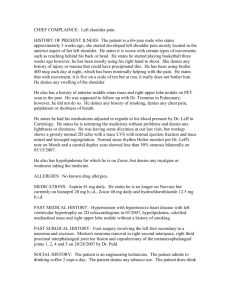
Name: John C. MRN: 123456 DOB: 07/25/1965 Age: 47 CC: New
advertisement

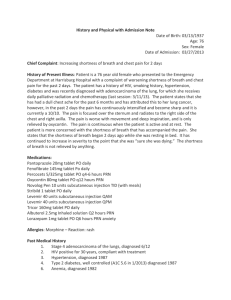
Name: John C. MRN: 123456 DOB: 07/25/1965 Age: 47 CC: New Patient/Initial Wellness Visit HPI: Mr. C is a 47 year old male with a history of HTN, hyperlipidemia, thoracic aortic aneurysm and depression. He presents to the office as a new patient and for an initial wellness visit. Mr. C states he is primarily concerned about his long term hypertension, which continues to be poorly controlled with his current medication regimen. He states that when his blood pressure gets “really high” he “doesn’t feel right” and develops a headache with dizziness, for which he has previously visited the ER at Jersey Shore hospital twice and undergone rapid reduction of his hypertension. Mr. C does not have records of his ER visits with him today and states that his last visit was “a couple of months ago”. Mr. C also states he has an aortic aneurysm “in his chest” which has been previously monitored, but has not been reevaluated in in the last two years. Today, Mr. C states that he feels “fine” and denies having a headache or dizziness. Additionally Mr. C denies experiencing any chest pain, SOB, palpitations, peripheral edema, nausea, vomiting, changes in vision or coughing. Mr. C states that he has had high blood pressure for 3-4 years, which he attributes to a diet that consists primarily of “nicotine and caffeine”. Other than continuing to experience some insomnia and increased fatigue, he has no complaints. Mr. C denies experiencing any pain currently. PMH: Medications: Benicar 40mg PO Q daily Lisinopril 10mg PO daily Paroxetine 20mg PO Q daily Atorvastatin 10mg PO QHS Vitamins: None Herbals: None Allergies: Latex Sensitivity (rash) Immunizations: Current Surgical Procedures: None Hospitalizations: No admissions, two visits to ER in last year secondary to hypertensive urgencies Trauma: Fall from ladder (1992) with fracture to right ankle Illnesses: HTN diagnosed “3-4 years ago”, patient states that it has never been well controlled, despite medication. Diagnosed with depression 2 years ago, at which point he was started on paroxetine. Mr. C states he continues to feel fatigued and have insomnia several days a week. Started on atorvastatin approximately one year ago for hyperlipidemia. No records available for evaluation of patient’s thoracic aortic aneurysm. Family History: Father: Died of “heart disease” at 72 Mother: Died of “heart disease” at 81 Brother: Alive and well, HTN, 44 years old Son: Alive and well, 18 years old Patient denies a family history of diabetes mellitus, cerebrovascular issues, bleeding disorders, cancer and known history of aortic aneurysms. Social History: Mr. C works at a local construction company in waste water treatment. He is married and lives with his family locally. He smokes approximately 20 cigars daily and drinks 1-2 beers a month. He also drinks on 4-6 caffeinated beverages daily. Denies use of illicit drugs. Mr. N does not exercise regularly. ROS: General: Gets “lightheaded” when his blood pressure is high. Also feels fatigued most days, despite getting 7 hours of sleep. Denies weight gain/loss in last year, loss of appetite, fatigue, fever, chills, or night sweats Skin: Denies rashes, pruritus, ecchymosis, lesions, or erythema Head: Headaches occasionally, including prior to his trips to the ED. Denies history of trauma to head, bumps or lesions Eyes: Denied changes in vision, blurred vision, diplopia, itching or sensitivity to light; Wears glasses, however last eye exam was approximately two years ago. Ears: Denies changes in hearing, tinnitus, infections or vertigo Nose: Denies changes or loss of sense of smell, rhinorrhea, congestion, or sinus infections Throat: Denies bleeding of gums, dry mouth, lesions or ulcers in mouth Neck: Denies pain or stiffness of neck; Denies history of thyroid issues or enlarged lymph nodes Pulmonary: Denies cough, sputum production, shortness of breath, wheezing or hemoptysis Cardiovascular: Denies chest pain, palpitations, angina, dyspnea on exertion, or claudication GI: Denies dysphagia, reflux, decrease in appetite, nausea, vomiting, hematemesis, diarrhea, constipation, hematochezia, or melena Endocrine: Denies heat/cold intolerance, polyuria, polydipsia, or polyphagia Neurological: Denies history of seizures, weakness, paralysis, numbness, previous CVA or tingling Genitourinary: Denies increased frequency, urgency, incontinence, dysuria, hematuria, or history of UTIs Musculoskeletal: Occasionally experiences low back pain. Denies current musculoskeletal/joint pain, joint swelling, or arthritis Hematology: Denies history of anemia, easy bruising or bleeding Psychiatric: Diagnosed with depression in 2011, currently denies feeling depressed. Denies history of anxiety, nervousness, illicit substance abuse or memory problems Physical Exam: General: Pleasant affect and cooperative throughout interview/exam; Appears to be in no acute distress and is alert and orientated to person, place and time Vital Signs: Temp: 98.1F (tympanic) Respirations: 20 HR: 72 BP: 180/110 (repeated with electric cuff: 191/118) Height: 72 inches Weight: 108 kg BMI: 32.3 Skin: Warm, dry, pink. No cyanosis/clubbing of nails. Nodes: No cervical, submandibular, supraclavicular, infraclavicular or axillary lymphadenopathy Head: Normocephalic, non-tender; No masses, lacerations, or lesions Eyes: PERRLA; Visual acuity: Right eye20/40 Left eye 20/25 without correction, 20/20 with glasses; EOMI; Conjunctiva and sclera clear; No ptosis noted; No papilledema/AV nicking/cotton wool spots; Cup-to-disc ratio 1:3 Ears: No hearing loss detected; tympanic membranes non-erythematous with equal mobility Nose: Symmetrical with no lesions, obstruction, inflammation or exudate noted; Frontal, maxillary and ethmoid sinuses non-tender Throat: Gums erythematous, no active bleeding noted; Multiple caries noted; No lesions, ulcers, or exudate of tongue or pharynx; Tonsils present and equal bilaterally; Moist mucous membranes; No deviation of the tongue; No lesions, masses or loss of ROM; Uvula symmetrical and non-erythematous Neck: Supple; Trachea is midline; Non-tender; No masses, carotid bruits, JVD, lesions or edema Chest/Lungs: Lungs clear to auscultation bilaterally; Non-labored breathing; Symmetrical chest expansion; No wheezing/rales/rhonchi/stridor Heart: Regular rate and rhythm; S1 and S2 appreciated; no murmurs/ rubs/thrills; No peripheral edema Abdomen: Obese; Soft, non-tender; No ecchymosis, striae, or bruits; Normoactive bowel sounds x 4; No organomegaly Rectal: Deferred by preceptor. Would assess for: Equal and concentric rectal tone; Appropriate prostate size, with no masses/tenderness Musculoskeletal: No deformities/ecchymosis/edema. Capillary refill two seconds in upper and lower extremities Peripheral Vascular: Radial, Posterior Tibial and Dorsalis Pedis pulses present and equal bilaterally, +2/4 Neurologic: CN II: Visual acuity: Right eye 20/40 Left eye 20/25 without correction, 20/20 with corrective glasses; Visual fields intact CN III, IV, VI: EOMI; no ptosis or nystagmius noted CN V: Facial sensation intact to light palpation; Masseter and temporalis muscles intact, with full ROM CN VII: Patient raises eyebrows equally, can close eyelids tightly, smile, and frown CN IX, X: Palate moves midline and superiorly and patient able to swallow; Uvula symmetrical and rises equally with swallowing CN XI: Able to shrug shoulders and rotate neck against resistance CN XII: Tongue movement is symmetrical with strength against resistance Mental Status: Orientated to person, place and time; Appropriate affect and mood; No dysarthria Additional mental status exam deferred. Additional testing to be evaluated include: Abstract reasoning via proverb; Able to read and write sentence; Awareness of current events, follows simple commands; Long term memory tested by recollection of past presidents and news events; Three object recall used to test short term memory Assessment: 1) 2) 3) 4) 5) 6) Uncontrolled Hypertension Thoracic Aortic Aneurysm Hyperlipidemia Depression Obesity Tobacco Abuse Additional Testing Ordered: CBC, CMP, TSH Additional Studies Ordered: Chest CT with contrast for evaluation of aneurysm Medication Changes: Discontinue Benicar and Paroxetine Start Azor 10/40mg PO Q daily Start Aspirin 81mg PO Q daily Start Cymbalta 60mg PO Q daily Plan: Mr. C’s history of very poorly controlled hypertension is concerning and we discussed for 30 minutes with the patient various ways to improve his hypertension and overall health. Discontinued patient’s Benicar and started on Azor 10/40mg. If he does not benefit from this medication, would consider switching to Tribenzor in the future for additional control. Strongly encouraged Mr. C to stop smoking, as it can contribute to his hypertension, progression of his thoracic aortic aneurysm and increases his risk of cancer and COPD. At this point, Mr. C stated that he would try to cut down on smoking. Mr. C is scheduled for a chest CT for evaluation of his thoracic aortic aneurysm. Discussed the warning signs he should be aware of concerning his aneurysm, including sharp, sudden chest and/or back pain. Discussed with Mr. C the importance of improving his diet by eating more fruits and vegetables and decreasing his consumption of caffeine products. Also encouraged Mr. C to increase his daily exercise as this will help him control his obesity. He is also scheduled for a CBC, BMP and TSH to establish his baseline bloodwork and evaluate his hyperlipidemia as well as possible secondary causes of his hypertension. Due to Mr. C’s increased fatigue and insomnia, his Paroxetine was discontinued and he was switched to Cymbalta 60mg. He was advised to contact the office or seek immediate medical attention if he experiences any adverse reactions to his changes in medications. These symptoms could include facial/body swelling, difficulty breathing and skin rashes/hives. Mr. C is scheduled for a follow up appointment in 2 weeks at which time the results of his bloodwork and imaging studies should be available for review. Mr. C was amiable to this course of action and denied any further questions. Vanessa G. Wittstruck, PA-S 4/05/13 17:54