Antipsychotic Presentation
advertisement

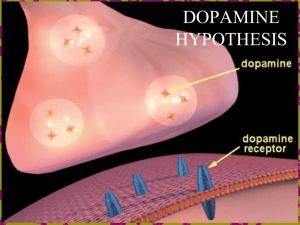
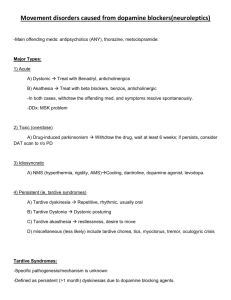
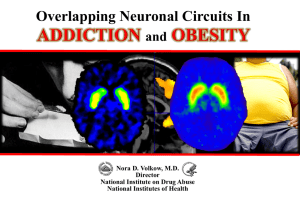
PSYCHOSIS #A syndrome of chronic disordered thinking and disturbed behavior (schizophrenia, mania, depression) Deficits in integrating thought and perception with emotion (some refer to a loss of “cognitive control”) paranoid delusions/thought insertion/ideas of reference hallucinations (generally auditory, but can be visual) loss of affect/poverty of speech/social withdrawal impaired ability to function with others idiopathic or organic etiology Prevalence of schizophrenia: 1% of population worldwide MENTAL ILLNESSES Environmental factors Maturational factors Neuronal connectivity Neurotransmitters Receptors/drug targets Schizophrenia Environmental Factors Exposure to infections ( in utero) Toxic/Traumatic Insults ALTERATIONS IN NEURODEVELOPMENT Autoimmunity Stress during gestation or early in childhood/adolescence Maturational Processes Apoptosis Synaptic Pruning Myelination (prenatal to adolescence) Unmasking Genetic Vulnerability Neuronal Plasticity • Structural changes during development and in response to environmental factors • Changes in neurotransmitter activity in response to environmental factors • Neurotrophic factors and changes in gene transcription – (eg. neuroregulin-1 which regulates neuronal migration) • Continues throughout life of the organism • Underlies learning and memory NEURONAL CONNECTIVITY Functional activity in neocortex of schizophrenic patients may be decreased Myelination Synaptic pruning Hormonal effects of puberty Exposure to stressors Defective connections in midbrain, nucleus accumbens, thalamus, temporo-limbic and prefrontal cortex STRUCTURAL BRAIN CHANGES IN SCHIZOPHRENIA • Schizophrenics show deficits in tasks involving prefrontal cortex or those requiring working memory • Prefrontal cortical thickness is reduced 5-10%, neuron size is down, but no change in neuron number • Synaptic connectivity is reduced • Medial dorsal thalamus shows 30% reduction in neuron number • Prefrontal cortex receives fewer projections from the thalamus • Hippocampus shows altered cytoarchitecture The Dopamine Hypothesis Schizophrenia results from excess activity of dopamine neurotransmission because: ALL antipsychotic drugs block dopamine receptors. Stimulant drugs which act through dopamine can produce schizophrenic-like behaviors (eg.amphetamines). Levodopa, a dopamine precursor, can exacerbate schizophrenic symptoms, or occasionally elicit them in non-schizophrenic patients. Higher levels of dopamine receptors measured in brains of schizophrenics. Brain [DA] increases during psychotic episodes but not during remissions. A HYPOTHESIS IN TRANSITION All antipsychotic drugs which block dopamine receptors do not reverse all symptoms positives are more responsive negatives may even be exacerbated Antipsychotics blocking DA and 5-HT receptors seem better for both positive and negative symptoms NMDA glutamate--based on effects of PCP in humans DA metabolites in CSF & plasma not significantly elevated in schizophrenics Antipsychotic drugs block DA receptors immediately but antipsychotic benefits take several days to weeks to occur New Findings Polymorphism of COMT gene with increased activity and more efficient metabolism of DA leading to: lower than normal prefrontal cortex DA release=hypofrontality Polymorphism of -7 nAChR on chromosome 15 as cause of disturbance in sensory gating=normalized by nicotine Partial D-2 agonist and 5-HT-2/5-HT-1a antagonist effective for positive/negative symptomatology DOPAMINE RECEPTORS: THE HOLY GRAIL FOR ANTIPSYCHOTIC MEDS? Dopamine recognized as a neurotransmitter in the 1950’s Five dopamine receptor subtypes: D-1,-2,-3,-4,-5 Drug naive schizophrenics show elevated D2 receptor number Cortex has much higher amounts of D1 than D2 receptors chronic antipsychotic drugs downregulate D1’s in the cortex and striatum THE HOLY GRAIL FOR MEDS, CONT’D Striatum has high concentrations of D1 & D2 receptors All effective antipsychotics possess some threshold level of D2 receptor blockade striatal D2s may be the site for antipsychotic drug-induced movement disorders clozapine upregulates cortical D2s at doses that do not affect striatal D2s Limbic structures contain high concentrations of D4s clozapine has high affinity for D4s, but selective D4 antagonists fail to show antipsychotic efficacy Serotonin inhibits dopamine neurotransmission atypicals show serotonin binding ability DRUG TARGETS, CONT’D The newer “atypicals” have the ability to block the behavioral effects of phencyclidine (PCP) PCP elicits behavioral/ cognitive symptoms indistinguishable from schizophrenia PCP is an uncompetitive blocker of NMDAglutamate ion channel function NEUROTRANSMITTERS Overactivity of dopamine in limbic regions (positive symptoms?) Abnormalities in dopamine storage, vesicular transport, release or reuptake NMDA-glutamate hypofunction (negative symptoms?) ANTIPSYCHOTIC DRUGS • no compound can target a given symptom • therapeutic effects correlated to potency at D-2 dopamine receptors • all have effects on other non-dopamine receptors (sideeffects, or therapeutic effects) • can also be used for Tourette’s, control of acute mania, intractable hiccups, choreas and ballisms DRUG TARGETS Dopamine receptors: D1, D2, D3, D4, D5 Serotonin receptors: 5-HT-1A, 2A, 3, 6, 7 Norepinephrine: -1 & -2 Muscarinic acetylcholine: mACh-1 & 4 Histamine: H-1 & 2 Dopamine, norepinephrine & serotonin transporters NMDA-glutamate receptor Dopamine Receptors Occupancy—therapeutic vs. side effects At therapeutic doses the “classical” antipsychotics occupy >75% of dopamine D-2 receptors. 85% occupancy needed to get extrapyramidal side effects. Clozapine, the “atypical”, blocks only 35% D-2 receptors at therapeutic doses. DRUG CLASSES • • • • • • • Phenothiazines: eg. chlorpromazine Thioxanthenes Butyrophenones: eg. haloperidol Diphenylbutylpiperidine Dihydroindolone Dibenzoxazepines: eg. clozapine Benzisoxazol: eg. risperidone PHARMACOLOGICAL PROPERTIES • Neuroleptic syndrome: – suppression of spontaneous behavior – loss of initiative and interest (anhedonia) – loss of affect and emotional content – slowness of movement – Parkinson-like extrapyramidal effects • Unpleasant when given to non-psychotic individual TYPE MANIFESTATIONS MECHANISM Autonomic nervous system Dry mouth, loss of accommodation; difficulty urinating, constipation Muscarinic blockade Orthostatic hypotension, impotence, failure to ejaculate Alpha adrenergic blockade Parkinson’s syndrome; akathisia, dystonia Dopamine receptor blockade Tardive dyskinesia Dopamine receptor supersensitivity Toxic confusional state Muscarinic blockade Galactorrhea; amenorrhea; infertility, impotence Hyperprolactinemia secondary to dopamine receptor blockade Central nervous system Endocrine system Spectrum of Adverse Effects Caused by Antipsychotic Drugs Low Potency High Potency Fewer extrapyramidal reactions (especially thioridazine) More sedation, more postural hypotension Greater effect on the seizure threshold, electrocardiogram (especially thioridazine) More likely skin pigmentation and photosensitivity Occasional cases of cholestatic jaundice Rare cases of agranulocytosis More frequent extrapyramidal reactions Less sedation, less postural hypotension Less effect on the seizure threshold, less cardiovascular toxicity Fewer anticholinergic effects Occasional cases of neuroleptic malignant syndrome SIDE EFFECTS, cont’d. • • • • • Parkinsonian syndrome neuroleptic malignant syndrome akathisia acute dystonic reactions tardivie dyskinesia Comparison of Tardive Dystonia and Tardive Dyskinesia Tardive dystonia Tardive dyskinesia Strikes younger Strikes sooner in the course of neuroleptic treatment Poor prognosis More males Patients with mood disorders may be more susceptible Anticholinergics may improve condition Strikes older Strikes later in the course of neuroleptic treatment Variable prognosis More females (?) Patients with mood disorders may be more susceptible Anticholinergics usually worsen condition TABLE 6. Comparison of Tardive Dystonia and Tardive Dyskinesia Tardive dystonia Tardive dyskinesia Strikes younger Strikes sooner in the course of neuroleptic treatment Poor prognosis More males Patients with mood disorders may be more susceptible Anticholinergics may improve condition Strikes older Strikes later in the course of neuroleptic treatment Variable prognosis More females (?) Patients with mood disorders may be more susceptible Anticholinergics usually worsen condition SIDE EFFECTS • Autonomics--related to blockade of alphaadrenergic and muscarinic receptors • Endocrine effects, primarily prolactin increases • Disruption of thermoregulatory control • Hypersensitivity reactions; eg. agranulocytosis with clozapine; browning of vision with thioridizine Stress & Schizophrenia Schizophrenic patients have altered sensitivity to stress They display abnormalities in autonomic nervous system and hypothalmic-pituitary adrenal function in response to stress Coping abilities seem best preserved in schizophrenics who suffer the least negative symptoms Cognitive deficits in schizophrenics may cause them to be less well adapted to their environment Schizophrenics have difficulty filtering incoming sensory stimuli Indications for Antipsychotic Drugs Schizophrenia Schizoaffective disorders Acute control of mania Tourette’s syndrome Huntington’s chorea and ballism Intractable hiccups