Christie E. Slottje, PA-S
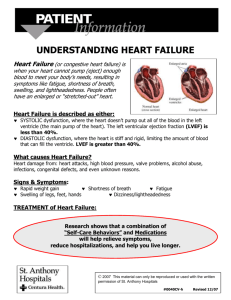
advertisement

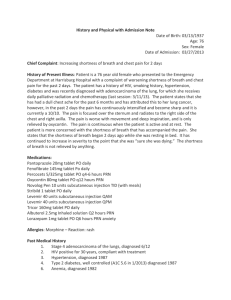
History and Physical with Admission Note Date of Birth: 06/13/1945 Age: 67 Sex: Female Date of Admission: 10/02/2012 Chief Complaint: Increasing shortness of breath x 3 days History of Present Illness: Patient is a 67-year old female with a history of advanced terminal COPD. She began having increasing shortness of breath since Friday, but did not seek medical care. The shortness of breath kept getting worse and she began to develop a dry cough Monday night. She used her Advair inhaler with minimal relief. Today, her shortness of breath continued to advance to the point that she called the ambulance. When EMS arrived her O2 saturation was 84% on room air. When she arrived in the emergency department she was hypoxic and in respiratory distress. She was put on a CPAP and taken to her emergency room and seen by the emergency room physician. She was treated with SoluMedrol and SVN treatment. Following treatment, she was still short of breath. Upon examination significantly diminished air movement was noted. Attending physician was then called to admit patient. The patient has been seen multiple times for episodes of COPD exacerbations. She has been instructed to seek medical care when increase shortness of breath is first noticed, but she has been non-compliant. Pertinent Past Medical History 1. Terminal COPD 2. History of recurrent bronchitis 3. History of respiratory failure 4. Smoking: She has been instructed many times to quit, however does not. Pertinent Family History: Father passed at the age of 75 of heart failure Pertinent Social History Patient has a significantly positive history for tobacco use. Patient claims to smoke 1 pack per day for past 40 years. Patient denies alcohol or illicit drug use. Patient does not attempt to exercise, and it is thought that she rarely leaves her apartment. Medications: Advair 115/21 inhaler, 2 puffs BID Tylenol 325mg, 2 tablets every 6 hours as needed for occasional headaches Allergies: Patient denies any known allergies. Review of Systems: General: Patient denies weight or appetite change, fever, chills, night sweats, or fatigue Head: Occasional headaches-unchanged in years, denies trauma, or changes in vision or hearing Skin: Patient denies any changes in skin, hair or nails, also denies any rashes or itching Eyes: Patient states that she does occasionally get dry eyes, attributing it to pollution from the road coming into the window of her apartment. Patient does not wear glasses or contacts, has had no blurring or decrease of visual acuity Ears: Patient states she believes she has occasional vertigo, however has never sought out medical care for this. Patient does not wear hearing aid and has not experienced hearing loss or ringing in ears Nose: Patient claims to have constant “runny nose,” denies sneezing or allergies Mouth, Throat, Neck: Patient denies sore throat, lesions in mouth, hoarseness or lumps or swelling of neck Cardiovascular: Patient denies chest pain, tightness, palpitations Respiratory: Positive for terminal COPD, multiple admissions for bronchitis and respiratory failure. Patient claims to have constant shortness of breath, increasing with walking or bending over. Gastrointestinal: Negative for abdominal pain, nausea, vomiting, diarrhea, and constipation Genitourinary: Patient denies pain with urination, blood in urination, history of urinary tract infections or kidney stones Central Nervous System: Negative for stroke, TIA, dizziness, or syncope Musculoskeletal: Patient denies weakness, decrease in muscle strength, difficulty walking Extremities: Negative for numbness, tingling, decreased strength or sensation Hematological: Patient denies history of DVT, PE, knowledge of bleeding or clotting disorder, or bruising easily Medical History Childhood: Patient denies any childhood illnesses, uncertain if she had chicken pox Adult Immunizations: Patient has not received flu vaccine this year, has previously received pneumonia (9/2010) vaccine or shingles (11/2011) vaccine Past Medical History: 1. Terminal COPD 2. History of recurrent bronchitis 3. History of respiratory failure 4. Hypertension 5. Hyperlipidemia 6. Smoking Hospitalization History: 1. Birth of 9 children 2. For all surgical procedures (see surgical history) 3. Admitted 3 times for CODP exacerbations/Bronchitis, all within last 7 years Surgical History: 1. Laparoscopic Cholecystectomy: 1996 2. Hysterectomy : 1991 3. Surgical knee repair: 1979 Family History: 1. Mother: deceased, uterine cancer 2. Father: deceased, heart failure 3. Siblings: 2 brothers, does no communicate with, last heard they were in good health 4. Children: Patient has 9 children, one deceased from auto accident, otherwise all alive and in good health. Social/Psychiatric History: She lives alone and claims to have distanced herself from the majority of her family. She believes the trouble with her family is related to the decisions she has made regarding her health and life style Patient claims that she has had trouble with anxiety and depression in the past, but she has never been treated medically. Patient also admits to 4-6 caffeinated drinks per day. Physical Examination Vitals: Blood Pressure: 123/92, Pulse 127, Respirations: 28, O2 saturation: was 84% on room air when EMS arrived at home, after SVN treatment and 2L oxygen via nasal cannula improved to 96% General: The patient is awake, alert, orientated, and appears to be in moderate distress, lying in bed Skin: Warm and dry, no scars, rashes, or bruises Head: Atraumtic and normocephalic Eyes: Pupils are equal and reactive to light, extraocular muscles intact Mouth: Poor dental hygiene, few teeth remaining, no bleeding or ulcers Neck: No tracheal deviation, no masses detected on thyroid, no lymphedema Chest: Increased AP diameter Breast: No changes in color, symmetry, lumps or tenderness Lungs: Significantly diminished breath sounds bilaterally with diminished air entry. Minimal expiatory wheezing detected Heart: Negative for rubs, gallops, clicks, or murmurs, regular rhythm, S1 and S2 detected, tachycardia Abdomen: Soft, positive bowel sounds x4, non-tender, no organomegaly Extremities: No edema or cyanosis, no calf tenderness Peripheral Vascular: Varicose veins observed on lateral thighs. Carotid, radial, posterior tibial, and dorsalis pedis all +2 and equal bilaterally Neurological: Patient awake, alert, and oriented, no focal deficient detected. Assessment: 1. Acute COPD exacerbation 2. Bronchitis 3. Pneumonia 4. Common cold/flu symptoms 5. Congestive Heart Failure 6. Lobar Atelectasis Plan: Admit the patient to the medical floor. See admission note. Christie E. Slottje, PA-S Christie E. Slottje, PA-S 10/2/2012 9:15 am Admission orders Patient Name: xxxxxxxxxxx DOB: 06/13/1945 Sex: Female Admit to: Medical Floor, Lock Have Hospital Admitting Physician: Dr. Raj Patel Diagnosis: Shortness of breath with cough, advanced terminal COPD Condition: Stable Vital Signs: Blood pressure, pulse, respirations, O2 saturation, and temperature every 6 hours Activity: As tolerated Nursing Care: Oxygen: 2L nasal cannula, titrate to keep O2 saturation above 92% Weight on admission, then everyday at same time Diet: low salt, low fat diet Ins & Outs: NSS with 10KCl at 100 cc/hour Studies: Check that all studies were completed as ordered in Emergency Department Blood cultures and sensitive Sputum cultures and sensitivity Medications: Home medications: 1. Advair 115/21 inhaler, 2 puffs BID 2. Tylenol 325mg, 2 tablets every 6 hours as needed for occasional headaches Given in ER: 1. Solu-Medrol 2. SVN treatment Medications on Floor: 1. Continue Home medications 2. Solumedol 60mg IV q 6 hours 3. Levaquin 60mg IV q 4 hours 4. Duoneb q 6 hours Allergies: NKA Lines: established #16 in right hand Special Instructions: none Christie E. Slottje, PA-S Christie E. Slottje, PA-S 10/2/2012 9:15 am