03-nardocci
advertisement
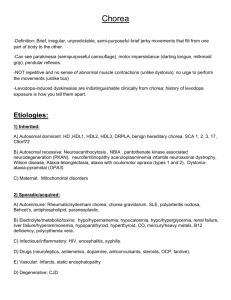
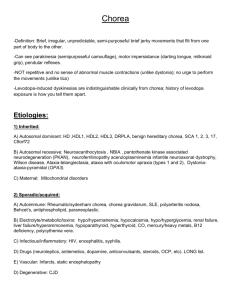
Cognitive and psychiatric features of movement disorders in children N Nardocci Fondazione IRCCS Istituto Neurologico“C Besta” Milano Limitation to the review • Small number of the study including small number of participants • Often studies not based on standardized cognitive and psychiatric assessment • Definition of behavioural or psychiatric symptoms not uniform • Difficulties in interpretating the cognitive and psychiatric manifestation as the result of the disease itself or as a consequence of therapy • Findings are presented as prevalence without indicating the severity of disability • In none the assessment include the impact on quality of life Sydenham chorea: cognitive aspects • Lower scores on WISC-R and impaired verbal fluency (Swedo FE et al 1993; Cunningham t al 2006) • ADHD reported in up 60% of children with persistent chorea (Maia DP et al 2005) • ADHD symptoms reported before the appearance of chorea (Ridel Kl et al 2010) Sydenham chorea: psychiatric aspects • Retrospective studies: 46% of patients decribed behavioural changes with emotional liability, depression, anxiety, irritability, ageregressed behaviour (Zomorrodi A et al 2006; Swedo et al 1993; Ridel et al 2010) • Prospective studies: obsessive-compulsive symptoms (70-81%); OCD (17-21%). (Swedo el al 1993;Ashbar et al 1998) Benign Hereditary chorea • Low-average IQ reported in isolated cases • No reports of cognitive decline (Schrag A et al 2000; Kleiner-Fisman G et al 2007) • Adult onset psychosis reported in several families (Kleiner-Fismann G et al 2007) Tourette syndrome • ADHD (up to 70%) • OC symptoms (up to 30%) • OCD ( up to 26%) • Separation anxiety (14%) • Bipolar disorders (11%) • Depression (2-9%) • Schizophrenia (3%) • Pervasive developmental disorders (5%) (Ganizadeh A et al 2009; Bund L et al 2009; Robertson 2006; Denckla MB 2006; Roessner V 2007 Opsoclonus-myoclonus syndrome • Cognitive impairment, lower intellectual performances (60-80%) and behavioural problems (17-90%). (Hammer et al 1995; Tate et al 2006; Turkel et al 2006; De Grandis et al 2009) • Behavioural disturbances: rage attacks, OC symptoms, Hyperactivity, Depression and ADHD (Tate et al 2006) Wilson disease • Psychiatric symptoms up 50% of adults before treatment. (Shanmugiah A et al 2008) • Psychiatric symptoms seems to occur with a higher percentage (60%) in the adolescentonset an may precede motor signs(Ullah M et al 2009) Primary and DYT1 dystonia • No data referring on cognitive and psychiatric aspects in children • Anxiety or depression before the onset of motor sign in 23% among a group of young people with Primary dystonia (aged 3-28 yrs). (Koukouni V et al 2007) • Depression has been identified in a series of asynptomatic DYT1 carrier (Heimann GA et al, 2004) Dystonia plus syndromes • Learning disability and depression have been reported in some families affected by DTY5 Dystonia (Hoffmann GF et al 2003; Hahn H et al 2001) • OCD usually appearing after the motor symptoms depression and anxiety in myoclonus dystonia (DYT11) (SaundersPullmann et al 2002; Nardocci 2012) Conclusions • Existing informations suggest that non motor deficits differ according with age, severity and progression of the disease • Non motor symptoms in children with MD may cause major disability • The cognitive and psychiatric manifestations may result from the disease itself or may be a consequence of therapy • Their recognition is mandatory and may facilitate management and the treatment requires clinical expertise • ADHD has been reported as a major comorbidity in Tourette syndrome • OCD is manifest in Sydenham chorea, Tourette syndrome and myoclonus dystonia • Cognitive and behavioural problems are typical of opsoclonus-myoclonus syndrome • Depression and anxiety are more frequent in genetic dystonia DYT11 Dystonia (SCGE gene mutations) • No evidence of cognitive defects in children • OCD may appear after the onset of motor symptoms in childhood (Saunders-Pullmann et al 2002; Nardocci 2012)