectoration. The mucus layer is also thought to have antioxidant, acid-neutralizing, and free radical scavenging functions that protect the epithelial cells 9) Describe deposition of particles. Include descriptions of interception, impaction, sedimentation, and diffusion. 1. Interception occurs when the trajectory of a particle brings it near enough to a surface so that an edge of the particle contacts the airway surface. Interception is important for the deposition of fibers. Whereas fiber diameter determines the probability of deposition by impaction and sedimentation, interception is dependent on fiber length. Thus, a fiber with a diameter of 1 μm and a length of 200 μm will be deposited in the bronchial tree primarily by interception rather than impaction. 2. Impaction - As a result of inertia, particles suspended in air tend to continue to travel along their original path. In an airstream that is not straight, such as at an airway bifurcation, a particle may be impacted on the surface. At relatively symmetrical bifurcations, which typically occur in the human lung, the deposition rate is likely to be high for particles that move in the center of the airway. In the average adult, most particles larger than 10 μmin aerodynamic diameter are deposited in the nose or oral pharynx and cannot penetrate to tissues distal to the larynx. Very fine particles (0.01 μm and smaller) are also trapped relatively efficiently in the upper airways by diffusion. Particles that penetrate beyond the upper airways are available to be deposited in the bronchial region and the deeplying airways. Therefore, the alveolar region has significant deposition efficiencies for particles smaller than 5 μm and larger than 0.01 μm. 3. Sedimentation- brings about deposition in the smaller bronchi, the bronchioles, and the alveolar spaces, where the airways are small and the velocity of airflow is low. As a particle moves through air, buoyancy and the resistance of air act on the particle in an upward direction while gravitational force acts on the particle in a downward direction. Eventually, the gravitational force equilibrates with the sum of the buoyancy and the air resistance, and the particle continues to settle with a constant velocity known as the terminal settling velocity. Sedimentation is not a significant route of particle deposition when the aerodynamic diameter is below 0.5 μm. 4.Diffusion - is an important factor in the deposition of submicrometer particles. A random motion is imparted to these particles by the impact of gas molecules. This Brownian motion increases with decreasing particle size, so diffusion is an important deposition mechanism in the nose and in other airways and alveoli for particles smaller than about 0.5 μm. * An important factor in particle deposition is the pattern of breathing. During quiet breathing, in which the TV is only two to three times the volume of the anatomic dead space (i.e, the volume of the conducting airways where gas exchange does not occur), a large proportion of the inhaled particles may be exhaled. During exercise, when larger volumes are inhaled at higher velocities, impaction in the large airways and sedimentation and diffusion in the smaller airways and alveoli increase. Breath holding also increases deposition from sedimentation and diffusion. Factors that modify the diameter of the conducting airways can alter particle deposition. In patients with chronic bronchitis, the mucous layer is greatly thickened and extended peripherally and may partially block the airways in some areas. Jets formed by air flowing through such partially occluded airways have the potential to increase the deposition of particles by impaction and diffusion in the small airways. Irritant materials that produce bronchoconstriction tend to increase the tracheobronchial deposition of particles. Cigarette smoking has been shown experimentally to produce such an effect. 11) How does the formation of bile help protect the small intestine from oxidative stress? Bilirubin and biliverdin are major constituents of bile. They have the same antioxidant properties within the gut as they do in any cell they are being produced in. 13) What is the most common site of toxicant-induced renal injury? The proximal tubule is the most common site of toxicant-induced renal injury. The reasons for this relate in part to the selective accumulation of xenobiotics into this segment of the nephron. For example, in contrast to the distal tubule, which is characterized by a relatively tight epithelium with high electrical resistance, the proximal tubule has a leaky epithelium, favoring the flux of compounds into proximal tubular cells. More importantly, tubular transport of organic anions and cations, low-molecular-weight proteins and peptides, GSH conjugates, and heavy metals is localized primarily if not exclusively to the proximal tubule. Thus, transport of these molecules will be greater in the proximal tubule than in other segments, resulting in proximal tubular accumulation and toxicity. 15) Why must asbestos fibers be less than 0.5 um in diameter to cause mesothelioma? For the development of mesothelioma, fiber diameter must be less than 0.5 μm, because thinner fibers may be translocated from their site of deposition via the lymphatics to other organs, including the pleural surface. The hazards associated with asbestos exposure depend on fiber length. Fibers 2μmin length may produce asbestosis; mesothelioma is associated with fibers 5μmlong, and lung cancer with fibers larger than 10 μm. Fiber diameter is another critical feature. Fibers with diameters larger than approximately 3 μm do not readily penetrate into the peripheral lung. Fill-in-the-blank, Multiple Choice, etc: 1) The __________LIVER_________ is primarily responsible for maintaining metabolic homeostasis of the body. 3) ______KUPFFER CELLS______ are the resident macrophages of the liver and constitute ~80% of the macrophages in the body.