Document
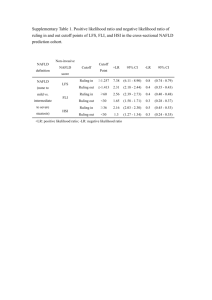
advertisement

Diabetes Mellitus and NonAlcoholic Fatty Liver Diseas Case study • • • • 56 year old Kuwaiti man T2DM and hypercholestremia diagnosed 6 years ago “little” Alcohol intake during weekends Medications - Metformin - Gliclazide - Atorvastatin - Baby Aspirin Case study continued • Physical exam: BMI 40 hepatomegaly • Labs: WBC 4000 HB 12 g/dl plat 122,000 INR 1 Iron Sat 40% ALT 76 iu/L (N < 60) AST 120 iu/L (N<40) ALP 70 iu/L (N) Albumin 39 g/L S Ferritin 600 ug/L(N <350) Abdominal Ultrasound Questions • What is the most likely cause of abnormal LFT in this patient ? • Would you proceed to liver biopsy if viral, autoimmune, and metabolic markers are negative ? • Should you stop statins ? • How would manage this patient ? • Would you recommend bariatric surgery ? Spectrum of Liver Disease in Diabetics Non Alcoholic Fatty live disease Alcoholic liver disease Spectrum of Liver Disease in Diabetics Chronic viral hepatitis especially HCV Autoimmune hepatitis Wilson’s disease Spectrum of Liver Disease in Diabetics Hemochromatosis Secondary iron overload Definition of Non-Alcoholic Fatty Liver Disease (NAFLD) • Evidence of fatty accumulation in the liver by imaging or histology • Alcohol intake less than 21 and 14 drinks per week for men and women respectively • No causes for secondary fat accumulation eg drugs, TPN, starvation, etc Classification of NAFLD NAFLD Non Alcoholic fatty liver NAFL (steatosis without inflammation) Low Risk of progression to cirrhosis Increased CDV mortality Non Alcoholic Steatohepatitis NASH Increased risk of progression to cirrhosis Increased risk of CDV mortality Simple Steatosis NAFL >5%–10% macrosteatotic hepatocytes NASH (without fibrosis) Hepatocyte Ballooning and Mallory Bodies Mallory Body Cirrhosis (stage 4) Early stage 3 (bridging fibrosis) PATHOGENESIS THE TWO (OR THREE) HIT HYPOTHESIS Bacterial overgrowth HSC: hepatic stellate cells EPIDEMIOLOGY Prevalence of NAFLD Vernon G et al. Aliment Pharmacol Ther. 2011;34:274-85. Prevalence of NAFLD in Select Populations By Ultrasound 100 90 80 70 60 50 40 30 20 10 0 non obese Obese T2DM undergoing bariatric surgery Chalasani N et al. Hepatology 2012;55:2005-23 NAFLD—Histological Spectrum and Natural History Time Progression 10-20yrs HCC 2-5 % Cirrhosis 20-25 % Lobular Inflammation NASH 5% Non Alcoholoc fatty liver NAFL Risk Factors For Progression To Cirrhosis • Risk factors for progression: -Diabetes -BMI > 30 ≥ 2 factors consider liver biopsy to - AST> ALT assess stage of disease -Age > 50 -Hispanic - Ferritin > 1.5 X nml Diagnosis Diagnostic Approach • Liver enzymes • Viral, autoimmune, and metabolic ( iron studies and ceruloplasmin) • Lipid profile • TSH • Imaging: US, CT, MRI, Fibroscan • NAFLD score • Liver biopsy Normal appearance of the liver at US. The echogenicity of the liver is equal to or slightly Greater than that of the renal cortex (rc). Normal Liver Fatty liver Fibroscan NAFLD fibrosis score Age BMI Hyperglycemia Platelet count Albumin AST ALT http://nafldscore.com NAFLD fibrosis score • < -1.455: predictor of absence of significant fibrosis (F0-F2 fibrosis) • ≤ -1.455 to ≤ 0.675: indeterminate score • > 0.675: predictor of presence of significant fibrosis (F3-F4 fibrosis) Treatment • Life style modification • Pharmacologic therapy • Surgery Summary of life style intervention studies: Diet and physical activity 1 2 3 4 5 1.Lazo M et al. Diabetes Care 2010. 2. Kantarzis K et al. Gut 2008 3. Promrat K et al. Hepatology 2010. 4. St George A et al. J Gastro Hepatol 2009. 5. Hallsworth K et al. Gut 2009 Lifestyle Interventions • Aim Hb A1c < 6.5 • Correct dyslipidemia • Alcohol consumption should be avoided or limited to one drink a day. • 10 % weight loss led to improvement in steatosis, necrosis, and inflammation; not fibrosis. • Moderate exercise ( 150-200 min/wk)alone can reduce steatosis but may not affect necroinflammation • 2-3 Cups of filtered coffee may prevent fibrosis ??? * Promrat, et al. Hepatology 2010 ** Dunn, et al. Hepatology 2008 ** Gunji. et al. Am J Gastro 2009 ** Moriya, et al. Alim Pharm Ther 2011 ***Ruhl , et al. Clin Gastro Hepatol 2005 Pharmacotherapy Insulin Sensitizers Metformin Pioglitazone Hepatoprotectants Ursodeoxycholic acid Vitamin E Omega-3 Summary of trials involving Pioglitazone therapy for NAFLD • Abbreviations: RCT, randomized controlled trial; , improvement; , no effect . AASLD recommendations: • Pioglitazone can be used to treat NASH in patients who have DM but long term safety and efficacy has not been established • Caution in patient with impaired myocardial function Summary of trials involving Metformin therapy for NAFLD Abbreviations: n/a, not available; RCT, randomized controlled trial; , improvement; , no effect. Summary of trials involving Vitamin E therapy for NAFLD effect • Abbreviations: n/a, not available; RCT, randomized controlled trial; , improvement; , no effect. Vitamin E: Safety Concerns • Meta-analysis including 136,000 participants found taking Vitamin E supplements > 400 IU/day had a higher risk of all cause mortality* • Vitamin E > 400 IU/day increases risk of prostate cancer in relatively healthy men** *Miller et al . Annals of Internal Medicine 2005 ** Klein, et al. JAMA 2011 AASLD Recommendations-Vit E • “until further data supporting its effictiveness become available, vit E is not recommended to treat NASH in diabetics” Summary of trials involving UDCA therapy for NAFLD • Abbreviations: n/a, not available; AASLD Recommendations • Metformin and usrodeoxycholic acid do not induce histologic improvement • Not recommended as specific therapies for NAFLD Summary of Bariatric surgery trials for NAFLD • Abbreviations: n/a, not available; , improvement; , no effect AASLD Recommendation on Bariatric Surgery • Premature to consider foregut surgery as an option to specifically treat NASH • Foregut surgery is not contra-indicated in otherwise eligible pts with NASH or NAFLD WITHOUT cirrhosis • For those with cirrhosis: type, safety and efficacy of foregut surgery is not established Statins • CVD common cause of death for NAFLD and NASH • Stratify risks and treat accordingly • Several studies show NAFLD and NASH pts are not at increased risk of liver injury over general population* • No RCTs with histological end points using statins to treat NASH *Chalasani, et al. Am J Gastro 2012 GREACE Study: Safety of Statins in Patients with Abnormal LFT • Athyros et al Lancet 2010 AASLD Recommendation on Statins “Given lack of evidence that patients with NAFLD and NASH are at increased risk for serious drug-induced liver injury from statins, they can be used to treat dyslipidemia in patients with NAFLD and NASH.” Take Home Messages • NAFLD is very common in diabetics who are at higher risk of cirrhosis and hepatocellular ca than the general population • Viral, autoimmune and metabolic liver disease should be ruled out in diabetics with NAFLD • Liver biopsy maybe considered in high risk patients • Lifestyle modification is the cornerstone of treatment • No drugs are currently recommended • Statins and fibrates are safe in NAFLD patients except in those with decompensated cirrhosis Thank You