7 - Ipswich and East Suffolk CCG
advertisement

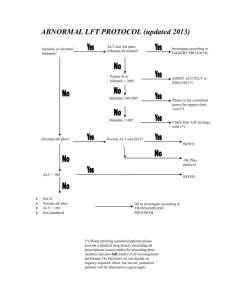
Deranged LFTs Pathways Dr A H Mohsen MD (KCL), MRCP, DTM&H A H Mohsen Consultant Gastroenterologist Main causes for progression of liver disease Alcohol consumption Obesity Hepatitis B/C Common serum liver chemistry tests AST/ALT Hepatocellular damage Bilirubin Cholestasis, impaired conjugation, or biliary obstruction GGT Cholestasis or biliary obstruction Alk-P Cholestasis, infiltrative disease, or biliary obstruction PT/Albumin Synthetic function How common abnormal LFTs? Abnormal LFTs: 1%–4% of the asymptomatic population Gastroenterology 2002 Those who have LFTs check: >10 are above twice limit of normal abnormal test result resolve spontaneously in 38% of patients Ryder, BMJ 2001 149 asymptomatic patients with elevated alanine aminotransferase levels who underwent liver biopsy Cause % Fatty live 56 Non-A, Non-B hepatitis 22 Alcohol related 11 Hepatitis B 3 Other diagnosis 8 No cause 2 Scand J Gastroenterol 1986 1124 consecutive patients with chronic elevations in aminotransferase levels 81 no definable cause had LB Cause Number Steatosis 41 NASH 26 Fibrosis 4 Hepatitis B 3 Cirrhosis 2 Normal 8 Am J Gastroenterol 1999 Abnormal LFTs Isolated rise Bili up to 3x ULN exclude haemolysis and Conjugated bilirubin Probably Gilbert’s ALT/AST Raised ALK-P Abnormal LFTs Isolated rise Bili up to 3x ULN ALT/AST Raised ALK-P Check GGT Normal: Bone disease Raised: x2 ULN >3 months USS & AMA Normal: repeat in 3-6 months Trend not improving abnormal: refer ALT/AST ALT<100 100-400 mod Risk Review 1-3 /12 Review 1 months Normal No further action ALT>400 Raised: x2.5 ULN >3 months Hep A,E,CMV,EBV USS, liver screen USS & liver screen Referral to Gast USS & liver screen Negative screen Fat on USS Positive screen No fat on USS Treat diagnosis NAFLD + ETOH Referral to Gast Fatty liver (NAFLD/NASH) Fibro-scan <7 >7 Criteria Low risk High risk Age <45 >45 Diabetes/IFG Absent Present BMI <30 >30 AST/ALT <1 >1 Platelet count >150 <150 Albumin >34 <34 If > 3 criteria • Life style intervention • Repeat fibro-scan in 1-2 years • GP to monitor Referral to Gast Isolated elevation of GGT Levels < 3 times upper limit of normal: Monitor 6-12 monthly Alcohol intake advice Review medications Levels > 3 times upper limit of normal: Repeat in 3 months Alcohol intake advice Review medications fibro-scan > 7 USS & fibro-scan If trends worsening fibro-scan > 7 Refer to Gast Recent case ST, 62 male Presented in March with severe UGIB Stabilised OGD: Likely gastric varices (D/W Addenbrokes) Catastrophic variceal bleed 10 hours later Died PMH: Type II DM (1999) Hypertension IHD ST, 62 male Current medications: 1. 2. 3. 4. 5. 6. 7. NovoRapid 20-40 units pre meal Lantus 40 units pre bed Metformin MR 1g bd Bendroflumethiazide 2.5mg Omeprazole 5mg Diltiazem MR 90mg Irbesartan 75mg Ref. Range 12/03/2014 ALP (30 - 130) 105 359 328 297 228 Albumin (35 - 50) 31 38 40 46 41 ALT (0 - 41) 37 74 88 93 78 Total Bilirubin (0 - 20) 22 18 21 13 14 22/09/2011 02/11/2010 27/10/2008 31/01/2007 NAFLD prevalence Liver biopsy/post-mortem series Hultcrantz R 1986, Ground K 1982 15-39% Third of the population was found to have hepatic steatosis in US (MRI) Hepatology 2004; 40:1387 Obese persons NAFL 60-90%, NASH 20-25%, cirrhosis 2-3% Diabetic : 50 % Morbidly obese and diabetic person NAFL 100%, NASH 50%, cirrhosis 19% Dixon J 2001, silverman J 1989, 1990 Examination Process A mechanical pulse is generated at the skin surface, which is propagated through the liver. The velocity of the wave is measured by ultrasound. The velocity is directly correlated to the stiffness of the liver, which in turn reflects the degree of fibrosis. - the stiffer the liver is the greater the degree of fibrosis. Project Overview A novel diagnostic pathway to detect significant liver disease in the community Amount Won £100,000 Innovation Challenge Prize Winner, November 2013 Summary Clear pathways NAFLD is the most common cause 1/3 of deranged LFTs resolve spontaneously Identify those at risk and refer early