235-2673-1
advertisement

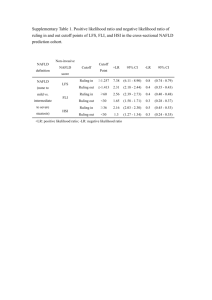
Title : Author’s Name & Affiliation : Relationship of Nonalcoholic fatty liver disease with anthropometric measurement among patients attending a tertiary care hospital of Northern India Purnoor Siraj1 1 Ph.D. Scholar Department of Community Medicine and Public Health, King George Medical College, UP, Lucknow-226003, India Dr. Neera Kohli2, 2 Professor, Department of Radiodiagnosis, King George Medical College, UP, Lucknow-226003, India Dr. VK Srivastava3, 3 Director and Dean of Medical Institute, Integral Institute of Medical Science and Research, Integral University, Lucknow – 226026, Uttar Pradesh, India Dr. S K Singh4, 4 Associate Professor, Department of Community Medicine and Public Health, King George Medical College, UP, Lucknow-226003, India S M Natu5, 5 Professor, Department of Pathology, King George Medical College, UP, Lucknow-226003, India Raj Mehrotra6 6 Professor & Head, Department of Pathology, King George Medical College, UP, Lucknow-226003, India Name of Department(s) : 1. Department of Community Medicine and Public 2. Health Department of Radiodiagnosis 3. Department of Pathology Name of Institution : King George Medical College, UP, Lucknow-226003, India Disclaimers : Nil Address for correspondence : Purnoor Siraj Ph.D. Scholar Department of Community Medicine and Public Health, King George Medical College, UP, Lucknow-226003, India Source of support : Nil Word Count : 1285 Number of table : 2 Number of figure : 2 Conflict of Interest : None declared ABSTRACT BACKGROUND Nonalcoholic fatty liver disease (NAFLD) is an increasingly recognized cause of liver disease worldwide. The present study was conducted with the aim to determine the association between anthropometric measurement and incidence of NAFLD among the adult population. MATERIAL AND METHODS The present cross-sectional study was conducted in the Department of Radiodiagnosis at King Georg’s Medical University, Lucknow. A total of 300 subjects were included by simple random sampling technique. All the subjects aged 20 to 60 years underwent ultrasonography (USG) examination of any part of the body were enrolled in the study. Individuals who have a history of alcohol consumption were excluded from the study. All subjects underwent anthropometric measurement which included Height, weight, waist circumference, hip circumference and mid upper arm circumference (MUAC). Body mass index (BMI) and waist hip ratio (WHR) were calculated using the standard formula. Statistical analysis was done by using SPSS 16.0 version. RESULTS Out of total, 76(25.3%) were found to be diagnosed with NAFLD (95%CI=22.8-27.8) subjects. The cases of NAFLD were significantly higher in males (32.0%) as compared to females (18.7%) (RR=1.17, 95%CI=1.14-2.58, p=0.008). The weight, waist circumference, hip circumference, MUAC, BMI and WHR were significantly (p<0.0001) associated with NAFLD. Likewise, NAFLD was found significantly (p<0.0001) higher among obese and overweight subjects. However, in multivariate logistic regression analysis, sex (adjusted OR=11.30, 95%CI=3.44-37.11, p<0.0001), waist circumference (adjusted OR=1.27, 95%CI=1.56-1.39, p<0.0001), hip circumference (adjusted OR=0.90, 95%CI=0.82-0.99, p=0.04) and BMI (adjusted OR=1.83, 95%CI=1.10-2.20, p=0.001) were significantly associated with NAFLD. CONCLUSIONS It can be concluded that higher anthropometric measurements were significantly associated with NAFLD. Keywords: Non-alcoholic fatty liver disease, Anthropometric measurements, Body mass index, waist hip ratio INTRODUCTION Non-alcoholic fatty liver disease (NAFLD) is defined as the accumulation of fat in the liver in the absence of alcohol consumption and chronic liver disease such as viral hepatitis or drugs may also cause it.1 NAFLD is common clinical condition which is fast assuming importance as a possible precursor of more serious liver disorders, including cirrhosis of the liver and hepatocellular carcinoma2 ultimately leading for need of transplantation3. Absence of signs and symptoms, and lack of sensitive and specific diagnostic tests, limits the ability to estimate the prevalence of NAFLD. The current epidemics of obesity and diabetes among adults and children residing in both developed and developing countries suggest that prevalence of NAFLD should have increased over time, and may be expected to increase further in future. NAFLD was initially described in obese, diabetic women, who did not consume alcohol. The data indicated that NAFLD may have male preponderance or an equal gender distribution and may even occur in the absence of obesity or diabetes.4,5 NAFLD can occur at all ages including childhood, though the highest prevalence is described in those between 40-50 years of age. With some limitations, both population and hospital-based studies from the West report that around 10-24 percent of general population, and 57-74 percent of obese individuals may have NAFLD.4,5 Thus, in view of the above context, the present study was conducted to assess the correlate of NAFLD with the demographic and anthropometric parameters. MATERIAL AND METHODS The present study was conducted at the Department of Radiodiagnosis, King George’s Medical University, Lucknow. Cross-sectional study design was used for data collection. A sample of 300 subjects was calculated by standard formula. Among those patients who meet the inclusion criteria and ready to participate were selected by simple random sampling technique. All the subjects aged 20 to 60 years underwent USG of any part of the body were included in the study. Individuals with the history of alcohol consumption, presence of HBsAg or anti-HCV antibodies, fatty liver suspected to be secondary to hepatotoxic drugs, inflammatory bowel disease and prior surgery that could cause fatty liver, or coeliac disease were excluded from the study. Pregnant and lactating women were also excluded. Only those cases were enrolled who have been recently diagnosed (new cases) with NAFLD. The subjects underwent for abdominal USG to examine for the presence or absence of fatty liver by same equipment and same operator, who was unaware of the clinical and laboratory results. The data was collected through pretested semi structured schedule which included demographic details and anthropometric measurements viz. weight, height, waist circumference, hip circumference and MUAC. Measurements were taken by the interviewer at the end of the interview, following a uniform protocol that included repeat measurements for each participant. If the two measurements differed by more than 0.5 cm, a third measurement was taken. When the two measurements were similar their mean was calculated. When a third measurement was required the mean of the third measurement and the closest to it of the first two measurements was calculated. BMI was calculated as body weight in kilograms divided by the square of height in meters and WHR was calculated as waist circumference divided by hip circumference. The study was approved by the Ethical Committee of the King George’s Medical University, Lucknow. A written consent was taken from all study subjects. The data collected was entered in the Microsoft Excel computer program and checked for any inconsistency. The mean (standard deviation) and percentages were calculated. The chi-square test was used to compare the categorical/dichotomous variable. The unpaired t-test was used to compare two continuous variables. The relative risk (RR) with its 95% confidence interval (CI) was calculated to find the risk of NAFLD. The multivariate logistic regression analysis was carried out to find out the associated factors with NAFLD. The p-value<0.05 was considered as significant. All the analysis was done by using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) software. RESULTS A total of 300 subjects were studied. Out of these, NAFLD was found present among 25.3 percent (95%CI=22.8-27.8) of subjects. Among them 47.0 percent were males and the mean age was 38.99 (±12.99) years. More than half (60.0%) of the subjects were from urban area and belonged to Hindu community (79.7%). Figure 1 showed that the cases of NAFLD was significantly higher in males (32.0%) as compared to females (18.7%) (RR=1.17, 95%CI=1.142.58, p=0.008). RR=1.17, 95%CI=1.14-2.58, p=0.008 (significant) 32.0% 35 30 18.7% Percent 25 20 Male 15 Female 10 5 0 Male Female Axis Title Figure1: Distribution of sex among NAFLD subjects The height was almost similar in both NAFLD (158.07±9.27) and non-NAFLD (158.18±5.74) subjects. The weight was significantly higher (p<0.0001) in NAFLD (65.66±11.84) subjects as compared to Non-NAFLD (53.77±7.28) subjects. Waist circumference (NAFLD: 94.76±13.05, Non-NAFLD: 74.90±7.61), hip circumference (NAFLD: 100.10±10.04, Non-NAFLD: 88.25±7.97), MUAC (NAFLD: 28.31±4.15, Non-NAFLD: 23.85±2.33), BMI (NAFLD: 26.29±4.41, Non-NAFLD: 21.48±2.60) and WHR (NAFLD: 0.95±0.08, Non-NAFLD: 0.85±0.06) were also significantly higher (p<0.0001) among NAFLD subjects as compared to Non-NAFLD subjects (Table-1). Table-1: Comparison of anthropometric measurements between NAFLD and non-NAFLD subjects Anthropometric NAFLD Non-NAFLD t and measurements (n=76) (n=224) p-value Height 158.07±9.27 158.18±5.74 0.12, 0.90 Weight 65.66±11.84 53.77±7.28 10.35, <0.0001* Waist circumference 94.76±13.05 74.90±7.61 16.12, <0.0001* Hip circumference 100.10±10.04 88.25±7.97 10.45, <0.0001* MUAC 28.31±4.15 23.85±2.33 11.61, <0.0001* BMI 26.29±4.41 21.48±2.60 11.50, <0.0001* WHR 0.95±0.08 0.85±0.06 10.99, <0.0001* *Significant Figure 2 depicts that cases of NAFLD was significantly higher (Chi-square for trend p<0.0001) in obese (81.3%) followed by overweight (70%), malnourished (13.3%) and present with normal BMI (11.8%). Percent Chi-square for trend=74.98, p<0.0001 90 80 70 60 50 40 30 20 10 0 81.3% 70.0% Malnourished Normal 13.3% 11.8% Overweight Obese Figure2: Distribution of BMI among NAFLD subjects Associated factors with NAFLD The multivariate logistic regression analysis revealed that sex (adjusted OR=11.30, 95%CI=3.4437.11, p<0.0001), waist circumference (adjusted OR=1.27, 95%CI=1.56-1.39, p<0.0001), hip circumference (Adjusted OR=0.90, 95%CI=0.82-0.99, p=0.04) and BMI (adjusted OR=1.83, 95%CI=1.10-2.20, p=0.04) were significantly associated with NAFLD (Table-2). Table-2: Factors associated with NAFLD (Multivariate logistic regression) Factors Beta coefficient S.E. Adjusted OR (95%CI) p-value Sex Male 2.425 0.607 11.30 (3.44-37.11) Female Ref 1.00 Weight 0.237 0.287 1.27 (0.72-2.22) Waist circumference 0.235 0.046 1.27 (1.39-1.56) Hip circumference -.102 0.050 0.90 (0.82-0.99) MUAC 0.185 0.107 1.20 (0.98-1.49) BMI 0.606 0.711 1.83 (1.10-2.20) Constant 31.619 *Significant, SE: Standard error, OR: Odds ratio, CI: Confidence interval <0.0001* 0.41 <0.0001* 0.04* 0.08 0.001* DISCUSSION NAFLD is associated with some components of metabolic syndrome and CVD risk factors. Over the past decade, it became apparent that NAFLD in some patients is a progressive disorder, leading to cirrhosis and liver failure.6 NAFLD is present in 10-24 percent of the general population in various countries.7 An USG based study conducted in India had showed a prevalence of 24.5%.8 The prevalence of NAFLD was much higher in obese and morbidly obese individuals.9 In the present study, the proportion of NAFLD was found to be 25.3 percent. This is in accordance with the study carried out by Wang et al. (2007) in China and Mohan et al. (2009) in Chennai, India who showed almost similar observation i.e. 24.5 percent and 32.0 percent respectively.10,11 It was also observed in the present study that male subjects constituted higher proportion (32.0%) than the females (18.7%). Similarly, Zhou et al. (2007) in China and Amarapurkar et al. (2007) in Mumbai, India also showed that the prevalence of NAFLD was higher in males as compared to females (22.4% vs. 7.1% and 24.6% vs. 13.6% respectively). 12,3 In the present study, subjects with NAFLD had a higher BMI (26.29±4.41) than those without (21.48±2.60), which is in accordance with a study conducted in coastal regions of India which showed that the persons with NAFLD had a higher BMI (mean 25.9±4.2) than those without (mean 22.1±3.3).2 In another study, among residents of two railway colonies at Mumbai, India showed high BMI (>25) in NAFLD subjects.3 In the present study, bivariate analysis showed that weight, BMI, waist circumference, hip circumference, WHR, MUAC all were significantly associated (p<0.0001) with NAFLD. However, Wan et al. (2007) reported that BMI and WHR were the predictor of NAFLD by biveriate analysis (χ2=69.35, p=<0.01).13 In the present study, the multivariate logistic regression analysis showed that sex (adjusted OR=11.30, 95% CI=3.44-37.11, p=<0.0001), waist circumference (adjusted OR= 1.27; 95% CI= 1.39-1.56, p=<0.0001) and hip circumference (adjusted OR=0.90, 95% CI=0.82-0.99, p=0.0001) were significantly associated with NAFLD. Lee et al. (2006) showed that the weight status [Obesity v/s Non-obesity, odds ratio (or=4.4)] was associated with NAFLD after adjusting for age and metabolic risk factors.14 CONCLUSION The results of the present study clearly demonstrated that there was a strong relationship between NAFLD and anthropometric parameters among adults in the studied population. It is recommended that USG of the liver should be a part of the routine health examination of obese adults. REFERENCES 1. Riquelme A, Arrese M, Soza A, et al. Non-alcoholic fatty liver disease and its association with obesity, insulin resistance increases serum levels of C-reactive protein in Hispanics. Liver international, 2008; 1-9. http://www.higadograso.cl/nafld%20chile.pdf 2. Singh SP, Nayak S, Swain M, et al. Prevalence of nonalcoholic fatty liver disease in coastal eastern India: a preliminary ultrasonographic survey. Tropical Gastroenterology. 2004 AprJun; 25(2):76-79. http://www.ncbi.nlm.nih.gov/pubmed/15471321 3. Amarapurkar D, Kamani P, Patel N, et al. Prevalence of nonalcoholic fatty liver disease: population based study. Annals of Hepatology. 2007 July-Sep; 6(3):161-163. http://www.annalsofhepatology.com/PDF/vol6n3/Hp073-07.pdf 4. Aga. Technical review on nonalcoholic fatty liver disease. Gastroenterology, 2002; 123:1705-1725. http://www.aasld.org/practiceguidelines/Documents/Practice%20Guidelines/technical_nonfat typg.pdf 5. Neuschwander Tetri BA and Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology, 2003 May; 37(5):1202-1219. http://www.ncbi.nlm.nih.gov/pubmed/12717402 6. Leclercq IA and Horsmans Y. Nonalcoholic fatty liver disease: the potential role of nutritional manage-ment. Curr Opin Clin Nutr Metab Care, 2008 November; 11(6):766-773. http://www.ncbi.nlm.nih.gov/pubmed/18827582 7. Nomora H, Kashiwagi S, Hayashi, et al. Prevalence of fatty liver in the general population of Okinawa, Japan. Japanese Journal of Medicine, 1998 May; 27(2):142-149. http://www.ncbi.nlm.nih.gov/pubmed/3047469 8. Singh SP, Nayak S, Swarn M, et al. Prevalence of NAFLD in eastern coastal India-A Preliminary USG study. Tropical Gastroenterology 2004 April-June; 25(2):76-79. http://www.ncbi.nlm.nih.gov/pubmed/15471321 9. Nila Rafiq, and Zobair M. Younossi. Effects of Weight Loss on Nonalcoholic Fatty Liver Disease. Seminars in liver disease, 2008 November; 28(4):427-433. http://www.ncbi.nlm.nih.gov/pubmed/18956298 10. Wang Z, Xia B, MaC, et al. Prevalence and risk factors of Non-alcohholic fatty liver disease in Shuigouohu distric of Wuhan city, central China. Postgrad Med J., 2007 Mar; 83(977):192-195. http://pmj.bmj.com/content/83/977/192.abstract 11. Mohan V, Farooq S, Deepa M, et al. Prevalence of Non-alcohholic fatty liver disease in urban south Indians in relation to different grades of glucose intolerance and metabolic syndrome. Diabetes Res Clin Pract. 2009 Apr; 84(1):84-91. http://www.ncbi.nlm.nih.gov/pubmed/19168251 12. Zhou YJ, li YY, Nie YQ, et al. Prevalence of fatty liver disease and risk factors in the population of South China, World Journal of Gastroenterology. 2007 Dec 21; 13(47):64196424. http://www.wjgnet.com/1007-9327/13/6419.pdf 13. Wan YP, Xu RY, Fang H, et al. The prevalence of non-alcoholic fatty liver disease and its related risk factors in 1180 school children in Shanghai, Zhonghua Gan Zang Bing Za Zhi. 2007; Sep; 15(9):644-648. http://www.ncbi.nlm.nih.gov/pubmed/17903363 14. Lee S, Jin Kim Y, Yong Jeon T, et al. Obesity is the only independent factor associated with ultrasound-diagnosed non-alcoholic fatty liver disease: a cross-sectional case-control study. J Gastroenterol, 2006 May; 41(5):566-572. http://www.ncbi.nlm.nih.gov/pubmed/16638699