Chorea - UMMS Wiki
advertisement

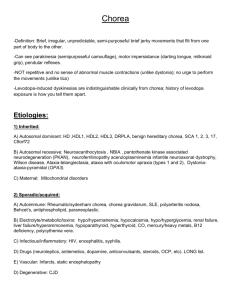
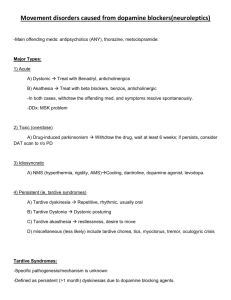
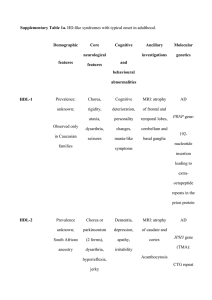
Chorea -Definition: Brief, irregular, unpredictable, semi-purposeful brief jerky movements that flit from one part of body to the other. -Can see parakinesia (semipurposeful camouflage), motor impersistance (darting tongue, milkmaid grip), pendular reflexes. -NOT repetitive and no sense of abnormal muscle contractions (unlike dystonia); no urge to perform the movements (unlike tics) -Levodopa-induced dyskinesias are indistinguishable clinically from chorea; history of levodopa exposure is how you tell them apart. Etiologies: 1) Inherited: A) Autosomal dominant: HD ,HDL1, HDL2, HDL3, DRPLA, benign hereditary chorea, SCA 1, 2, 3, 17, C9orf72 B) Autosomal recessive: Neuroacanthocytosis , NBIA , pantothenate kinase associated neurodegeneration (PKAN), neuroferritinopathy aceruloplasminemia infantile neuroaxonal dystrophy, Wilson disease, Ataxia-telangiectasia, ataxia with oculomotor apraxia (types 1 and 2), Dystoniaataxia-pyramidal (OPA3). C) Maternal: Mitochondrial disorders 2) Sporadic/acquired: A) Autoimmune: Rheumatic/sydenham chorea, chorea gravidarum, SLE, polyarteritis nodosa, Behcet’s, antiphospholipid, paraneoplastic. B) Electrolyte/metabolic/toxins: hypo/hypernatremia, hypocalcemia, hypo/hyperglycemia, renal failure, liver failure/hyperammonemia, hypoparathyroid, hyperthyroid, CO, mercury/heavy metals, B12 deficiency, polycythemia vera. C) Infectious/inflammatory: HIV, encephalitis, syphilis. D) Drugs (neuroleptics, antiemetics, dopamine, anticonvulsants, steroids, OCP, tardive). E) Vascular: Infarcts, static encephalopathy D) Degenerative: CJD Pearls from the history: -Acute onset: Vascular or sydenham’s -Chronically progressive: neurodegenerative -Nonprogressive: benign hereditary chorea -Episodic: paroxysmal hyperkinetic chorea (genetic) Workup for acquired/sporadic chorea: -Comprehensive acquired chorea labs: COMP, CBC, TSH, PTH, pregnancy test, ANA, ESR/CRP, B12, HIV, CPK (chorea-acanthocytosis, Mcleod), ferritin (neuroferritinopathy if low), ceruloplasmin (wilsons), 24 hour urine copper, lactate/pyruvate (mitochondrial), AFP (ataxia telecangectasia, ataxia with oculomotor apraxia), antigliadin (celiac), uric acid (Lesch-Nyhan), peripheral blood smear, DSDNA, ENA-5, antiphospholipid antibodies, urine and serum organic and amino acids, RPR, ammonia, heavy metals. +/- paraneoplastic panel (anti-YO, anti-Hu, anti-CRMP5), CJD workup. -MRI, CT C/A/P vs. PET scan (? occult malignancy) Workup for genetic chorea: Examples: -HL2: South African families. Onset 3-4th decade. Chorea, dementia, parkinsonism, dystonia, death in 15-25 years. -DRPLA: Average age onset 30 (but ranges 1st-7th), looks like HD but with severe ataxia, parkinsonism. AD. -Neuroacanthocytosis: AR. Onset 20-40 years. Tongue pushing food out of mouth (oro-buccal lingual dyskinesias), self-mutilation, seizures, absent reflexes, vocalizations, dystonia, tics, elevated CPK/LFTs, peripheral neuropathy/myopathy. Slow chorea. Sudden loss of axial muscle tone (“rubber man”). Diagnosis by finding acanthocytes. EMG will show neuropathy. PET shows pre-synaptic and post-synaptic dopamine deficit. -Benign hereditary chorea: AD. Starts in early childhood, then static in 2 nd decade. No dementia, but can get learning problems/MR, thyroid problems, lung problems. Often in Brain-Lung-Thyroid syndrome. -C9orf72 expansion: Dystonia, chorea, myoclonus, tremor, rigidity. -PKAN: X-linked, get brain iron accumulation. Global developmental delay/epilepsy/spasticity in childhood, followed by dystonia, chorea, cognitive decline, parkinsonism. MRI shows EYE OF THE TIGER sign. Tx: -Treat underlying cause -Tetrabenazine (depletes dopamine) -Antipsychotics -Antiepileptics (Valproic acid, carbamazepine) -? DBS