Pain Management
advertisement

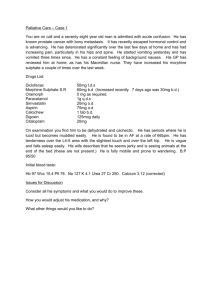
Pain Management In the Palliative Care Setting M. Thomas Beets MD Objectives: • Recognize the importance of cultural differences when developing pain management approaches to patients and families • Have more insight into the multimodality approach to pain management • Identify symptoms occuring in palliative care patients in order to evaluate the various treatment options • Understand ongoing research in pain management of the palliative patient Three Steps • Assess the cause of the pain (may be multiple causes) • Treat each type of pain • Reassess continuously, expecially if pain uncontrolled Categories of Pain • • • • (P)Physical (A)Emotional (I)Social or interpersonal (N)Spiritual or existential Assessment • • • • • • History Character of the pain Physical Pain assessment scale Lab Imaging Bone Pain • Intensifies on movement (Incident pain) • Tender to palpation • Deep and aching Neuropathic Pain • • • • • • • Shooting Burning Paresthesias-tingling Stabbing Scalding Often follows sensory nerve distribution May have allodynia (pain from light touch) Raised Intracranial Pressure • Generalized or posterior head pain • Nausea Visceral Pain • Spasms • Cramping • Colicky • Consider anticholinergics Opioids • Respiratory depression not usually clinically significant • Physical dependence is not addiction • Tolerance verses disease progression • Very wide effective dose range • Are effective by mouth • Rare to have euphoria in palliative patients WHO 3-Step Ladder Step 3, Severe Pain Morphine WORLD HEALTH ORGANIZATION Step 2, Moderate Pain Hydromorphone Methadone Fentanyl Acet or ASA + Oxycodone Codeine + Nonopioid analgesics Hydrocodone Step 1, Mild Pain Aspirin (ASA) Acetaminophen (Acet) Nonsteroidal antiinflammatory drugs (NSAIDs) + Adjuvants Oxycodone + Adjuvants + Adjuvants Equianalgesic Doses of Opioid Analgesics PO, SL Parenteral 100 Codeine 60 - Fentanyl 0.1 15 Hydrocodone 4 Hydromorphone 1.5 150 Meperidine 50 10 Methadone 5 15 Morphine (MS Contin, Morphine, Kadian, Avinza, MSIR, Roxanol) 5 10 Oxycodone (Percodan, Percocet, Oxycontin, Oxyfast, OxyIR) - 1mcg/hr Fentanyl = 2 mg morphine/24 hours Education on Palliative and End of Life Care 2007 - Equianalgesic Example • 40 yr old male, Lung Ca & Bone mets, severe pain Current: mg/24 hrs Morphine Equivalent MS Contin 400 mg TID =1200 mg/24 hrs Duragesic 2 100 mcg patches = 400 mg/24 hrs Roxanol 20 mg/ml x 10 doses of 1ml = 200 Morphine Equivalent Total (Oral) mg/24 hrs Equianalgesic Dose, one-third for IV use IV/Subcut Morphine Rate, divide by 24 hrs =1800 =600 mg/24 hrs =25 mg/hr Principles • • • • • • • • Work with oral morphine equivalents Give around the clock Limited cross-tolerance Opioid rotation Begin with low dose In elderly begin with ½ the usual dose Titrate Q 4 hr booster is 10% of 24 hr dose Principles • Avoid meperidine-metabolized to normeperidine with 15-20 hr ½ life • Avoid pentazocine-inhibits analgesia of morphine • Avoid IM • Treat constipation-softening agent and stimulant, avoid bulking agents Principles • Severe liver disease-opioids and benzodiazepines will have delayed metabolism (avoid methadone and acetominophen) Bone or Soft Tissue Pain • • • • • • Opioids NSAIDS Steroids Calcitonin Radiosotopes biphosphonates Neuropathic Pain • • • • • Tricyclic antidepressants Anticonvulsants Local anesthetics Baclofen Capsaicin Raised ICP • Steroids Visceral Pain • • • • Oxybutinin 5-10 mg po tid Hyoscyamine 0.125mg 1-2 po or sl q 4 hrs prn Transdermal scopolamine Glycopyrrolate 0.2 mg IV, subcut q 4 hrs Other modalities • • • • • Distraction Meditation Massage TENS Acupuncture Other Pearls • • • • • • • • Ketamine Steroids XRT Most opioids are effectively absorbed from the rectum Transdermal, transmucosal, subcut, IV Epidural or intrathecal analgesics Ketorolac Lorazepam Bibliography • EPEC (Education in Palliative and End-of-life Care), Education of all healthcare professionals on the essential clinical competencies in palliative care. www.epec.net Storey P, Knight C, UNIPAC Three: Assessment and Treatment of Pain in the Terminally Ill. 2nd ed. New York:Mary Ann Liebert, 2003. • WHO Ladder: Cancer Pain relief and Palliative Care. Technical Report Series 894. Geneva: World Health Organization; 1990.