Hypoglycaemia in Diabetes Guideline
advertisement

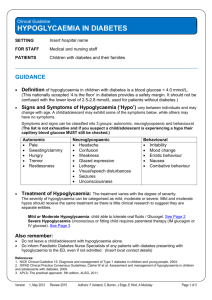
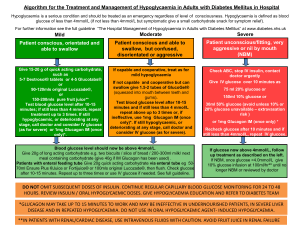
Clinical Guideline HYPOGLYCAEMIA IN DIABETES SETTING Insert hospital name FOR STAFF Medical and nursing staff PATIENTS Children with diabetes and their families _____________________________________________________________________________ GUIDANCE Definition of hypoglycaemia in children with diabetes is a blood glucose < 4.0 mmol/L. (This nationally accepted ‘4 is the floor’ in diabetes provides a safety margin. It should not be confused with the lower level of 2.5-2.8 mmol/L used for patients without diabetes.) Signs and Symptoms of Hypoglycaemia (‘Hypo’) vary between individuals and may change with age. A child/adolescent may exhibit some of the symptoms below, while others may have no symptoms. Symptoms and signs can be classified into 3 groups: autonomic, neuroglycopaenic and behavioural. (The list is not exhaustive and if you suspect a child/adolescent is experiencing a hypo their capillary blood glucose MUST still be checked.) Autonomic Pale Sweating/clammy Hungry Tremor Restlessness Neuroglycopaenic Headache Confusion Weakness Glazed expression Lethargy Visual/speech disturbances Seizures Unconsciousness Behavioural Irritability Mood change Erratic behaviour Nausea Combative behaviour Treatment of Hypoglycaemia: The treatment varies with the degree of severity. The severity of hypoglycaemia can be categorised as mild, moderate or severe. Mild and moderate hypos should receive the same treatment as there is little clinical research to suggest they are separate entities. Mild or Moderate Hypoglycaemia: child able to tolerate oral fluids / Glucogel. See Page 2 Severe Hypoglycaemia Unconscious or fitting child requires parenteral therapy (IM glucagon or IV glucose). See Page 3 Also remember: Do not leave a child/adolescent with hypoglycaemia alone. Do inform Paediatric Diabetes Nurse Specialists of any patients with diabetes presenting with hypoglycaemia to the ED, even if not admitted. (Insert local contact details) References: 1. NICE Clinical Guideline 15: Diagnosis and management of Type 1 diabetes in children and young people, 2004. 2. ISPAD Clinical Practice Consensus Guidelines, Clarke W et al. Assessment and management of hypoglycaemia in children and adolescents with diabetes, 2009. 3. APLS: The practical approach, 5th edition, ALSG, 2011. Version 2, May 2014 Review 2016 Authors: F Ackland, C Burren, J Edge, E Hind, A McAulay, Bill Lamb Page 1 of 3 Treatment of Mild or Moderate Hypoglycaemia 1. Follow this box if child is co-operative and able to tolerate oral fluids 2. Follow this box if child refuses to drink, is uncooperative, but is conscious Give 10-15g of fast acting oral carbohydrate such as: Give Glucogel® or Dextrogel® (formerly known as Hypostop®). This is a fast acting sugary gel, in an easy twist top tube. Each tube contains 10g glucose. Squirt tube contents in the side of each cheek (buccal) evenly and massage gently from outside enabling glucose to be swallowed and absorbed quickly. 3-4 glucose tablets 150 ml (~ ½ cup) sugary drink (not diet) such as cola (15g) or Lucozade Sport (10g) 3 jelly babies NB Chocolate or milk WILL NOT bring glucose levels up quickly enough DO NOT use Glucogel in an unconscious or fitting child. After 10-15 minutes recheck blood glucose: 1. If still low (<4 mmol/l) and able to take oral fluids repeat Box 1 above (once) 2. If still low (<4 mmol/l), refuses to take oral but is conscious, follow Box 2 above (once) 3. If deteriorated after first run through above or not responded after having administered 2nd dose of above then proceed to Box 4 (See Page 3) 4. If better and blood glucose > 4.0 mmol/L follow Box 3 (see below) 3. If feeling better and blood glucose level >4.0mmol/L, give 10 -15g slow acting carbohydrate snack (or normal meal if it is meal time) such as: One slice of toast One piece of fresh fruit (not banana) A cereal bar (max 15g CHO) One plain digestive or hobnob biscuit Glass of milk (200ml) (Patients on insulin pumps may have differing local policy guidelines as to the need for this slow acting carbohydrate and/or adjustment of basal insulin rates following correction of a hypoglycaemic episode. Please refer to your local policy guideline.) Retest 20-30 minutes later to confirm target glucose (>4.0 mmol/L) is maintained. If hypo is just before a meal time (when insulin is usually given) the hypo should be treated first and once the blood glucose is >4.0 mmol/L the insulin should be given as usual. DO NOT OMIT INSULIN, especially important with an early morning hypo. Review history of hypo: If possible the cause should be identified and if necessary the insulin dose adjusted, e.g. for early morning/night-time hypo ask about extra exercise the evening before and details of bedtime snack. Treatment of Severe Hypoglycaemia Follow this page if child unconscious or fitting (or also not responded from page 2) Version 2, May 2014 Review 2016 Authors: F Ackland, C Burren, J Edge, E Hind, A McAulay, Bill Lamb Page 2 of 3 CHECK CAPILLARY BLOOD GLUCOSE AND CONFIRM HYPOGLYCAEMIA (<4 mmol/l) Do involve medical assistance by this stage: Outside hospital: call emergency services. Inside hospital: bleep paediatric registrar Place in the recovery position if possible and assess Airway Breathing Circulation DO NOT attempt to give any oral fluid or Glucogel® If IV access is present go straight to box 5 instead of box 4 4. Give Glucagon (Glucagen) by Intramuscular injection Dose: Check if IM glucagon has been given at home or in ambulance Check expiry date Administer intramuscularly in the thigh. Age <8 yrs or body weight <25 kg: 0.5 ml (half syringe) Age >8 yrs or body weight >25 kg: 1 ml (whole syringe) Glucagon is a fast acting drug and the child/adolescent should respond after 5 minutes. After the child has regained consciousness leave him/her on one side as one of the common side effects of glucagon is nausea/vomiting 5. IV 10% Glucose If recovery is not adequate after a dose of glucagon or IV access is readily available AND BG <4 mmol/l, then administer 2mls/kg 10% dextrose as slow IV bolus. Note: If alcohol causes or contributes toward hypoglycaemia, glucagon may be ineffective (as hepatic stores of glycogen depleted) and intravenous glucose will be required. Further Monitoring after a severe hypo: Check blood glucose after 5 minutes, 15 minutes and then half hourly until BG stable above 5 mmol/l Continue to monitor baseline observations: oxygen saturation, pulse, blood pressure, temperature Record presence of or absence of ketones. Document management Inform diabetes team if during the day, or if concerns during the night. Do not omit normal insulin unless instructed to do so by diabetes team. If blood glucose >4.0 mmol/l and child able to tolerate oral fluids: Offer clear fluids, and once tolerating clear fluids offer simple carbohydrates, such as toast, crackers (see box 3, page 2) Try to identify the cause of hypoglycaemia and discuss this with the patient/family Refer to diabetes team for review of treatment, advice or education Version 2, May 2014 Review 2016 If child not improving: If patients have protracted vomiting and are unable to tolerate oral fluids, hospital admission and IV glucose infusion must be considered, especially if a child has returned to the emergency department with further hypoglycaemia during the same intercurrent illness. If a child/Adolescent remains unconscious on correction of BG consider cerebral oedema, head injury, adrenal insufficiency or drug overdose Authors: F Ackland, C Burren, J Edge, E Hind, A McAulay, Bill Lamb Page 3 of 3