Emergency Care (hypoglycaemia)
advertisement

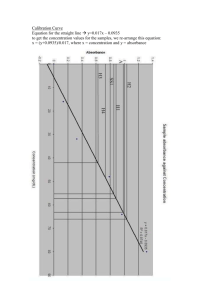
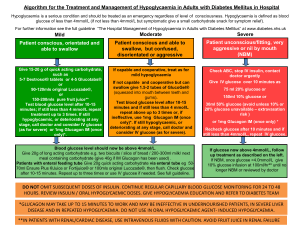
Presentation title Emergency Care Part 2: Treating and Preventing Hypoglycaemia Slide no 2 Emergency care 1 Managing DKA 2 Treating and preventing hypoglycaemia 3 Surgery in children with diabetes Slide no 3 Hypoglycaemia • One of the most common acute complications of diabetes • Low blood glucose • May causes severe symptoms • Coma or seizures • Limitation in the management of diabetes • Effective treatment and prevention are key Slide no 4 Criteria • Symptoms of hypoglycaemia occur around <3.5 mmol/l (but not always!) • Awareness of symptoms depend on background values • Confusion may occur with rapidly dropping BGs but also with only modest hypoglycaemic values • Counter regulation in individuals without diabetes begins at <4 mmol/l • “Hypo” or “low sugar” symptoms due to bodies’ selfcorrecting hormonal responses (adrenalin) Slide no 5 Symptoms • Trembling • Rapid heart rate • Pounding heart (palpitations) • Sweating • Pallor • Hunger and/or nausea • Irritability Neuroglycopenia • • • • • • • Difficulty concentrating Irritability Blurred or double vision Disturbed colour vision Difficulty hearing Slurred speech Poor judgement and confusion • Dizziness and unsteady gait • Tiredness • Nightmares • Inconsolable crying • Loss of consciousness • Seizures Slide no 7 DCCT and now standard Classification of severity • Mild Hypoglycemia • Recognition and self treatment • Usually <3.9 mmol/l • Moderate Hypoglycemia • Aware of symptoms • Needs assistance to take care of themselves • Severe Hypoglycemia • Loss of consciousness (coma), convulsion, marked confusion • Usually <2.5 mmol/l Slide no 8 Management • Identify hypoglycaemia • Symptoms • Blood glucose values • Teach how to recognize and manage hypoglycaemia • Learn symptoms • Learn responses to symptoms • Re-enforcement by family and heath care workers • Treat the hypoglycaemia • Determine cause (when possible) Slide no 10 Treatment (1) • Feed the child simple sugar • Rapid acting carbohydrate e.g. sweetened drinks, fruit juices, glucose in water, sweets, packet of sugar • Enough to make symptoms go away… don’t overtreat • Give 0.3 g/kg of glucose if available • Follow up with regular meal or snack – controversial but certainly reasonable if less than optimal monitoring possible Treatment (2) • If the child has severe symptoms • Not able to eat • Glucagon (0.5 mg for age <12 yr, 1.0 mg for ages >12 yr) • IV glucose (3 ml/kg of 10% dextrose, 1 ml/kg of 30% dextrose) • Oral rapid acting foods - glucose, sugar or honey Slide no 12 Determine cause • • • • • Too much insulin – dose error or timing Too little/late food Increased activity, sometimes hours later Illness, esp. gastrointestinal viruses Alcohol • Does not cause hypo but makes it nearly impossible for body to self-correct since “liver is busy” • Knowing cause helps to avoid future hypoglycaemia Slide no 13 Prevention • Reminders about the symptoms of hypoglycaemia • Reminders about the causes • Help to identify risk factors e.g. age, longer duration of diabetes, higher doses, etc. • Repeated episodes of hypoglycaemia should result in specific advise to prevent recurrences • Re-involve adults and caregivers/direct supervision • Often some psychological issues Questions Changing Diabetes® and the Apis bull logo are registered trademarks of Novo Nordisk A/S