Fatty Liver Disease and Genetic
Interactions
Gagan Sood, M.D
Associate Professor
Baylor College of Medicine
• Non alcoholic fatty liver disease ( NAFLD)
Alcohol like liver disease that develops
in people who are not heavy drinkers
Spectrum of Non Alcoholic Fatty Liver Disease
Steatohepatitis
Steatosis
Cirrhosis
Hepatocellular carcinoma
NAFLD Prevalence Worldwide
• Obesity is known risk
factor for NAFLD
• But not all obese people
develop NAFLD
Genes (or nature)
Environment (or nurture)
• 18 Years old Hispanic Male
• Abnormal lab results
AST/ALT
•
•
•
•
3/10
64/117
12/10
62/114
BMI 31
Viral , autoimmune and metabolic studies unremarkable
Fasting Glucose 92, HOMA IR 2.2, Cholestrol 184 TG 224
US increased echogenicity suggestive of fatty liver
Moderate steatosis
Ballooning degeneration
Moderate Inflammation
NAS > 5 STAGE 1
•
Does Fatty liver disease runs in
family ??
• I don’t know …but I know is …no
one runs in family …
Died age 60
50 Yrs. DM
18 M NASH
22 F AST/ALT
26 F OW
28 F OB DM Fatty liver
• Ms AP 58 Hispanic female
• Refd for evaluation of cirrhosis
Abnormal Liver
panel>30 years
Hyperlipidemia for > 6
years
Diabetes mellitus
> 5 years
Cirrhosis 1
Year
• BM1 27 Cholesterol 212 TG 230 Hb A1c 6.9
Died age 68
Died age 60
58 F
50 F OLT
DM
Is there genetic predisposition
• For the development of
a nonalcoholic fatty
liver disease
• Progression to
steatohepatitis and
cirrhosis/HCC
Genetic Basis for NAFLD
• Familial Clustering of NAFLD
• Familial Aggregation studies
• Population based studies
• Genetic Studies
–
Candidate Gene studies
–
GWAS studies
Familial Clustering of NAFLD and
Cryptogenic cirrhosis
• Ninety patients with biopsy
proven NASH
• 18 % of patients had one or
more first degree relative with
NASH
• Nine families, where multiple
members in same generation
or subsequent generation had
NASH
• One family with identical twins,
one received transplant and
other awaiting
Wilner et al Am J Gastro 2001
Struben et al Am J Med 20010
• Familial Aggregation Studies
Familial aggregation study
University of California San Diego
• Hypothesis : NAFLD is highly heritable
• Determined prevalence of fatty liver in siblings and parents of
children with and without NAFLD
• All children were obese or overweight
• Children with histologically proven NAFLD and children
without NAFLD served as probands
• 44 (33 with NAFLD /11 without NAFLD ) , 152 family members
( parents and siblings )
• Hepatic fat content was measured noninvasively using MRI
Schwimmer etal Gastro 2009
Heritability of NAFLD
Adjusted for age, sex, race and BMI the heritability of fatty liver was ( 1.000)
• Fatty Liver was present in 18 % of family
members of NAFLD despite being non obese
and having normal ALT.
Index patient
=
Fatty liver
=
↑ALT
=
Obese
• NAFLD is simply not about weight
–
–
Highly familial…..
Likely Genetic …..
Ethnic differences in NAFLD
Dallas Heart Study Results
Race
n
Black
1105
Liver fat
White< 5.5%
734
Hispanic
410
Total
2240
Hepatic fat measurement by
MR Spectroscopy
Liver fat
< 5.5%
Liver fat
> 5.5%
Steatosis 31 %
Hepatic Triglyceride Content (HTGC)
MRI spectroscopy
50%
45%
45%
40%
33%
Hepatic TG %
35%
30%
24%
25%
20%
15%
10%
5%
0%
BMI
Median age
Hispanics
31
46
White
29
46
Black
30
41
• What we know about the
genetics of Fatty liver
Overview of the metabolic processes influencing the development of NAFLD.
Hooper A J et al. J. Lipid Res. 2011;52:593-617
• Majority of NAFLD patients do not have
inherited gene disorder in a Mendelian
fashion
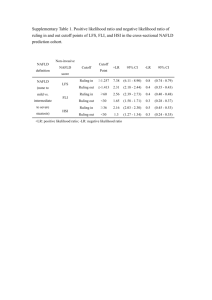
Summary of inherited disorders associated with fatty liver
Disorder
Abetalipoproteinemia
Gene
MTTP
Inheritance
Recessive
Prevalence
∼1 in 1,000,000
Familial
hypobetalipoproteinemia
APOB
Co-dominant
∼1 in 3,000
(heterozygous)∼1 in
1,000,000
Citrullinemia type II
SLC25A13
Recessive
∼1 in 100,000 to 230,000
(Japan)
Familial partial lipodystrophy type
2
LMNA
Dominant
Unknown
Familial partial lipodystrophy type
3
PPARG
Dominant
Unknown
Congenital generalized
lipodystrophy
AGPAT2, BSCL2
Recessive
∼1 in 10,000,000
Neutral lipid storage disorder
PNPLA2, CGI-58
Recessive
Unknown
Wolman disease
LIPA
Recessive
<1 in 300,000
Cholesterol ester storage disease
LIPA
Recessive
∼1 in 40,000
Medium-chain acylcoenzyme-A
dehydrogenase deficiency
ACADM
Recessive
∼1 in 20,000
USF/
multiple genes
???Recessive
1 In 100
Familial Combined
Hyperlipidemia ( FCHL)
Genetic Studies
• NAFLD is a complex polygenic disease
• Recent advances in genomics have identified
multiple variants in different genes involved
hepatic lipid metabolism.
• Genetic variants or also referred as single
nucleotide polymorphism (SNPs)
DNA sequence
(Genotype)
Disease
(Phenotype)
Environment
Genome-wide association study
( GWAS),
• Genome-wide association studies (GWAS) are
performed to identify single nucleotide
polymorphism ( SNPs) in DNA and to study
their association with disease.
SNP A
NAFLD
Unaffected
SNP B
NAFLD
Unaffected
Genome-Wide association study of hepatic
steatosis
• Genome wide scan was
performed to Identify
genetic variants or SNPs
contributing to
difference in hepatic fat
content.
• Each variant was tested
for association with
hepatic fat content
Dallas Heart Study
Genome-wide Association Study in DHS
Non-synonymous SNPs (n = 9,229)
P=5.9 X 10-10
5.4 x 10-6
Chromosome
© Helen Hobbs, Nature Genetics V40, pp 1461, 2008
© Helen Hobbs 2009
C
G
PATATIN LIKE DOMAIN
I148M
481
(ATC) → (ATG))
• PNPLA3 variant ( I148M or G allele ) located on
chromosome 22
• Cytosine to Guanine substitution
• Changes codon isolucine to methionine
1
Proteins within the PNPLA family.
Family of enzymes
regulating lipid
metabolism
Progenitor of this family is
patatin a major protein of
patato tubers
Kienesberger P C et al. J. Lipid Res. 2009;50:S63-S68
©2009 by American Society for Biochemistry and Molecular Biology
PNPLA3 or Adiponutrin
• Highly expressed in liver and adipocytes
• Codes 481 amino acid protein involved in
regulation of lipid metabolism
• It has both lipolytic and lipogenic activity
PNPLA3 Variant
(I148M)
↓ TG Hydrolysis
↑Lipogenic activity
Steatosis
↑ ALT
Ethnic Differences in the Frequency of PNPLA3I148M
AfricanAmericans
Minor Allele
Frequency
0.17
Prevalence of
Hepatic Steatosis
(%)
0
EuropeanAmericans
Hispanics
0.23 0.49
PNPLA3: I148M and Hepatic TG Content
© Helen Hobbs, Nature Genetics V40, pp 1461, 2008
© Helen Hobbs 2009
• If this variant leads to more aggressive
histological disease ?
• If PNPLA3 variant associated with markers of
metabolic syndrome ?
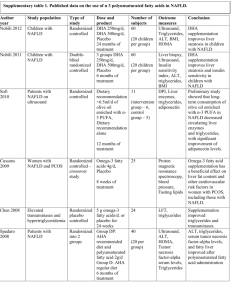
Genetic studies evaluating association of the PNPLA 3 148 M
with Fatty liver
STUDY
POPULATION
n
Key Findings
Romeo
Multiethnic
2111
↑Liver fat in all
↑AST/ALT in Hispanics
Yaun
Indian-Asian
Europeans
12,419
↑AST/ALT
Kotronen
Finns
291
↑Liver fat in all
Sookoian
Argentineans
266
↑steatohepatitis
Kantatzis
Germans
330
↑Liver fat ↑AST/ALT
Romeo
Obese Italians
678
Interaction with obesity
Kollerits
Europeans
4290
↑AST/ALT
Tian
Mexicans
1221
↑ Risk of ALD
Meta-analysis of the influence of I148M variant :Summary of results
I148M variant (GG carriers )
• Higher (73 % ) lipid fat content
• Higher risk (3.4 – fold) of higher necroinflammatory scores
• More risk of develop liver fibrosis
This effect is independent of HOMA-IR ,
Fasting glucose, insulin or BMI
PNPLA3 Variant ( I148M variant )
1. PNPLA3 variant is associated
NAFLD/NASH in both adult and pediatric cohorts
II. Elevated ALT/AST levels
III. Severe steatohepatitis with greater levels of fibrosis
I.
2. PNPLA3 not associated with
I.
II.
Insulin resistance
Metabolic syndrome ( BMI, dyslipidemia, and diabetes mellitus )
3. PNPLA3 variation sensitizes the liver to environmental stressors
I.
Upregulated in presence of obesity
II.
Upregulated by high carbohydrate diet
Overview of the metabolic processes influencing the development of NAFLD.
Hooper A J et al. J. Lipid Res. 2011;52:593-617
Summary
• There appears to be genetic predisposition to development of
NAFLD.
• Supported by familial aggregation of NAFLD and racial and
ethnic difference in prevalence of NAFLD
• Genome –Wide association studies suggests association with
polymorphisms in various genes affecting lipid metabolism,
oxidative stress and insulin resistance.
• There is strong and independent association of PNPLA3
variant with steatosis and liver injury