MOVEMENT DISORDERS - The Children`s Medical Center of Dayton
advertisement
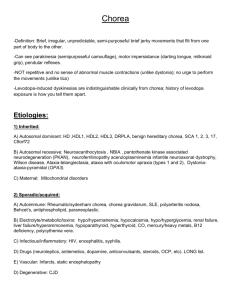
MOVEMENT DISORDERS IN CHILDREN September 2010 Gogi Kumar MD Child Neurologist Dayton Children’s Hospital Wright State University Movement disorders in children Can be paroxysmal: Dystonia, tics, tremors No single diagnostic test Clinical description is important Often confused with seizures, malingering, cerebral palsy Treatment can be effective in a small percentage Type of abnormal movements Chorea Athetosis Dystonia Myoclonus Tics Tremors Stereotypies Movement disorders in children The most common types of abnormal movements in children Tics Drug induced Dystonia related to CP Sydenham’s chorea Essential or task specific tremor Psychogenic tremor Movement disorders in children Percentage in a series of 684 patients under 18 yrs of age Movement disorders in children, Fernandez-Alvarez, Aicardi Tics are different !!! Can be reproduced voluntarily Patient has partial control Do not interfere with voluntary activity Tics predominate in facial muscles, proximal limbs May persist in sleep Chorea Chorea is a rapid, purposeless, irregular, jerky movement that seems to flow randomly from one part of the body to another. Etiology Genetic choreas Huntington’s disease Neuroacanthocytosis Ataxia telangiectasia Spinocerebellar ataxias Paroxysmal kinosegenic choreoathetosis Etiology of chorea Parainfectious and autoimmune disorders Sydenham’s chorea SLE Wilson’s disease Chorea gravidarum Antiphospholipid antibody syndrome Post infectious or post vaccinal encephalitis Etiology of chorea Athetotic Cerebral Palsy Bilirubin encephalopathy Basal ganglia tumors Metabolic disorders. Sydenham’s Chorea Most common cause of chorea in children Typical age is 8-9yrs with female preponderance. 4-8 weeks after GABHS pharyngitis. 20 – 35% may have hemichorea. Hypotonia, emotional lability, ADHD, tics, OCD symptoms may accompany it. 60-80%pts have cardiac involvement. Sydenham’s chorea Self limited disorder with remission within 6-9 months. Recurrence is reported in 20-50% of patients Inv: ASO titres, throat culture, cardiac examination. Treatment: Sodium Valproate, Carbamazepine, Pimozide. Tetrabenazine, Tiapride SSRIs for OCD symptoms. Rheumatic fever prophylaxis. Patient with possible Sydenham’s chorea History including FH and drug use,physical examination Typical history Atypical history or hemichorea Imaging MRI No other cause ESR,CRP,Echocard iogram,ECG Jones criterion not met Other cause Jones criterion met ASO/Anti Dnase B,Throat culture, Rapid antigen test,GABHS, RBC, TFT,Renal and hepatic function,ceruloplasmin,RF antinuclear antibodies Sydenham’s chorea Other cause Oosterveer DM et al. Sydenham’s chorea: a practical overview of the current literature. Pediatr Neurol 2010;43:1-6. Drug induced chorea Dopamine receptor blocking agents Dopamine agonists SSRIs TCAs OCPs Lithium. Investigations and Treatment MRI to rule out basal ganglia lesion. Rheumatological markers. Specific Gene testing according to the presence of other features. Treatment: Antidopaminergic drugs are the mainstay of treatment. Risperidone olanzapine, tetrabenazine, haloperidol. Amantidine, Gabapentin, Carbamazepine, Valproic acid. PANDAS PANDASen Thriving Extinct Endangered PANDAS (pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections) Presence of obsessive-compulsive disorder or tic disorder Onset between age 3 years and beginning of puberty Onset or exacerbation of signs are temporally related to group A b-hemolytic streptococcal infection. Abnormal results of neurological examination (hyperactivity/choreiform movements or tics during an exarcerbation) Dystonia and Athetosis Dystonia is a syndrome of sustained muscle contractions causing abnormal postures or twisting and repetitive movements. Athetotic movements are complex, wormlike, irregular, non propositional and predominate over postural anomalies and on the distal parts of limbs and face. Common types of Dystonia Benign paroxysmal torticollis in infancy Dopa responsive dystonia Idiopathic torsion dystonia Transient idiopathic dystonia of Infancy Secondary dystonia: 1.Structural brain damage :Hemidystonia 2. Metabolic dystonia: Glutaric aciduria Wilson’s disease, Lesch Nyan syndrome Homocystinuria. Idiopathic Torsion Dystonia DYT1 Onset is before 15 yrs of age Onset in 1 limb, foot inversion is common Initially it appears in only certain postures. Course is progressive for 5-10 yrs and then becomes stationary. N shaped progression Tremors, swallowing difficulties, myoclonus can be present. Idiopathic Torsion Dystonia DYT1 Investigations: Blood count and search for acanthocytes MRI Copper and ceruloplasmin Slit lamp examination Lysosomal enzymes (hexosaminidase,galactosidase) ERG Organic acids in urine. Dopa responsive dystonia (DYT5) First 12 yrs of life (median age of onset 4.5 and 6 yrs) Females to male 2.5:1 Fatiguability, clumsiness of gait, dystonic posture limited to one foot . Severity of the dystonia worse during the day and improves with sleep. Postural tremor / Hyperactive reflexes present. Marked and prolonged effect of L-Dopa (5-30mg/kg/day) Mutations of DYT-5 gene GTP cyclohydrolase1 gene Transient idiopathic dystonia of infancy Onset before 5 months of age Abnormal posture limited to one hand. Arm is abducted and the forearm pronated with flexion at the wrist May be permanent but can be paroxysmal Dystonia disappears when the infant performs propositive movements. Transient idiopathic dystonia of infancy Treatment of Dystonia A trial of low dose Levo Dopa (62.5mg-100mg) 2-3 times daily is warranted High doses of Benzhexol (Artane) Start with 4-5mg/day and increase to 80 mg/day Tetrabenazine and Pimozide/Haloperidol Baclofen Clonazepam and Diazepam Botox Deep Brain stimulation Tremor in children 10-20% of pediatric movement disorders. Action tremor most common. Rest tremor uncommon, bad prognosis. Task specific tremor . Can occur in conjunction with dystonia/ myoclonus. Etiology of Tremors Benign Physiological Shuddering attacks Jitteriness Spasmus nutans Hereditary Essential tremor Fragile X premutation Strokes or Brain Lesions Thalamus, midbrain, or cerebellum Peripheral neuropathies Mitochondrial encephalopathies Metabolic Hypoglycemia B12 deficiency Inborn errors of metabolism Endocrine Hyperthyroidism Hyperadrenergic states Drugs, Toxins Valproate Phenytoin Carbamazepine Lamictal Gabapentin Lithium Tricyclic antidepressants Bronchodilators Caffeine Amphetamines Thyroxine Neuroleptics Cyclosporin Amiodarone Serotonin reuptake inhibitors Cocaine Mercury Manganese Psychogenic Essential tremor Adapted from Bain and colleagues Core criteria (features that must be present): Bilateral action tremor of the hands and forearms (but not rest tremor); or isolated head tremor with no signs of dystonia No other neurological signs, with the exception of the cogwheel phenomenon Secondary criteria (features that are supportive, but not necessary): Long duration of symptoms (over 3 years) Positive family history Responsiveness to alcohol Epidemiology of ET Adults: Prevalence of 0.24%- 4.8%, no reliable data in children. 15-30% of Adults report onset in childhood. M:F 3:1 in pediatrics. Tremor onset at a mean age of between 3-11 yrs. Differential diagnosis of ET Wilson’s disease and hyperthyroidism should always be excluded. If tremors are associated with dystonia, myoclonus,ataxia,seizures,weakness or it is unilateral suspect other causes. Postural and kinetic tremor Detailed medical history and examination Findings suggest other than essential tremor History and physical examination suggests essential tremor. Targeted diagnostic testing Diagnosis of essential tremor Treat underlying cause of tremor Assess for disability and determine whether treatment is needed. Determine whether daily therapy is required Propranolol as needed Pediatr Drugs 2009; 11 (5) Initiate maintenance therapy with propranolol 0.5–1 mg/kg/day in three divided doses titrated up to 4 mg/kg/day Deep brain stimulation Monitor for progression Poor response Second-line agents: primidone, topiramate, gabapentin, benzodiazepines, botulinum toxin Shudder attacks http://video.yahoo.com/watch/2666541?fr=yvmtf Start in the first yr of life. Brief bursts 5-15 sec of rapid tremor of head and arm No change in level of consciousness EEG normal Precede essential tremor Propranolol may be effective. References Pediatric Neurology ,Principles and Practice. Swaiman, Ashwal and Ferriero, Fourth Edition. Movement Disorders in Children. Emilo Fernandez-Alvarez and Jean Aicardi Ferrara J,Jankovic J .Epidemiology and Management of Essential Tremor in children, Pediatric Drugs 2009;11(5):293-307. Keller S, Dure L. Tremor in childhood,Semin Pediatr Neurol 2009 ;16: 60-70. Cardoso F et al. Seminars on Chorea, Lancet Neurol 2006; 5: 589–602 Sanger TD et al, Definition and Classification of Hyperkinetic Movements in Childhood, Movement Disorders Vol. 25, No. 11, 2010, pp. 1538–1549 Gonzalez-Alegre P, The Inherited dystonias Semin Neurol 2007;27:151–158 E. Ferna´ndez-Alvarez. Dystonia : The Paediatric Perspective European Journal of Neurology 2010, 17 (Suppl. 1): 46–51 Martino D et al,The PANDAS subgroup of tic disorders and childhood-onset obsessive–compulsive disorder Journal of Psychosomatic Research 67 (2009) 547–557 Kirsch DB, Mink JW. Psychogenic movement disorder in children. Pediatr Neurol 2004;30:1-6. Oosterveer DM, Overweg-Plandsoen WCT, Roos RAC. Sydenham’s chorea: a practical overview of the current lit- erature. Pediatr Neurol 2010;43:1-6. Jancovic Joseph, Treatment of Dystonia Lancet Neurol 2006; 5: 864–72 Thank You !