Tardive dyskinesia and akathesia
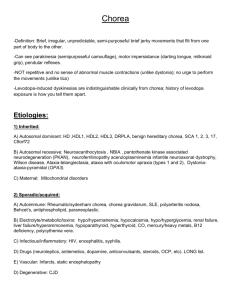
advertisement
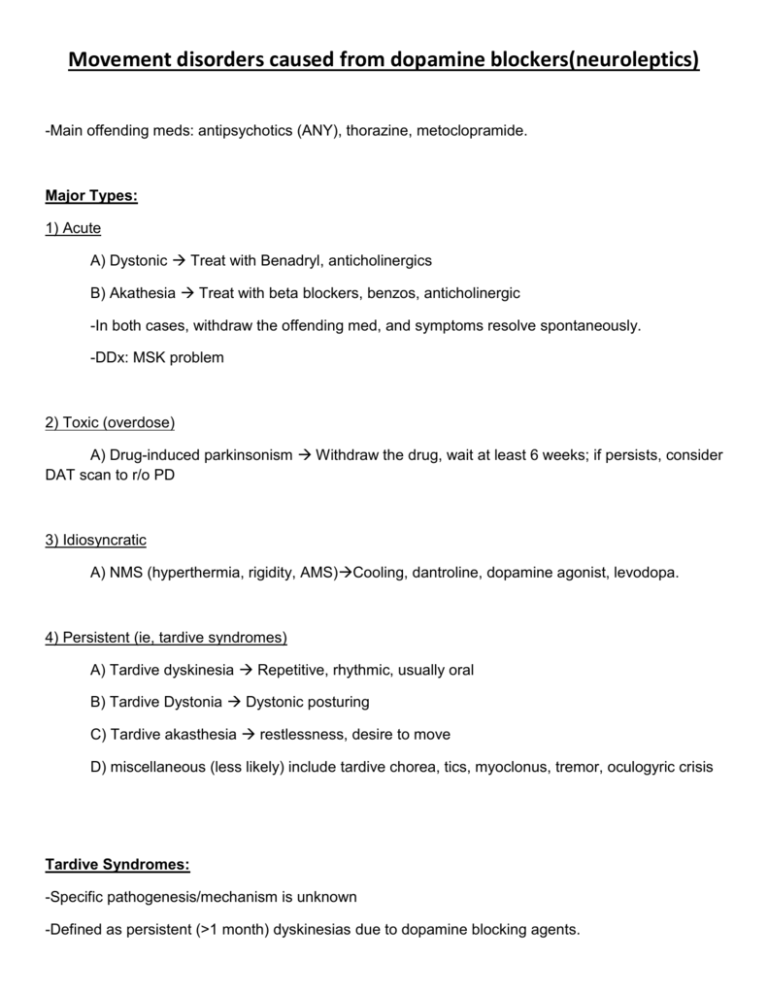
Movement disorders caused from dopamine blockers(neuroleptics) -Main offending meds: antipsychotics (ANY), thorazine, metoclopramide. Major Types: 1) Acute A) Dystonic Treat with Benadryl, anticholinergics B) Akathesia Treat with beta blockers, benzos, anticholinergic -In both cases, withdraw the offending med, and symptoms resolve spontaneously. -DDx: MSK problem 2) Toxic (overdose) A) Drug-induced parkinsonism Withdraw the drug, wait at least 6 weeks; if persists, consider DAT scan to r/o PD 3) Idiosyncratic A) NMS (hyperthermia, rigidity, AMS)Cooling, dantroline, dopamine agonist, levodopa. 4) Persistent (ie, tardive syndromes) A) Tardive dyskinesia Repetitive, rhythmic, usually oral B) Tardive Dystonia Dystonic posturing C) Tardive akasthesia restlessness, desire to move D) miscellaneous (less likely) include tardive chorea, tics, myoclonus, tremor, oculogyric crisis Tardive Syndromes: -Specific pathogenesis/mechanism is unknown -Defined as persistent (>1 month) dyskinesias due to dopamine blocking agents. -Onset can be a few days after medication started, to even a year after medication stopped (though rule of thumb is <3 months after medication stopped). -CAN be permanent. Sooner drug is discontinued, sooner it fades away (can easily last for months or even years after drug is stopped). -Often occurs as combination of tardive symptomatology -RISKS OF IT OCCURING: Age (Elderly means increased likelihood it occur, more severe, more likely to stay around), women, longer duration of med exposure, more potent med, interruptions in drug. SECOND GENERATION ANTIPSYCHOTICS DON’T DECREASE THE RISK. A) Classic TD: -rhythmic and stereotyped. -Oral>limb>trunk >respiratory/diaphragm. -Classically see tongue-popping, marching in place, akathesias, and orofacial movements. -Of note, can KEEP TONGUE OUT (unlike chorea). ‘-NOT impair swallowing. -Sensory trick of putting finger to lips can suppress it. -DDx brainstem strokes, chorea, oromandibular dystonia, idiopathic, HD, liver problems, meds (phenytoin, lithium, TCAs, antihistamines, anticholinergics, levodopa). B) Tardive Akathesia: -Unable to sit still, specific discomfort/pain (often focal and burning) that relieved with movement, usually more wide spread, present significantly throughout the day (not just at night). Vs RLS. -DDx other med effects (levodopa, anticholinergics, dopamine depleters) C) Tardive dystonia: -Can mimic primary dystonia. -Tends to manifest as either 1) retrocollis + extension elbows + flexion wrists, 2) trunchal flexion during walking, or 3) oromandibular/lingual dystonia D) Tardive Chorea -Mainly occurs when suddenly withdraw a drug. Self-limited (6 weeks), mainly in kids, Chorea resembles syndenham chorea, as appears restless. Treatment of Tardive syndromes: -If at all possible, taper offending agent SLOWLY. DO NOT ABRUPTLY WITHDRAWL, IT WILL WORSEN THE TARDIVE SYMPTOMS AND NECESSITATE THE DRUG BEING ADDED BACK AND RE-TAPERED. -If can’t withdraw drug (ie, they are psychotic), try to switch to clozapine or quetiapine. -Tardive dyskinesias: Not much. Botox (if focal). Little evidence for lithium, keppra, baclofen, Depakote, ECT. Takes TIME to resolve. 50% of patients will have 50% improvement in 5 years from time of med removal. 1/3 of patients will normalize within 3 months of med removal. -Akathesias: Tetrabenazine, klonopin. Not much evidence for anything else.