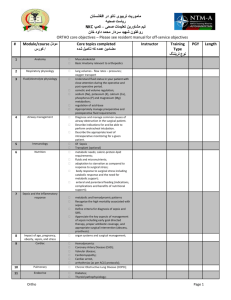
ENT Core objectives
advertisement

ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives # Module/course مودل کورس/ Core topics completed مضامین عمده که تکمیل شده 1 Anatomy Musculoskeletal Basic Anatomy Ear- Nose –Throat (see below) 2 Respiratory physiology 3 Fluid/electrolyte physiology lung volumes - flow rates – pressures; oxygen transport Understand fluid status in your patient with close attention during the operative and post-operative period. Identify and manage electrolyte abnormalities. Identify and manage acid-base disturbances. Diagnose and manage common causes of airway obstruction in the surgical patient. Describe indications for and how to perform surgical airways Cricothyroidectomy Open trachostomy Describe indications for and be able to perform orotracheal intubation. Describe the appropriate level of intraoperative monitoring for a given patient. Of Sepsis Transplant (optional) metabolic needs; caloric-protein-lipid requirements; fluids and micronutrients; adaptation to starvation as compared to response to surgical stress; body response to surgical stress including catabolic response and the need for metabolic support; enteral and parenteral feeding (indications, complications and benefits of nutritional support); 4 Airway management 5 Immunology 6 Nutrition 7 Sepsis and the inflammatory response metabolic and hemodynamic patterns Recognize the high mortality associated with sepsis. Define criteria for diagnosis of sepsis and SIRS. Appreciate the key aspects of management of sepsis including early goal directed therapy, proper antibiotic coverage, and appropriate surgical intervention (abscess, prosthesis). organ systems and surgical management; Hemodynamics Coronary Artery Disease (CAD); Valvular disease; Cardiomyopathy; Cardiac arrest, arrhythmias (as per ACLS protocols); Chronic Obstructive Lung Disease (COPD); 9 Impact of age, pregnancy, obesity, sepsis, and stress Cardiac 10 Pulmonary 8 Instructor Training Type نوع تریننگ PGY Page 1 Length ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives 11 Endocrine 12 Renal 13 Hepatic 14 Hematologic 15 Risk assessment strategies and scores 16 Diagnostic modalities and radiation safety 17 Medical treatments and their impact on surgery (Optional) Diabetes; Thyroid pathophysiology; Parathyroid pathophysiology; Adrenal pathophysiology; Renal failure Cirrhosis Liver failure Screening for diatheses Hypocoagulable states Hypercoagulable states anesthetic risks cardiac risks ICU risk scores trauma assessment including GCS nutritional assessment preoperative screening tests and their limitations. plain radiography; ultrasound; CT scan; MRI technology; fluoroscopy immunosuppression; cancer chemotherapy; radiotherapy; common drugs with impact on hemostatic function and how to correct their impact; tribal customary medicine (alternative medicine); blood products (types, indications and adverse reactions). purpose and basis of staging; basic principles of neoplastic transformation including tumor growth and spread; pathology requirements for appropriate assessments; definition of common pathological terms such as but not limited to neoplasia, malignancy, dysplasia, metaplasia and atypia; genetics of neoplasia and families at risk; environmental carcinogens; paraneoplastic syndromes; principles of multi-modality therapy. community and hospital acquired bacteria, fungi and viruses; impact of blood borne pathogens, including HIV, Hepatitis B and Hepatitis C. Describe the differences of healing by primary closure, by delayed primary closure and by secondary intention, and the indications for each. Recognize the various phases of wound healing and the approximate time course associated with each phase. Describe the significance of epithelialization and defense against contamination. Describe clinical factors that may retard healing. Recognize and differentiate wounds, which 18 Cancer Care (Optional) 19 Management of common infections 20 Wound healing Page 2 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives 21 Principles of prophylaxis 22 Principles of anesthesia 23 Pre and Post-operative care have resulted in a loss of tissue and those, which have not. Recognize and differentiate clean vs. infected wounds; which can be safely closed primarily and those which cannot. Describe the functions of a dressing. Contrast “dehiscence” and “evisceration” and describe their presentation and management. Assess a wound for signs of infection, attending to the local heat, erythema, and excessive pain; outline the management of an infected surgical wound. Describe the factors that lead to non-healing chronic wounds. Describe factors that lead to pressure ulcers and treatment. wound and systemic infection thromboembolism (DVT, PE) tetanus. local anesthetic agents, indications, contraindications and administration; regional anesthetics; general anesthetics; procedural sedation, indications, contraindications and administration; complications arising from the administration of anesthesia. Describe the complications of and be able to order appropriately: O Barbiturates O Local anesthetics O Neuromuscular blockade reversal agents O Neuromuscular blockers O Sedatives Describe the role and indications for use of epinephrine in local anesthesia. Pre-operative assessment in traumatic injury: Discuss primary assessment and emergency management of patients with craniofacial trauma. Develop competence in determining which patients require immediate surgical intervention. Develop competence in basic emergent procedures especially those related to airway management. Pre-operative assessment in an elective procedure: Recognize and understand common medical co-morbidities that can affect a surgical procedure. Understand how to properly assess a patient pre-operatively, and when to order additional pre-operative testing. Develop competency in the intra-operative preparation of the patient for basic head and neck procedures including patient positioning, surgical prepping, pharmacologic prophylaxis, premedication and airway concerns. Understand the indications for medical Page 3 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives 24 Wound healing and wound care versus surgical treatment of nasal and paranasal sinus disorders. Pre-, intra-, peri-, and post-operative management of patients undergoing rhinologic and endoscopic skull base procedures, including identification and proper management of rhinologic emergencies and complications. Post operative management: Discuss prevention of peri-operative cardiac events. Discuss proper fluid management and appropriate use of blood products in the postoperative patient. Discuss the causes of postoperative fever. Discuss the differential diagnoses for patients with postoperative respiratory difficulty. Understand how to manage post-operative pain. Describe the differences of healing by primary closure, by delayed primary closure and by secondary intention, and the indications for each. Recognize the various phases of wound healing and the approximate time course associated with each phase. Discuss the growth factors involved in wound healing. Describe the significance of epithelialization and defense against contamination. Describe clinical factors that may retard healing. Recognize and differentiate wounds, which have resulted in a loss of tissue and those, which have not. Recognize and differentiate clean, cleancontaminated, contaminated and infected wounds. Describe the wound management based on the wound. Specifically what wound can be safely closed primarily and which ones cannot. Describe the management of traumatic wounds, including tetanus prophylaxis. Assess a wound for signs of infection, attending to the local heat, erythema, and excessive pain; outline the management of an infected surgical wound. Describe the signs of necrotizing soft tissue infection. Obtain proper wound specimen for gram stain and cultures. Identify, differentiate and treat wound complications of hematoma and seroma. Identify wound dehiscence and “evisceration” and initiate care. Describe the functions of a dressing. Debride and pack wounds and apply dressings. Perform extensive wound debridement under supervision. Page 4 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives 25 Basic anatomy 26 Epistaxis Stridor Discuss the specific recommendations for management and prevention of complications from animal and insect bites. Describe the factors that lead to non-healing chronic wounds. Describe factors that lead to pressure ulcers and treatment. Describe the applied anatomy of the ear, nose (including paranasal sinuses, anterior and middle cranial fossa), mouth, pharynx, larynx and neck. Understand the basic sciences, as relevant to the head and neck and upper-aerodigestive system including its embryology, physiology, pharmacology, pathology, microbiology, biochemistry, genetics and immunology. Conduct essential componnts of the basic ear, nose, and throat physical exam and review of symptoms. Become competent in the otolaryngologic history and physical examination with particular emphasis on speech and swallow function. Understand and describe assessment procedures such as audiologic tests, electronystagmography, laryngoscopy, and videostroboscopy. Develop competency in the basic interpretation of plan X-ray and CT imaging of the nose, paranasal sinus and anterior/middle cranial fossa. Understand the blood supply of the nares and sinuses, define Kiesselbach’s plexus. Differentiate anterior and posterior bleeding and know the common sources of bleeding for each syndrome. Understand the common etiologies of epistaxis and list common risk factors and associated medical conditions. Understand the importance of the initial assessment, including the need for airway intervention, fluid resuscitation, and cardiovascular stability. Take a focused history and physical exam on a patient with epistaxis. Be comfortable with the initial management of epistaxis including use of medications and tamponade procedures, as well as obtaining intravenous access. List the treatment options for anterior bleeding (cautery, nasal packing, contralateral nares packing, thrombogenic foams and gels) and understand when to utilize each treatment method. List the treatment options for posterior bleeding. Recognize the common signs and symptoms in a patient suffering from stridor. Understand the causes of stridor. Describe and be proficient in establishing an emergency airway. Be able to do a focused history and physical Page 5 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives 27 Malignant lesions 28 Rhinitis, rhinorrhea, and nasal obstruction 29 Emergency care 30 Infections exam on a patient presenting with stridor. List the appropriate diagnostic testing necessary once a patient is stabilized. List the risk factors for developing cancer of the tongue, oral cavity, pharynx and larynx. Identify and describe common exam findings of the oral cavity and pharynx including malignant lesions and lesions resembling malignancy. Identify and describe common malignant and benign laryngeal problems in adults. Understand the pathophysiology of malignancy (Squamous Cell Carcinoma, Adenocarcinoma, Adenoid Cystic Cancer, Chondrosarcoma). List treatment options for the above listed malignancies. Recognize benign tumors like granular cell, chondroma, and papillomas. Define rhinitis and recognize the clinical symptoms (sneezing, rhinorrhea, nasal congestion, nasal itching). Recognize and describe common causes of rhinitis and rhinorrhea (allergic rhinitis, nonallergic rhinitis, occupational exposure, structural abnormalities that could lead to recurrent rhinitis or rhinorrhea). List treatment options for rhinorrhea and rhinitis. Recognize the common symptoms associated with nasal obstructions. List the common etiologies causing nasal obstruction. Based on history and physical exam, be able to form a thorough differential diagnosis and initiate proper treatment for nasal obstruction, rhinitis, and rhinorrhea. Be able to perform anterior rhinoscopy. Understand the role of CT scan in the assessment of sinus pathology. Describe and explain the work up and treatment of otolaryngologic emergencies such as airway obstruction, tracheotomy care, caustic ingestion, deep neck abscesses, and maxillofacial trauma. Develop competence in determining which patients require immediate surgical intervention and which can be initially managed conservatively or medically. Develop competence in basic emergency procedures, particularly those related to airway and bleeding: o Surgical procedures o Endoscopic procedures Be able to communicate your assessment and treatment strategy to an attending physician. Describe typical patient presentations of common infections such as acute sinusitis, pharyngitis, and acute suppurative otitis media and determine the best treatment options for each disease process. Page 6 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives 31 Tonsils and adenoids 32 Hoarseness and laryngitis 33 Tracheotomy and tracheostomy Diagnose and treat common infections of the ears, nose, and throat, particularly acute sinusitis, pharyngitis, and otitis media. Know the indications for paranasal sinus culture. Know how to perform paranasal sinus cultures and washout techniques. Understand bacterial resistance and list the contributing factors responsible for resistance development. List and understand the indications for a tonsillectomy in adults and children. List the common complications to tonsillectomy and adenoidectomy. Describe and understand the pharyngeal anatomy. Be able to perform a focused history and physical exam on a patient with special attention to examination of the tonsils and adenoids. Recognize the clinical and physical exam findings of a patient with a peritonsillar abscess and understand the surgical intervention. Become familiar with common signs and symptoms of hoarseness and laryngitis. List the common causes of laryngitis (reflux, allergic, autoimmune, infectious) both acute and chronic. Utilize a directed history and physical to properly diagnose someone with laryngitis/hoarseness. Understand the anatomy of the larynx including the hyoid bone, the nine laryngeal skeleton cartilages, extrinsic and intrinsic muscles as well as the blood and nerve supply of all vital structures in the region. Become competent in the diagnosis, assessment, and management of patients with voice disorders: o Spasmodic dysphonia (adductor vs. abductor) o Paradoxical voice cord movement o Parkinson’s Disease o Tremor Become competent in the diagnosis, assessment, and management of patients with laryngeal cancer. Know what kind of cancer is the most common, and how it metastasizes (direct spread, hematogenous, or lymphatic). List the indications for tracheotomy and tracheostomy. Be competent in performing a tracheotomy or tracheostomy. Understand the risks and complications of a tracheotomy/tracheostomy. List the important anatomy that the surgeon needs to recognize when doing a tracheotomy/tracheostomy. List the contraindications (both relative and absolute) to a tracheotomy/tracheostomy. Understand the post-operative care required Page 7 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives 34 Trauma 35 Swallowing disorders of a tracheostomy tube. Know the indications to change a tracheostomy tube. Understand how to change a tracheostomy tube. Know the characteristics of a patient who can be decannulated and be able to perform decannulation. Describe the priorities involved in treating patients with head and neck injuries. Describe the mechanical and structural properties of the facial skeleton as they relate to fracture patterns in facial trauma. Describe the concepts of primary bone healing, malunion, nonunion and osteomyelitis. Discuss the advantages and disadvantages of various techniques of treatment of facial fractures including: a. Non-operative treatment b. Closed reduction c. Mandibulomaxillary fixation d. Open reduction with and without fixations e. Intraoral splints f. External fixation g. Bone grafting Describe complications of facial fracture treatment (secondary deformities, infections/osteomyelitis, malocclusion, nonunions, malunions). Describe the neuroanatomy, cranial nerve anatomy and soft tissue anatomy pertinent to facial fractures. Recite the treatment of soft tissue injuries of the head and face including parotid gland and duct injuries, facial nerve injuries, and lacrimal apparatus injuries. Develop competence in determining which patients require immediate surgical intervention and master basic trauma procedures particularly those related to airway management: Be able to perform a cricothyroidotomy. Be able to interpret plain X-ray and CT images of the nose, paranasal sinuses, and anterior/middle cranial fossa in a trauma patent. Describe the treatment options, including surgical and non-surgical, for patients suffering from nasal fractures. Understand the basic science principles integral in swallowing. Recognize the clinical presentation of a patient with a swallowing disorder. Perform a directed history and physical in a patient complaining of dysphagia. Differentiate oropharyngeal dysphagia from esophageal dysphagia by history and physical exam. Recognize the difference between dysphagia with solid food and liquids and understand Page 8 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives # how this impacts your differential diagnosis. Become competent in the diagnosis, assessment and management of patients with swallowing disorders: a. Structural defects vs. functional deficits b. Zenker’s diverticulum c. Cricopharyngeal spasm d. Esophagitis/pharyngitis Surgical Skills کورس/مودل Dates Instructor Training Type نوع تریننگ 1 1 1 Appropriate tissue handling during surgery Blunt and sharp dissection 1 1 Vascular control in elective and critical situations Closure of simple wounds 1 1 1 1 10 Application of appropriate wound dressing Urethral catheter insertion 1 11 Insertion of a nasogastric tube 1 12 Tourniquet application 1 1 1 1 2 3 4 5 6 7 8 9 13 14 Incision with sharp and energy-based instruments Knot tying Suturing Appropriate use of drains Splint for bony injury or soft tissue injury Remove a superficial skin lesion 15 Drain a superficial abscess 1 16 Biopsy 1 1 1 Tube thoracostomy Needle Cricothyroidotomy Cricothyroidotomy or tracheostomy Preparation of specimen for a pathologist Appropriate wound surveillance and dressing care Insertion of a nasogastric tube 1 1 1 1 1 1 17 18 19 20 21 22 23 24 # Secure arterial and venous vascular access Needle thoracostomy ENT Skills Dates Instructor Training PGY Length PGY Length Page 9 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives Type نوع تریننگ Neck abscess drainiage Office and OR management of epistaxis Excision of simple masses in the neck Foreign body removal from nose and ear Nasal endoscopy and anterior rhinoscopy Flexible fiberoptic assessment of the airway Direct laryngoscopy/microlaryngoscopy Bronchoscopy Esophagoscopy Tracheostomy Tonsillectomy External fixation of mandibular fracture Submandibular gland excision Surgical neck exploration and aerodigestive tract repair in neck trauma Flap closure of persistent tracheostomy Caldwell Luc operation Mastoidectomy Endoscopic management of epistaxis 20 Office endoscopy of upper airway, biopsy, and debridements Internal fixation of maxillofacial fractures # Advanced ENT Skills 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Neck abscess drainage. Office and OR management of epistaxis. Excision of simple masses in the neck. Foreign body removal from nose and ear. Nasal endoscopy and anterior rhinoscopy Flexible fiberoptic assessment of the airway Direct laryngoscopy/microlaryngoscopy Bronchoscopy Esophagoscopy Tracheostomy Tonsillectomy External fixation of mandibular fractures (dental wiring). Submandibular gland excision Surgical neck exploration and aerodigestive tract repair in neck trauma. 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 1-5 Core topics completed مضامین که تکمیل شده 1-5 Instructor Training Type نوع تریننگ PGY5 2-5 2-5 2-5 2-5 3-5 3-5 3-5 3-5 3-5 3-5 3-5 3-5 4-5 4-5 Page 10 Length ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives 15 16 17 18 19 20 Flap closure of persistent tracheostomy Caldwell Luc operation Mastoidectomy Endoscopic management of epistaxis Office endoscopy of upper airway, biopsy, and debridements. Internal fixation of maxillofacial fractures Certification/Training تریننگ/ تصدیق نامه BLS 3 ACLS 4 ATLS 4-5 4-5 4-5 4-5 4-5 Certification of completion بدست آوردن شهادت نامه 2 1 4-5 Complete H&P Date(s) تاریخ Comments نظریات Obtain a detailed surgical history that is appropriate for age, sex and clinical problem. Obtain and review relevant medical records and reports. Obtain information from prior hospitalizations. Know the patient’s other physicians. Perform a detailed physical examination. Develop a focused differential diagnosis. Assess, document and manage perioperative risk factors. Document the treatment plan in the medical record, including indications for treatment. Page 11 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives Topic Skills مهارت های بخش مراقبت جدی Hospital Hygeine o o o o Handwashing asespsis antisepsis Lab 1 Lab 2 airway lines suturing fracture care. Admit orders, Pre-op note and orders Post-op note and orders Operation reports Transfer note & orders Discharge note & orders when appropriate when inappropriate Abdominal mass Aortic aneurysm Aortic dissection/rupture Appendicitis Atelectasis, lung contusion Bowel gas patterns (Large vs. small intestine, normal vs. abnormal vs. nonspecific) Diaphragm abnormalities Fractures Free air in abdomen Hemothorax, pneumothorax Lung mass, mediastinal nodes Paraesophageal hernia Pleural effusion Pneumonia Pulmonary embolism Pulmonary infiltrate Spinal column fractures Visceral abnormalities and injuries Pancreatitis, pancreatic tumor Bowel obstruction, ileus Spleen laceration, splenic infarct Hemoperitoneum, ascites Liver tumors,cysts,laceration, hematoma Biliary tree dilation, cholecystitis retroperitoneal hematoma, tumors Hernias: inguinal,femoral,umbilical and incisional colon tumors, diverticulitis, volvulus Renal, ureteric and bladder stones (calculi) o o o o o Central venous line Chest tube Endotracheal tube Nasogastric tube Trachestomy o 1 Computer skills o o 2 Skills Lab: o o o o 3 Documentation I: o o o 4 Documentation II: o o Consultation: o o o 5 6 o o o o o o o o o o o o o o o o o o o o o o o o o o Imaging I: Recognize abnormalities Instructor تعداد پروسیجرهای اجرا شده چند سال تجربه Evaluation dates PGY Year 7 Imaging II: Appropriate placement 8 Chest Tubes o Nasogastric and Oraltracheal o 9 10 Page 12 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives tubes Peripheral and Central lines o Urinary Catheters o 11 12 Medical Proficiency Evaluater 1 Perform a complete/appropriate assessment of pt 2 Perform a complete consultation 3 Ensure patients receive appropriate end-of-life care 4 Formulate and implement a management plan چند سال تجربهEvaluation dates Comments نظرات Demonstrate proficient and appropriate use of 5 procedural skills, indications, contraindications Surigcal ICU issues Core topics completed مضامین که تکمیل شده 1 Types of Shock 2 Catheters 3 Ventilation 4 Vasopressors 5 6 Blood Component therapies Transfusion 7 Criticaly ill complications 8 Nutrition Instructor Training Type نوع تریننگ PGY Anaphylactic Cardiogenic Hemorrhagic Neurogenic Septic venous and arterial catheters; interpret data, and direct therapy indication modes weaning medications indications indications indications minor and major transfusion reactions Aspiration Deep vein thrombosis Line sepsis Pressure ulcers Upper gastrointestinal bleeding Indications options See ICU objectives for more Page 13 Length ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives TOP 15 Must Know Surgical Issues o o o Abdominal pain – Acute abdomen: o o o o o o 1 o o Anorectal disease: o o o 2 o o o o Appendicitis: 3 o o o o o o o o Biliary tract disease: o o o o 4 Colon: 5 o o o o o Describe a systematic approach to the history in the assessment of the acute abdomen. Understand the different types of abdominal pain (visceral, parietal, referred); characterization of abdominal pain (onset, provocative, quality, radiation, site, symptoms of pain, time course). Outline the specific ways that the physical examination is different in the assessment of the acute abdomen than it is in the benign abdomen. Identify the immediate life threatening conditions of abdominal pain: Abdominal aortic aneurysm, mesenteric ischemia, perforation of gastrointestinal tract, acute bowel obstruction, volvulus, ectopic pregnancy, placental abruption, myocardial infarction, splenic rupture, hemoperitoneum and massive intraabdominal hemorrage List the differential diagnosis of localized tenderness in the epigastrium and each of the four abdominal quadrants. Describe the signs/symptoms, pathogenesis, diagnosis and management of the common causes of the acute abdomen. Describe the role of the peritoneum in intra-abdominal inflammatory processes. Describe the presentation and management of conditions that commonly present as an acute abdomen that do not require surgical therapy. State the etiological factors in the development of hemorrhoidal disease, including the roles of diet, pregnancy, and occupation. Describe the symptoms and physical findings of patients with internal and external hemorrhoids. Outline the principles of management of patients with symptomatic external hemorrhoids and symptomatic internal hemorrhoids. Outline the symptoms, physical findings of patients with perianal infections and pilonidal disease. Describe the symptoms and physical findings of patients with fissure-in-ano and outline the principles of management. Understand the pathogenesis of the inflammatory process of appendicitis. Identify the clinical manifestations of appendicitis. Be able to perform a careful physical examination. Know how to elicit the following signs: McBurney’s point, Rovsing’s, Psoas and Obturator signs. Obtain appropriate labs and radiologic studies to aide in diagnosis. Know the differential diagnosis of acute appendicitis. Understand the operative indications for appendicitis. Understand the medical and surgical management of appendicitis. List the complications of acute appendicitis if left untreated. List the common types of gallstones and describe the pathophysiology involved in their formation. Describe the signs and symptoms in a patient with biliary colic. Contrast these symptoms with those of acute cholecystitis. List the tests commonly used in the diagnosis of calculus biliary tract disease. Describe the indications for, limitations of, and potential complications of each test. List the complications which can occur from biliary calculi. Outline the medical and surgical management of a patient with acute cholecystitis. Describe the symptoms and signs of chloedocholithiaisis; describe the management of this problem. Compare and contrast the liver enzyme abnormalities in obstructive jaundice and viral hepatitis. List the most common bacteria found in cholecystitis and cholangitis. Discuss the risk factors for colorectal cancer. Identify the common symptoms of colorectal cancer. Discuss the evaluation and treatment of colorectal cancer. Discuss the role of radiotherapy and chemotherapy in management of patients with Page 14 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives o o o o o Cholelithiasis (Acute cholecystitis): o o o o o o o o o 6 o o Gastrointestinal bleeding: o o o o 7 o o o Hernias: o o o o o o o 8 Jaundice 9 o o o o o o o o o Liver cysts: 10 o colorectal cancer. Describe the clinical findings of diverticular disease, differentiating the symptoms and signs of uncomplicated and complicated diverticulitis. Discuss non-operative management of diverticular disease. Discuss operative therapy for diverticular disease i.e. uncomplicated and complicated. Differentiate ulcerative colitis and Crohn’s disease of the colon in terms of history, xray findings, prognosis and risk of cancer Define the following: Acute cholecystitis Acalculous cholecystitis Chronic cholecystitis Understand the pathogenesis of the inflammatory process of acute cholecystitis Identify the clinical manifestations of acute cholecystitis Perform a careful physical examination Know how to perform the Murphy’s sign Obtain appropriate labs and radiologic studies to aide in diagnosis Know the differential diagnosis of acute cholecystitis Understand the operative indications for acute cholecystitis Understand the medical and surgical management of acute cholecystitis List the complications of acute cholecystitis if left untreated Define hematemesis, hematochezia, melena, and guaiac positive stool; state their significance with regard to the level of the bleeding source. Outline the resuscitation plan for a hypotensive patient with a major GI hemorrhage. Given a patient with upper and lower GI hemorrhage, outline according to priority, the steps of assessment and initial management once resuscitation has been completed. In order of frequency, list the most common causes of upper and lower GI bleeding in the general population, in the adult (age 16 years and above), and in the infant (birth to 2 years). Outline the work-up of the adult patient presenting with occult blood on rectal exam. List criteria for surgical intervention in a patient with GI hemorrhage. Provide a definition of a hernia and understand the incidence of various types of hernias. Describe the epidemiology, pathogenesis and classification of hernias. Specifically, define the various locations of hernias on the abdominal wall. Understand the different types of hernias (reducible, incarcerated, strangulated, and sliding) at each anatomic site. Differentiate a direct, indirect, and femoral hernia of the groin and define the anatomic relationship between them. Describe the clinical manifestations of hernias based on location. Describe the abdominal and groin exam and the findings associated with the different types of hernias. Obtain appropriate labs and radiologic studies to aide in diagnosis. Know the differential diagnosis of hernias. Identify the types of hernia repair used for common abdominal wall hernias. Understand the potential complications of hernia repair. Describe the medical management of hernias based on location. Understand the anatomy and physiologic abnormalities of the different types of diaphragmatic and hiatal hernias. Define obstructive jaundice. Describe the pathophysiology of obstructive jaundice. List the causes of obstructive jaundice. Describe the clinical manifestations of obstructive jaundice. Know the differential diagnosis of jaundice. Understand the operative indications for obstructive jaundice. Understand the medical and surgical management of obstructive jaundice. List the complications of obstructive jaundice if left untreated. Know the classification of hepatic cysts with specific focus on Echinococcal (hydatid) cysts. Understand the pathogenesis of Echinococcal (hydatid) cysts: Page 15 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives o o o o o o o o o o Pancreatitis: o o o o o o o o o o 11 Peptic ulcer disease: o o o o o o o o o o o o o 12 Peritonitis: 13 o o o Life cycle and epidemiology of Echinococcus Know the four species of Echinococcus that cause infection in humans and the geographic distribution. Identify the clinical manifestations of Echinococcus not only in the liver but in the lung and other organs: Describe what symptoms occur with cyst rupture Perform a careful physical examination in a patient suspected of being infected with Echinococcus. Obtain appropriate labs and radiologic studies to aide in diagnosis. Know the differential diagnosis of liver cysts. Understand the operative indications for Echinococcal cysts. Understand the medical and surgical management of Echinococcal cysts: Specifically, know the various surgical techniques and the risks of each. Specifically, know the chemotherapy agents used to medically treat Echinococcus. List the complications of Echinococcal cysts if left untreated. Understand prevention of Echinococcal cysts. Define acute and chronic pancreatitis: Describe the differences between acute and chronic pancreatitis. Understand the etiology of acute and chronic pancreatitis. Describe the pathogenesis of acute and chronic pancreatitis. Describe the risk factors for acute and chronic pancreatitis. Identify the clinical manifestations of acute and chronic pancreatitis. Be able to perform a careful physical examination. Obtain appropriate labs and radiologic studies to aide in the diagnosis of pancreatitis. Know how to predict the severity and classification of acute pancreatitis: Know Ranson’s criteria Know Apache II score Know the differential diagnosis of acute and chronic pancreatitis. Understand the medical and surgical management of acute and chronic pancreatitis: Understand the different therapeutic approach between acute and chronic pancreatitis Understand the operative indications for acute and chronic pancreatitis and potential complication of surgery Understand the complications of acute and chronic pancreatitis if left untreated Define peptic ulcer disease. Understand the epidemiology and pathogenesis of peptic ulcer disease. Describe the risk factors for peptic ulcer disease. Identify the clinical manifestations of peptic ulcer disease. Be able to perform a careful physical examination. Obtain appropriate labs and radiologic studies to aide in diagnosis. Know the differential diagnosis of peptic ulcer disease. Understand the medical and surgical management of peptic ulcer disease. Understand the operative indications for peptic ulcer disease and potential complication of surgery. Understand the complications of peptic ulcer disease and the specific treatment for each: Bleeding Perforation Penetration Gastric outlet obstruction Define spontaneous bacterial peritonitis (SBP): Know the common organisms associated with SBP. Understand the pathogenesis of the spontaneous bacterial peritonitis (SBP). Know the risk factors of spontaneous bacterial peritonitis (SBP): Understand the clinical and laboratory features that are associated with an increased risk of spontaneous bacterial peritonitis (SBP). Identify the clinical manifestations of spontaneous bacterial peritonitis (SBP). Page 16 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives o o o o o o Small and Large Bowel Obstruction: 14 o o o Breast Disease: o o o o o o 15 Perform a careful physical examination. Obtain appropriate labs and radiologic studies to aide in diagnosis. Know the differential diagnosis of spontaneous bacterial peritonitis (SBP). Understand the medical management of spontaneous bacterial peritonitis (SBP): Specifically, understand prophylaxis therapy and indications in spontaneous bacterial peritonitis (SBP). List the complications of spontaneous bacterial peritonitis if left untreated. Know small and large bowel obstruction including pathogenesis, causes, risk factors, clinical manifestations, physical examination, lab and x-ray confirmation, differential diagnosis, operative indications for small and large bowel obstruction and medical and surgical management. Understand the pathogenesis of breast cancer. Recognize the common clinical manifestations of breast cancer (Lump, nipple discharge, lymph node enlargement). Develop a differential diagnosis for breast lumps and list the four major categories (fibroadenoma, fibrocystic disease, carcinoma). List four major risk factors for breast cancer. Complete a focused physical exam in a patient with suspected breast cancer. List the various labs and radiological studies required for full evaluation of a breast lump, including breast cancer screening guidelines. Be able to properly interpret a mammogram. Understand the operative indications when evaluating a breast lump/mass. Master the various surgical techniques: lumpectomy, mastectomy, radical mastectomy, sentinel lymph node dissection. Page 17 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ENT core objectives – Please see resident manual for off-service objectives ENT Resident Expectations توقوعات از دوکتوران دوره تخصص PGY-1 schedule General orientation: 1 month Orthopedic/trauma surgery: 2 months General surgery: 1 month ENT surgery: 1 month Vascular/thoracic surgery: 1 month Plastic surgery/burn care: 1 month Critical care: 1 month Emergency: 1 month Radiology: 1 month Exam: 1 month PGY-1 Skills During the first year of the Otolaryngology residency program, residents will take a common year of instruction with their peers from the General Surgery, Urology and Orthopedic Surgery residency programs. This year of training is known as the Foundations of Surgery Program. The resident will attend all surgery required lectures and conferences. While the resident will administratively fall under the Otolaryngology Program Director, evaluations and rotation assessments will be completed by the directors of each specific rotation. The purpose of the first year is to provide the resident with a foundation of surgical knowledge and basic surgical technique. Please refer to the Foundations of Surgery program for a description of the course PGY-2 schedule Head and Neck service: 4 months Rhinology, otology, facial plastics: 3 months Pediatric ENT: 3 months Radiology CT: 1 month Exam: 1 month PGY-2 skills Develop enhanced proficiency in the provision of pre-operative and post-operative care Establisk a knowledge base and skill proficiency for the management of the critically ill surgical patient Increased skill in operative technique required for procedures of increasing surgical complexity Formulate plans of care based on acquired information Understand decision making processes used in the care of surgical patients Develop a post-operative plan of care Develop knowledge and skills necessary to function as the trauma team leader Provide house coverage for consultations and emergency room admissions PGY-3 schedule Head and neck service: 2 months Rhinology, otology, facial plastics: 2 months Laryngology: 2 months Radiology MRI: 1 month Neurotology: 2 months Research: 2 months Exam: 1 month PGY-4 schedule Head and neck service: 3 months ENT subspecialties: Rhinology, otology, facial plastics: 3 months Pediatric ENT: 3 months Research: 2 months Exam: 1 month PGY-5 schedule Head and neck service chief: 3 months Rhinology, otology, facial plastics chief: 3 months Neurotology chief: 3 months Research chief: 2 months Exam/MoPH monograph: 1 month of instruction. PGY-3 skills Continue to develop technical skills necessary for the performance of more complex surgical procedures in general surgery. Establish a knowledge base, judgment and interpersonal skills necessary to function as a surgical consultant. Teach junior residents in the emergency room, wards, and operating room. Competently manage a house-staff team in the peri-operative care of the patient. Work with the attending physician on development of post-operative plan. Master the details of pre-operative preparation of a hospitalized patient or an outpatient. Demonstrate the personal and professional responsibility, leadership skills, and interpersonal skills necessary for independent practice as a ENT Surgeon. PGY-4 skills Master technical skills necessary for the performance of more complex surgical procedures in general surgery. Provide clinical and administrative leadership for residents and students assigned to surgical services. Act as a mentor for junior surgical residents. Learn more advanced surgical techniques. PGY-5 skills Continue to master technical skills necessary for the performance of all surgeries. Achieve the full competence (including knowledge, skills, and attitudes) of a board eligible surgeon. Function as faculty. Page 18