2nd Annual HCSSC Symposium presentation(Barbara)
advertisement
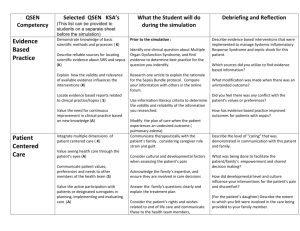
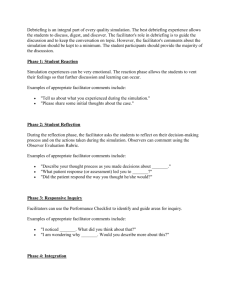
Simulation Coordinator and NUR 270 Course Coordinator met to discuss format of Capstone Simulation based competency blueprint mutually agreed upon Previous competency was inherited as a skill based demonstration lab. Objectives formulated Faculty training session -Dry Run After the 2012 Symposium in Charleston, we changed the skills based competency to a simulation focusing on leadership, resource allocation, delegation, critical thinking, communication and prioritization. Consultation with the GHS Simulation Center resulted in the current simulation involving 5 students and 7 faculty. The current simulation allows us to facilitate 40 students in 4.5 hours with 7 facilitators. Consistent faculty Time management – have increased the time from a 20 minute stagger to 30 minute stagger starts Effective communication/scheduling between multiple staff, multiple entities, students etc. Organization and consistency in a purposefully chaotic environment. Faculty hours0.80 faculty hours per student during simulation with 40 students. This does not include prep time on the part of the simulation center or course leadership. Student recognizes patient needs and prioritizes patient care Student performs initial and focused assessment Student communicates effectively Student provides a safe environment Student delegates appropriately Student demonstrates appropriate leadership skills Student Prep Debriefing During Simulation Reflection on Learning 4 Different Patients selected for student assignment Post Partum Hemorrhage, COPD- Rapid Response, DKA ready for discharge, Pediatric Head Injury All patients had a safety error to correct; critical decisions to make; communication to Charge Nurse/MD; and reassessment of the patient’s changing condition. Student name_________________ Time_______________ May 22 2013 RAPID RESPONSE- Check List RAPID RESPONSE INITIAL ASSESSMENT- total time frame not to exceed 9 minutes 1 Enter room to check patient 2 Did not perform IWIPE Identify self Wash hands Identify patient Provide privacy Explain procedure 3 Did not check patient chart 4 Did not perform initial assessment Checks VS –normal VS Pulse RR O2Sat B/P 5 Did not complete a focused Neuro Assessment Did not complete a focused Cardiac Assessment Did not complete a focused Respiratory Assessment NURSING INTERVENTIONS- total time to decide to call Rapid Response 5 minutes 8 Did not rechecks vital signs – BP is low must recognize and please show rhythm SVT 180 narrow QRS at 9 min mark Pulse RR O2Sat Did not reassess B/P Did not reassess Heart sounds Did not reassess Breath sounds 9 Pulse OX- change in O2 SAT down to 80% at 10 minute mark RR increased to 25 10 Increases Oxygen to patient via NC 11 Change in neuro status- pt states I don’t feel good Did not reassess neuro status IV for KVO 12 Did not recognize need for Rapid Response Team 13 Did not communicate with Charge Nurse 14 Did not utilize ISBARR format (for MD or Rapid Response Team ) 15 Did not communicate effectively with the patient SAFETY VIOLATIONS Intervention/therapy in place that was not ordered Patient left alone during critical period Bed left in high position/unlocked Inappropriate use of side rails Patient not identified properly Personal protective equipment Failure to recognize ISBARR - Identify, Situation, Background, Assessment, Recommendation, Read back Organizational grid: › Time slots › Faculty Patient Charts Charge Nurse Report Scenario Checklists Debriefing Room students receive a 23 minute individual debriefing from the faculty running their scenarios and are then sent into the debriefing room to talk about the scenario as a group. Addition of Scenarios to interchange cases Continue to refine checklists Addition of a rubric to grade the simulation Develop the preparatory assignment for the students- Admission Ticket Addition of EHR documentation Utilization of individual rooms rather than quad room Video evaluation of charge nurse SIMULATION SPECIALIST- Paula Rozov Melanie Cason , RN, MSN, CNE Fran Lee, DBA, CHSE