Ortho Core objectives
advertisement

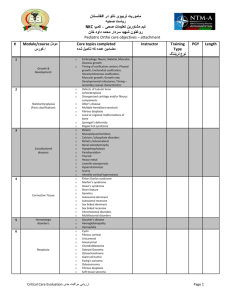
ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives # Module/course مودل کورس/ Core topics completed مضامین عمده که تکمیل شده 1 Anatomy Musculoskeletal Basic Anatomy relevant to orthopedics 2 Respiratory physiology 3 Fluid/electrolyte physiology lung volumes - flow rates – pressures; oxygen transport Understand fluid status in your patient with close attention during the operative and post-operative period. osmotic and volume regulation; sodium (Na), potassium (K), calcium (Ca), phosphorus (P) and magnesium (Mg) metabolism; regulation of acid-base Appropriately manage preoperative and postoperative fluid requirements Diagnose and manage common causes of airway obstruction in the surgical patient. Describe indications for and be able to perform orotracheal intubation. Describe the appropriate level of intraoperative monitoring for a given patient. Of Sepsis Transplant (optional) metabolic needs; caloric-protein-lipid requirements; fluids and micronutrients; adaptation to starvation as compared to response to surgical stress; body response to surgical stress including catabolic response and the need for metabolic support; enteral and parenteral feeding (indications, complications and benefits of nutritional support); 4 Airway management 5 Immunology 6 Nutrition 7 Sepsis and the inflammatory response metabolic and hemodynamic patterns Recognize the high mortality associated with sepsis. Define criteria for diagnosis of sepsis and SIRS. Appreciate the key aspects of management of sepsis including early goal directed therapy, proper antibiotic coverage, and appropriate surgical intervention (abscess, prosthesis). organ systems and surgical management; Hemodynamics Coronary Artery Disease (CAD); Valvular disease; Cardiomyopathy; Cardiac arrest, arrhythmias (as per ACLS protocols); Chronic Obstructive Lung Disease (COPD); Diabetes; Thyroid pathophysiology; 9 Impact of age, pregnancy, obesity, sepsis, and stress Cardiac 10 Pulmonary 11 Endocrine 8 Ortho Instructor Training Type نوع تریننگ PGY Page 1 Length ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives 12 Renal 13 Hepatic 14 Hematologic 15 Risk assessment strategies and scores 16 Diagnostic modalities and radiation safety 17 Medical treatments and their impact on surgery (Optional) Parathyroid pathophysiology; Adrenal pathophysiology; Renal failure Cirrhosis Liver failure Screening for diatheses Hypocoagulable states Hypercoagulable states anesthetic risks cardiac risks ICU risk scores trauma assessment including GCS nutritional assessment preoperative screening tests and their limitations. plain radiography; ultrasound; CT scan; MRI technology; fluoroscopy immunosuppression; cancer chemotherapy; radiotherapy; common drugs with impact on hemostatic function and how to correct their impact; tribal customary medicine (alternative medicine); blood products (types, indications and adverse reactions). purpose and basis of staging; basic principles of neoplastic transformation including tumor growth and spread; pathology requirements for appropriate assessments; definition of common pathological terms such as but not limited to neoplasia, malignancy, dysplasia, metaplasia and atypia; genetics of neoplasia and families at risk; environmental carcinogens; paraneoplastic syndromes; principles of multi-modality therapy. community and hospital acquired bacteria, fungi and viruses; impact of blood borne pathogens, including HIV, Hepatitis B and Hepatitis C. Describe the differences of healing by primary closure, by delayed primary closure and by secondary intention, and the indications for each. Recognize the various phases of wound healing and the approximate time course associated with each phase. Describe the significance of epithelialization and defense against contamination. Describe clinical factors that may retard healing. Recognize and differentiate wounds, which have resulted in a loss of tissue and those, which have not. 18 Cancer Care (Optional) 19 Management of common infections 20 Wound healing Ortho Page 2 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives 21 Principles of prophylaxis 22 Principles of anesthesia 23 Transplant/Implant 24 Complications in the surgical patient Ortho Recognize and differentiate clean vs. infected wounds; which can be safely closed primarily and those which cannot. Describe the functions of a dressing. Contrast “dehiscence” and “evisceration” and describe their presentation and management. Assess a wound for signs of infection, attending to the local heat, erythema, and excessive pain; outline the management of an infected surgical wound. Describe the factors that lead to non-healing chronic wounds. Describe factors that lead to pressure ulcers and treatment. wound and systemic infection thromboembolism (DVT, PE) tetanus. local anesthetic agents, indications, contraindications and administration; regional anesthetics; general anesthetics; procedural sedation, indications, contraindications and administration; complications arising from the administration of anesthesia. Describe the complications of and be able to order appropriately: O Barbiturates O Local anesthetics O Neuromuscular blockade reversal agents O Neuromuscular blockers O Sedatives Describe the role and indications for use of epinephrine in local anesthesia. Transplantation: description of grafts (autograft, xenograft, allograft) rejection (hyperacute, acute cellular and chronic). Implantation: principles of compatibility, biological reaction/rejection. cardiac (principles of advanced cardiac life support); shock; multiple organ dysfunction syndrome; respiratory failure (mechanical ventilation); stress gastritis; postoperative ileus; fat embolism; Infections: -spreading and necrotizing infections - clostridium difficile; - methicillin-resistant Staph. aureus; - vancomycin-resistant Enterococci; -common pathogens. compartment syndromes (limb, abdomen); pressure sores; delirium (psychiatric disorders); stroke; Page 3 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives Pre and Post-operative care 25 Assessment of basic diagnostic radiographs (See Imaging I-II skills) 26 Pre and Post-operative care in Orthopedics 27 Orthopedic procedures 28 Musculoskeletal infections Ortho brain death Pre-operative evaluation Discuss the pre-operative assessment of trauma, endoscopic, and open surgery patients. Post operative management: Discuss prevention of peri-operative cardiac events. Discuss proper fluid management and appropriate use of blood products in the postoperative patient. Discuss the causes of postoperative fever. Discuss the differential diagnoses for patients with postoperative respiratory difficulty. Understand how to manage post-operative pain. Be able to adequately order and properly interpret the following tests: Conventional bone x-rays Fluoroscopy Understand the indications, contraindications and risks of the following procedures. Be able to properly order them when indicated and to discuss the implications of the findings of each: Computed tomography CT) MRI Understand the principles of pre and post-op care for common orthopedic problems and be able to demonstrate to the satisfaction of the orthopedic staff. Knowledge of the common postoperative complications and the management of these complications to include: Wound, joint, soft tissues and implanted material infection Abnormal bleeding Deep venous thrombosis, pulmonary embolism Fat embolism Pressure sores Joint ankylosis Compartment syndromes Understand the indications, risks, and alternatives of these typical orthopedic procedures, and gain experience as available, under direct supervision: Splinting and taping of common injuries Application of traction Casting and cast management Open reduction and fixation of fractures Arthrocentesis Injection of steroids External fixation device placement and management Osteomyelitis; septic arthritis; Mycobacterium Tuberculosis of the spine/arthritis: Describe the epidemiology and risk factors for these infections. Understand the relevant anatomy based on location of infection. Describe the pathophysiology of infection Page 4 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives 29 Biceps tendinopathy and tendon rupture: o Acute treatment o Physical therapy Clavicle fractures: o Describe the classification and location of clavicle fractures: Group I Group II Group III Frozen shoulder (adhesive capsulitis): o Acute treatment o Physical therapy o Subacromial injection and intraarticular dilation (hydroplasty) Glenohumeral osteoarthritis: o Acute treatment o Physical therapy o Glenohumeral joint injection Rotator cuff tendinopathy and tears: o Differentiate rotator cuff tendinopathy versus rotator cuff tears: Acute treatment to include adjunct therapy Physical therapy Subacromial injection Shoulder Ortho based on the type. Discuss the differential diagnosis of these infections. Discuss the clinical presentation of these infections. Perform a thorough physical examination. Order the appropriate laboratory and radiology studies and be able to adequately interpret. Understand the medical management for each of these infections. Understand the indications for surgical management. Describe appropriate follow-up care and complications if left untreated. Acromioclavicular (AC) Joint Injuries: o Type I AC joint injury o Type II AC joint injury o Type III AC joint injury o Type IV AC joint injury o Type V AC joint injury o Type VI AC joint injury Shoulder dislocations: o Anterior shoulder dislocation o Posterior shoulder dislocation o Inferior shoulder dislocation o Immobilization o Operative treatment o Rehabilitation o Patient education Page 5 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives Shoulder impingement: o Acute treatment o Physical therapy o Subacromial injection Superior labral anterior-posterior (SLAP) lesion Special tests for the shoulder: Understand the indications; be able to perform and interpret the following physical exam maneuvers: o o o o o o o o o o o Apley scratch test Apprehension test Cross arm test Drop arm test Empty can test Hawkin’s test Neer test Push off test Speed’s Maneuver Spurling test Subacromial impingement o Sulcus sign o Yergason Test Carpal Tunnel Syndrome: Acute therapy Wrist splinting Physical therapy Glucocorticoid injection DeQuervain’s Tenosynovitis: Acute therapy Thumb and Wrist splinting Glucocorticoid injection Ganglion Cyst: Aspiration and glucocorticoid injection. Understand the indications for surgical management. 30 Kienbock’s Disease: Lichtman’s modification of Stahl’s classification of plain radiographs. Fractures of carpal (scaphoid, lunate) and wrist (radius, ulnar) bones: Understand perilunate and scapholunate dislocations. Understand scapholunate advanced collapse (SLAC) and scaphoid non-union advanced collapse (SNAC). Upper extremity: hand and wrist Ortho Metacarpal and phalanges fracture Osteoarthritis of hands Radial Tunnel Syndrome Rheumatoid Arthritis Page 6 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives Trigger finger (stenosing flexor tenosynovitis): Acute therapy Immobilization Physical therapy Glucocorticoid injection 31 Upper extremity: elbow 32 Lower extremity: hip 33 Lower extremity: knee Ortho Ulnar Nerve Entrapment Special tests for the hand and wrist: o Durkan carpal compression test o Finkelstein’s test o Froment’s sign o Grind test o Lunotriquetral shear test o McMurray’s test o Phalen maneuver o 1. Scaphoid compression and shift test o 2. Supination lift test o 3. Tinel’s sign o 4. Watson’s test Elbow dislocation: Lateral and medial epicondylitis Ligamentous injuries Medial collateral ligament Lateral collateral ligament Nerve entrapment Medial nerve entrapment Radial nerve entrapment Ulnar nerve entrapment Nursemaid’s elbow (Radial head subluxation) Olecranon bursitis Special tests for the elbow: Valgus and Varus test Avascular necrosis of the hip (osteonecrosis) Femur fracture (proximal) and femoral neck fracture Iliopsoas Tendinitis Labral tear Pelvic fracture Osteoarthritis of the hip Slipped Capital Femoral Epiphysis (SCFE) Trochanteric bursitis Glucocorticoid injection Special tests for the Hip: o Faber or Patrick Test o Piriformis syndrome o Thomas Test o Trendelenburg test Avascular necrosis of the femoral condyle (osteonecrosis) Bursitis of knee Fractures of lower extremity (distal femur, patella, tibial plateau) Iliotibial band syndrome Knee dislocations (Tibiofemoral) Ligamentous tears of the knee: Anterior Cruciate ligament tears Posterior Cruciate ligament tear Page 7 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives Medical collateral ligament injury Lateral collateral ligament injury Medial meniscal tear Osteoarthritis of the knee Osteochondritis Dissecans of knee and ankle Patellofemoral Pain syndrome Popliteal cyst Patellar tendinitis Special Tests for the knee: o Anterior and posterior drawer test o Lachman test o McMurray’s test o Noble’s test o Ober’s test o McMurray’s test o Thumb sign o Valgus and Varus stress test o Wilson’s test Achilles tendinopathy and rupture Ankle Sprain/fracture Freiberg’s disease Hallux Valgus Jones’s Fracture Plantar Fasciitis Retrocalcaneal bursitis Tarsal tunnel syndrome Special tests for ankle and foot: o Anterior and drawer test o External rotation test o Inversion test o Neuroma test o Ottawa Ankle rule o Talar tilt o Thompson’s test Cervical Radiculopathy Cervical Spine Fracture Cervical Spondylosis Diffuse Idiopathic Skeletal Hyperostosis (DISH) Thoracic Outlet Syndrome Special Tests for the neck o Spurling test o Waddell’s sign o Inversion test o Neuroma test o Ottawa Ankle rule o Talar tilt o Thompson’s test Ankylosing Spondylitis (AS) Back Strain Cauda Equina Syndrome Compression fracture Disk herniation (Lumbar Radiculopathy) Osteoarthritis of spine Spinal Infection Spondylolisthesis and Spondylolysis Special Tests for the Spine: o Nerve roots and their action o Straight leg sign 34 Lower extremity: ankle and foot 35 Neck 36 Spine Ortho Page 8 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives Waddell’s sign Surgical Skills کورس/مودل # 1 Conduct of a surgical procedure Dates 2 Incision with sharp and energy-based instruments Knot tying Instructor Training Type نوع تریننگ PGY principles of patient safety; principles of management of patient and surgical team with respect to blood borne pathogens (needle stick injury, mucosal exposure, cautery smoke); cautery and emerging energy sources; procedure planning (appropriate instruments and supplies); calling for help. 1 1 1 Appropriate tissue handling during surgery Blunt and sharp dissection 1 1 Vascular control in elective and critical situations Closure of simple wounds 1 1 1 1 11 Application of appropriate wound dressing Urethral catheter insertion 1 12 Insertion of a nasogastric tube 1 13 Tourniquet application 1 1 1 3 4 5 6 7 8 9 10 14 15 Suturing Appropriate use of drains Splint for bony injury or soft tissue injury Remove a superficial skin lesion 16 Drain a superficial abscess 1 17 Biopsy 1 1 1 Tube thoracostomy Needle Cricothyroidotomy Cricothyroidotomy or tracheostomy 1 1 1 1 18 19 20 21 22 23 Secure arterial and venous vascular access Needle thoracostomy Preparation of specimen for a pathologist Ortho Page 9 Length ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives 24 25 # Appropriate wound surveillance and dressing care Insertion of a nasogastric tube Orthopedic Surgical Skills 1 2 3 4 5 6 7 8 9 10 11 12 Instructor Training Type نوع تریننگ PGY 1-5 1-5 Simple casting and cast management Splinting and taping of common injuries Application of traction Closed reduction and stabilization of fractures Compartment release upper and lower limb 1-5 1-5 1-5 1-5 1-5 4-5 Arthrocentesis Open reduction and fixation of fractures Arthroplasty Spine surgery 4-5 4-5 4-5 4-5 1 Types of Shock 2 Catheters 3 Ventilation 4 Vasopressors 5 Blood Component therapies 7 1 Dates Evaluation and assessment of patients with orthopedic disease and thorough physical exam Understand indications and risks of and alternatives to typical orthopedic procedures Basic Fracture care Surigcal ICU issues 6 1 Transfusion Criticaly ill complications Ortho Core topics completed مضامین که تکمیل شده Anaphylactic Cardiogenic Hemorrhagic Neurogenic Septic venous and arterial catheters; interpret data, and direct therapy indication modes weaning medications indications indications indications minor and major transfusion reactions Aspiration Deep vein thrombosis Line sepsis Pressure ulcers Upper gastrointestinal bleeding Instructor Training Type نوع تریننگ PGY Page 10 Length Length ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives 8 Nutrition Indications options See ICU objectives for more Certification/Training تریننگ/ تصدیق نامه Certification of completion بدست آوردن شهادت نامه Complete H&P 1 2 BLS 3 ACLS 4 ATLS Topic Skills مهارت های بخش مراقبت جدی Hospital Hygeine o o o 1 Computer skills o o 2 Skills Lab: o o o o 3 Documentation I: o o o 4 Ortho Date(s) تاریخ Comments نظریات Obtain a detailed surgical history that is appropriate for age, sex and clinical problem. Obtain and review relevant medical records and reports. Obtain information from prior hospitalizations. Know the patient’s other physicians. Perform a detailed physical examination. Develop a focused differential diagnosis. Assess, document and manage perioperative risk factors. Document the treatment plan in the medical record, including indications for treatment. Instructor تعداد پروسیجرهای اجرا شده چند سال تجربه Evaluation dates PGY Year Handwashing asespsis antisepsis Lab 1 Lab 2 airway lines suturing fracture care. Admit orders, Pre-op note and orders Post-op note and orders Page 11 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives Documentation II: o o Consultation: o o o 5 6 o o Operation reports Transfer note & orders Discharge note & orders when appropriate when inappropriate Abdominal mass Aortic aneurysm Aortic dissection/rupture Appendicitis Atelectasis, lung contusion Bowel gas patterns (Large vs. small intestine, normal vs. abnormal vs. nonspecific) Diaphragm abnormalities Fractures Free air in abdomen Hemothorax, pneumothorax Lung mass, mediastinal nodes Paraesophageal hernia Pleural effusion Pneumonia Pulmonary embolism Pulmonary infiltrate Spinal column fractures Visceral abnormalities and injuries Pancreatitis, pancreatic tumor Bowel obstruction, ileus Spleen laceration, splenic infarct Hemoperitoneum, ascites Liver tumors,cysts,laceration, hematoma Biliary tree dilation, cholecystitis retroperitoneal hematoma, tumors Hernias: inguinal,femoral,umbilical and incisional colon tumors, diverticulitis, volvulus Renal, ureteric and bladder stones (calculi) o o o o o Central venous line Chest tube Endotracheal tube Nasogastric tube Trachestomy o o o o o o o o o o o o o o o o o o o o o o o o o o Imaging I: Recognize abnormalities 7 Imaging II: Appropriate placement 8 Chest Tubes o 9 Nasogastric and Oraltracheal tubes o Peripheral and Central lines o Urinary Catheters o 10 11 12 Ortho Page 12 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives Medical Proficiency Evaluater 1 Perform a complete/appropriate assessment of pt 2 Perform a complete consultation 3 Ensure patients receive appropriate end-of-life care 4 Formulate and implement a management plan چند سال تجربهEvaluation dates Comments نظرات Demonstrate proficient and appropriate use of 5 procedural skills, indications, contraindications TOP 15 Must Know Surgical Issues o o o Abdominal pain – Acute abdomen: o o o o o o 1 o o Anorectal disease: o o o 2 Appendicitis: o o o o o o o 3 Ortho Describe a systematic approach to the history in the assessment of the acute abdomen. Understand the different types of abdominal pain (visceral, parietal, referred); characterization of abdominal pain (onset, provocative, quality, radiation, site, symptoms of pain, time course). Outline the specific ways that the physical examination is different in the assessment of the acute abdomen than it is in the benign abdomen. Identify the immediate life threatening conditions of abdominal pain: Abdominal aortic aneurysm, mesenteric ischemia, perforation of gastrointestinal tract, acute bowel obstruction, volvulus, ectopic pregnancy, placental abruption, myocardial infarction, splenic rupture, hemoperitoneum and massive intraabdominal hemorrage List the differential diagnosis of localized tenderness in the epigastrium and each of the four abdominal quadrants. Describe the signs/symptoms, pathogenesis, diagnosis and management of the common causes of the acute abdomen. Describe the role of the peritoneum in intra-abdominal inflammatory processes. Describe the presentation and management of conditions that commonly present as an acute abdomen that do not require surgical therapy. State the etiological factors in the development of hemorrhoidal disease, including the roles of diet, pregnancy, and occupation. Describe the symptoms and physical findings of patients with internal and external hemorrhoids. Outline the principles of management of patients with symptomatic external hemorrhoids and symptomatic internal hemorrhoids. Outline the symptoms, physical findings of patients with perianal infections and pilonidal disease. Describe the symptoms and physical findings of patients with fissure-in-ano and outline the principles of management. Understand the pathogenesis of the inflammatory process of appendicitis. Identify the clinical manifestations of appendicitis. Be able to perform a careful physical examination. Know how to elicit the following signs: McBurney’s point, Rovsing’s, Psoas and Obturator signs. Obtain appropriate labs and radiologic studies to aide in diagnosis. Know the differential diagnosis of acute appendicitis. Understand the operative indications for appendicitis. Page 13 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives o o o o o Biliary tract disease: o o o o o o o o o 4 Colon: o o o o 5 o Cholelithiasis (Acute cholecystitis): o o o o o o o o o 6 o o Gastrointestinal bleeding: o o o o o o 7 Hernias: o o o 8 Ortho Understand the medical and surgical management of appendicitis. List the complications of acute appendicitis if left untreated. List the common types of gallstones and describe the pathophysiology involved in their formation. Describe the signs and symptoms in a patient with biliary colic. Contrast these symptoms with those of acute cholecystitis. List the tests commonly used in the diagnosis of calculus biliary tract disease. Describe the indications for, limitations of, and potential complications of each test. List the complications which can occur from biliary calculi. Outline the medical and surgical management of a patient with acute cholecystitis. Describe the symptoms and signs of chloedocholithiaisis; describe the management of this problem. Compare and contrast the liver enzyme abnormalities in obstructive jaundice and viral hepatitis. List the most common bacteria found in cholecystitis and cholangitis. Discuss the risk factors for colorectal cancer. Identify the common symptoms of colorectal cancer. Discuss the evaluation and treatment of colorectal cancer. Discuss the role of radiotherapy and chemotherapy in management of patients with colorectal cancer. Describe the clinical findings of diverticular disease, differentiating the symptoms and signs of uncomplicated and complicated diverticulitis. Discuss non-operative management of diverticular disease. Discuss operative therapy for diverticular disease i.e. uncomplicated and complicated. Differentiate ulcerative colitis and Crohn’s disease of the colon in terms of history, x-ray findings, prognosis and risk of cancer Define the following: Acute cholecystitis Acalculous cholecystitis Chronic cholecystitis Understand the pathogenesis of the inflammatory process of acute cholecystitis Identify the clinical manifestations of acute cholecystitis Perform a careful physical examination Know how to perform the Murphy’s sign Obtain appropriate labs and radiologic studies to aide in diagnosis Know the differential diagnosis of acute cholecystitis Understand the operative indications for acute cholecystitis Understand the medical and surgical management of acute cholecystitis List the complications of acute cholecystitis if left untreated Define hematemesis, hematochezia, melena, and guaiac positive stool; state their significance with regard to the level of the bleeding source. Outline the resuscitation plan for a hypotensive patient with a major GI hemorrhage. Given a patient with upper and lower GI hemorrhage, outline according to priority, the steps of assessment and initial management once resuscitation has been completed. In order of frequency, list the most common causes of upper and lower GI bleeding in the general population, in the adult (age 16 years and above), and in the infant (birth to 2 years). Outline the work-up of the adult patient presenting with occult blood on rectal exam. List criteria for surgical intervention in a patient with GI hemorrhage. Provide a definition of a hernia and understand the incidence of various types of hernias. Describe the epidemiology, pathogenesis and classification of hernias. Specifically, define the various locations of hernias on the abdominal wall. Understand the different types of hernias (reducible, incarcerated, strangulated, and sliding) at each anatomic site. Differentiate a direct, indirect, and femoral hernia of the groin and define the anatomic relationship between them. Describe the clinical manifestations of hernias based on location. Describe the abdominal and groin exam and the findings associated with the different types of hernias. Page 14 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives o o o o o Jaundice 9 o o o o o o o o o o o o o Liver cysts: o o o o o o o 10 Pancreatitis: o o o o o o o o o o 11 Peptic ulcer disease: 12 Ortho o o o o o o Obtain appropriate labs and radiologic studies to aide in diagnosis. Know the differential diagnosis of hernias. Identify the types of hernia repair used for common abdominal wall hernias. Understand the potential complications of hernia repair. Describe the medical management of hernias based on location. Understand the anatomy and physiologic abnormalities of the different types of diaphragmatic and hiatal hernias. Define obstructive jaundice. Describe the pathophysiology of obstructive jaundice. List the causes of obstructive jaundice. Describe the clinical manifestations of obstructive jaundice. Know the differential diagnosis of jaundice. Understand the operative indications for obstructive jaundice. Understand the medical and surgical management of obstructive jaundice. List the complications of obstructive jaundice if left untreated. Know the classification of hepatic cysts with specific focus on Echinococcal (hydatid) cysts. Understand the pathogenesis of Echinococcal (hydatid) cysts: Life cycle and epidemiology of Echinococcus Know the four species of Echinococcus that cause infection in humans and the geographic distribution. Identify the clinical manifestations of Echinococcus not only in the liver but in the lung and other organs: Describe what symptoms occur with cyst rupture Perform a careful physical examination in a patient suspected of being infected with Echinococcus. Obtain appropriate labs and radiologic studies to aide in diagnosis. Know the differential diagnosis of liver cysts. Understand the operative indications for Echinococcal cysts. Understand the medical and surgical management of Echinococcal cysts: Specifically, know the various surgical techniques and the risks of each. Specifically, know the chemotherapy agents used to medically treat Echinococcus. List the complications of Echinococcal cysts if left untreated. Understand prevention of Echinococcal cysts. Define acute and chronic pancreatitis: Describe the differences between acute and chronic pancreatitis. Understand the etiology of acute and chronic pancreatitis. Describe the pathogenesis of acute and chronic pancreatitis. Describe the risk factors for acute and chronic pancreatitis. Identify the clinical manifestations of acute and chronic pancreatitis. Be able to perform a careful physical examination. Obtain appropriate labs and radiologic studies to aide in the diagnosis of pancreatitis. Know how to predict the severity and classification of acute pancreatitis: Know Ranson’s criteria Know Apache II score Know the differential diagnosis of acute and chronic pancreatitis. Understand the medical and surgical management of acute and chronic pancreatitis: Understand the different therapeutic approach between acute and chronic pancreatitis Understand the operative indications for acute and chronic pancreatitis and potential complication of surgery Understand the complications of acute and chronic pancreatitis if left untreated Define peptic ulcer disease. Understand the epidemiology and pathogenesis of peptic ulcer disease. Describe the risk factors for peptic ulcer disease. Identify the clinical manifestations of peptic ulcer disease. Be able to perform a careful physical examination. Page 15 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives o o o o o o o o o Peritonitis: o o o o o o o 13 Small and Large Bowel Obstruction: 14 o o o Breast Disease: o o o o o o 15 Ortho Obtain appropriate labs and radiologic studies to aide in diagnosis. Know the differential diagnosis of peptic ulcer disease. Understand the medical and surgical management of peptic ulcer disease. Understand the operative indications for peptic ulcer disease and potential complication of surgery. Understand the complications of peptic ulcer disease and the specific treatment for each: Bleeding Perforation Penetration Gastric outlet obstruction Define spontaneous bacterial peritonitis (SBP): Know the common organisms associated with SBP. Understand the pathogenesis of the spontaneous bacterial peritonitis (SBP). Know the risk factors of spontaneous bacterial peritonitis (SBP): Understand the clinical and laboratory features that are associated with an increased risk of spontaneous bacterial peritonitis (SBP). Identify the clinical manifestations of spontaneous bacterial peritonitis (SBP). Perform a careful physical examination. Obtain appropriate labs and radiologic studies to aide in diagnosis. Know the differential diagnosis of spontaneous bacterial peritonitis (SBP). Understand the medical management of spontaneous bacterial peritonitis (SBP): Specifically, understand prophylaxis therapy and indications in spontaneous bacterial peritonitis (SBP). List the complications of spontaneous bacterial peritonitis if left untreated. Know small and large bowel obstruction including pathogenesis, causes, risk factors, clinical manifestations, physical examination, lab and x-ray confirmation, differential diagnosis, operative indications for small and large bowel obstruction and medical and surgical management. Understand the pathogenesis of breast cancer. Recognize the common clinical manifestations of breast cancer (Lump, nipple discharge, lymph node enlargement). Develop a differential diagnosis for breast lumps and list the four major categories (fibroadenoma, fibrocystic disease, carcinoma). List four major risk factors for breast cancer. Complete a focused physical exam in a patient with suspected breast cancer. List the various labs and radiological studies required for full evaluation of a breast lump, including breast cancer screening guidelines. Be able to properly interpret a mammogram. Understand the operative indications when evaluating a breast lump/mass. Master the various surgical techniques: lumpectomy, mastectomy, radical mastectomy, sentinel lymph node dissection. Page 16 ماموریت تربیوی ناتو در افغانستان ریاست صحیه NKC تیم مشاورین تعلیمات صحی – کمپ روغتون شهید سردار محمد داود خان ORTHO core objectives – Please see resident manual for off-service objectives Ortho Resident Expectations توقوعات از دوکتوران دوره تخصص PGY-1 schedule General orientation: 1 month Orthopedic/trauma surgery: 2 months General surgery: 1 month ENT surgery: 1 month Vascular/thoracic surgery: 1 month Plastic surgery/burn care: 1 month Critical care: 1 month Emergency: 1 month Radiology: 1 month Exam: 1 month PGY-1 Skills During the first year of the Urology residency program, residents will take a common year of instruction with their peers from the Otolaryngology, Orthopedic and General Surgery residency programs. This year of training is known as the Foundations of Surgery Program. The resident will attend all surgery required lectures and conferences. While the resident will administratively fall under the Urology Program Director, evaluations and rotation assessments will be completed by the directors of each specific rotation. The purpose of the first year is to provide the resident with a foundation of surgical knowledge and basic surgical technique. Please refer to the Foundations of Surgery program for a description of the course of instruction. PGY-2 schedule Pediatric orthopedics: 2 months Traumatology: 3 months Critical Care: 1 month General surgery: 2 months Radiology: 1 month Orthopedic techniques: 1 month Plastic surgery/burn care: 1 month Exam: 1 month PGY-2 skills Develop enhanced proficiency in the provision of pre-operative and post-operative care Establisk a knowledge base and skill proficiency for the management of the critically ill surgical patient Increased skill in operative technique required for procedures of increasing surgical complexity Formulate plans of care based on acquired information Understand decision making processes used in the care of surgical patients Develop a post-operative plan of care Develop knowledge and skills necessary to function as the trauma team leader Provide house coverage for consultations and emergency room admissions PGY-3 schedule Neurosurgery: 2 months Ortho/soft tissue/sport: 2 months Physiotherapy: 1 month Vascular surgery: 1 month Radiology: 1 month Orthopedic hand surgery: 2 months Orthopedic foot surgery: 2 months Exam: 1 month PGY-4 schedule Neurosurgery: 2 months Ortho infection/tumour: 2 months Amputation/rehabilitation: 2 months Ortho complex reconstruction: 3 months Elective surgery: 2 months Exam: 1 month PGY-5 schedule Orthopedic surgery (chief resident): 2 months Pediatric orthopedic surgery (chief resident): 2 months Traumatology (chief resident): 2 months Elective surgery/research: 2 months Exam/MoPH monograph: 4 months Ortho PGY-3 skills Continue to develop technical skills necessary for the performance of more complex surgical procedures in Orthopedic surgery Establish a knowledge base, judgement and interpersonal skills necessary to function as a surgical consultant Teach junior residents in the emergency room, wards, and operating room Competently manage a house-staff team in the peri-operative care of the patient Work with the attending physician on development of post-operative plan Master the details of pre-operative preparation of a hospitalized patient or an outpatient Demonstrate the personal and professional responsibility, leadership skills, and interpersonal skills necessary for independent practice as an Orthopedic surgeon PGY-4 skills Master technical skills necessary for the performance of more complex surgical procedures in Orthopedic surgery Provide clinical and administrative leadership for residents and students assigned to surgical services Act as a mentor for junior surgical residents Learn more advanced surgical techniques PGY-5 skills Continue to master technical skills necessary for the performance of all surgeries Achieve the full competence (including knowledge, skills, and attitudes) of a board eligible surgeon Function as faculty Page 17